Abstract
Only 20–30% out of the treated hypertensive patients in Europe are achieving blood pressure (BP) control. Among other recognized factors, these poor results could be attributable to the fact that for many doctors it is very difficult to detect which is the predominant hemodynamic cause of the hypertension (hypervolemia, hyperinotropy or vasoconstriction). The aim of the study was to use non-invasive thoracic electrical bioimpedance (TEB) to evaluate hemodynamic modulators and subsequent hemodynamic status in uncontrolled hypertensive patients, receiving at least two antihypertensive drugs. A number of 134 uncontrolled hypertensive patients with essential hypertension were evaluated in nine European Hypertension Excellence centers by means of TEB (the HOTMAN® System). Baseline office systolic and diastolic BP averaged 156/92 mmHg. Hemodynamic measurements show that almost all patients (98.5%) presented at least one altered hemodynamic modulator: intravascular hypervolemia (96.4%) and/or hypoinotropy (42.5%) and/or vasoconstriction (49.3%). Eleven combinations of hemodynamic modulators were present in the study population, the most common being concomitant hypervolemia, hypoinotropy and vasoconstriction in 51(38%) patients. Six different hemodynamic states (pairs of mean arterial pressure and stroke index) were found. Data suggest that there is a strong relation between hypertension and abnormal hemodynamic modulators. This method might be helpful for treatment individualization of hypertensive patients.
Introduction
Despite the clear benefits of numerous classes of antihypertensive therapy, hypertension remains poorly controlled in clinical practice and blood pressure (BP) control of hypertensive patients remains a major unsolved problem in Europe (Citation1,Citation2). This has significant implications for public health, because low BP control has been shown to be associated with a marked increase in the risk of fatal and non-fatal cardiovascular (CV) events (Citation3,Citation4). Antihypertensive agents reduce morbidity and mortality associated with hypertension through BP control. Studies have indicated that even small reductions in systolic or diastolic BP result in 30% and 40% reductions in the risk of ischemic heart disease and fatal stroke, respectively (Citation5).
According to current recommendation, five major classes of antihypertensive agents [thiazide diuretics, calcium antagonists, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor antagonists and beta-blockers] are suitable for the initiation and maintenance of antihypertensive treatment, alone or in combination (Citation6). Choice of antihypertensive drugs is made considering previous experience with the drug, effect of drugs on CV risk factors, presence of specific disease or disorders, and drug cost, among others. The reasons why hypertension is poorly controlled include inadequate or suboptimal antihypertensive medication, medication intolerance, patient non-compliance, underestimation of comorbidities, physician perceptions about drug effectiveness, medication cost, etc. All guidelines for the management of hypertension emphasize the need to improve long-term CV outcomes as well as to increase the proportion of patients achieving target BP (Citation6), without providing a specific algorithm.
Hypertension is a multifactorial disease, but the hemodynamic component of BP physiology includes factors that affect intravascular volume, cardiac inotropy and systemic vascular resistance. Usually, physicians do not have the possibility of evaluating the hemodynamic causes of the hypertension – hypervolemia, hyperinotropy or vasoconstriction – or whether there is a combination of these causes. For this reason, the BP problem is treated like a symptom, without paying attention to the hemodynamic causes of BP elevation, and the selection of antihypertensive agents is often done independently of the hemodynamic status of the patient. When the pharmacological class of antihypertensive agent does not correspond to the hemodynamic state, BP reduction is limited. By contrast, when the pharmacological class of antihypertensive treatment is adapted to the hemodynamic state [for instance diuretics for hypervolemia, or calcium-channel blocker/ACE inhibitor/angiotensin receptor blockers (CCB/ACEI/ARB) for increased peripheral resistances], BP reduction may occur more rapidly and to a greater extent (Citation7–10).
The study purpose was to assess hemodynamic modulators (intravascular volemia, inotropy and vasoactivity) and hemodynamic status [mean arterial pressure (MAP) and stroke index (SI)] in uncontrolled hypertensive patients using a non-invasive thoracic electrical bioimpedance (TEB) technique (the HOTMAN System®, Hemo Sapiens Inc.) and possible relationship between uncontrolled hypertension and untargeted hemodynamic modulators.
Materials and methods
A clinical evaluation was conducted in nine European Hypertension Excellence Centers over a period of 2 months, using a common standardized procedure. Centers included 134 uncontrolled hypertensive patients with essential hypertension treated with at least two antihypertensive drugs. According to the protocol, any patient meeting inclusion and exclusion criteria attended each Center of Hypertension over the study period was chosen to be evaluated. All patients were already following an antihypertensive treatment, but were not controlled under the previous medication (BP values > 140/90 mmHg clinically and > 130/80 mmHg average of 24 h on ambulatory BP monitoring). Office BP was taken in concordance with “2007 ESH Guidelines for the management of arterial hypertension”, with the patient seated using an oscillometric method.
We implemented the HOTMAN® System (Hemo Sapiens Inc.), a computer operating device based on TEB for providing non-invasive assessment of hemodynamic modulators and evaluation of the hemodynamic status of the patients. TEB measurement was obtained as a part of routine care. Hemodynamic parameters were achieved in supine patients after 10 min of rest. The TEB technique belongs to impedance cardiography (ICG), a non-invasive hemodynamic diagnostic and monitoring technology. ICG has demonstrated its usefulness and reproducibility in various populations (Citation11–14).
The principle of TEB is based on measuring the thorax impedance (resistance of body tissues) when is applied an alternating current with a very low intensity and high frequency. The measurement current passes between two pairs of TEB sensors located on the upper neck and upper abdomen in a direction parallel to the spine. Four other receptor sensors are located at the root of the neck and at the diaphragm level. These sensors detect ECG signals as well as the voltage of the electrical current that crosses the thorax, which is proportional to the thoracic impedance (Citation15). HOTMAN System functioning is based on a proprietary very low TEB technology, utilizing very low TEB measurement current with fully digitized, high sampling rate generation and acquisition of the TEB signal. The TEB measurement current is only 7 μA, safe for the patients and with high reproducibility. Its digital data processing results in wide bandwidth, high-quality and high-resolution TEB signal, unavailable with analogue acquisition methodologies.
These features enable precise measurements of TEB signal’s key magnitude and timing events. Following the digital process of TEB and ECG signal, this technique provides information about the value of blood flow [cardiac index (CI) and SI, heart rate (HR)], contractility and left ventricle performance [ejection phase contractility index (EPCI), inotropic state index (ISI) and left stroke work index (LSWI)] and afterload [stroke systemic vascular resistance index (SSVRI), and thoracic fluid conductivity (TFC)].
Compared with the classical ICG technique, the HOTMAN® System has some different characteristics: it measures systemic vascular resistance per beat as SSVRI, a parameter not detected by other bioimpedance devices; it is the only system that offers a beat-to-beat evaluation of cardiac inotropy (ISI); and intravascular volume is not evaluated through TFC, but calculated as a component of total contractility according to the Frank–Sterling Law. In addition, the HOTMAN® System presents the hemodynamic status of the patient and the situation of the hemodynamic modulators: volemia, inotropy, vasoactivity and chronotropy (Citation16).
Statistical analysis
For every patient, the percent deviations of the hemodynamic modulators from its ideal values were calculated. Data were recorded in a computer database using Excel software from the HOTMAN System's printed status report.
Results
One hundred and thirty-four patients with essential hypertension were evaluated. All subjects followed antihypertensive therapy for more than 2 months and presented documented history of uncontrolled BP. During the study, office systolic and diastolic BP averaged 156/91.9 mmHg; 110 subjects (82.1%) had BP level above normal values and 24 (17.9%) patients exhibited normal BP. None of the patients with normal BP value had this value < 120/80 mmHg. BP during hemodynamic measurements and hemodynamic parameter in study group are presented in . No demographic data were collected during the study.
Table I. Blood pressure and hemodynamic parameters in the study group.
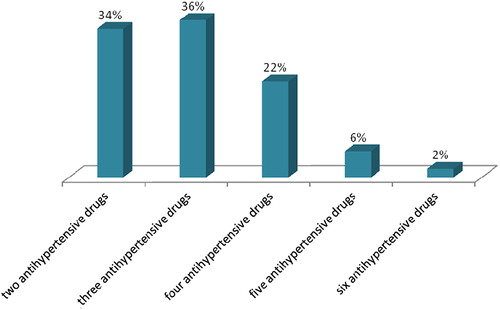
Patients included in the study took an average of 3.06 ± 1 antihypertensive medications belonging to five major classes of antihypertensive agents recommended by 2007 ESH/ESC Guidelines – thiazide diuretics, calcium antagonists, ACE inhibitors, angiotensin receptor antagonists and beta-blockers – alone or in combination. Only 11 (8.1%) patients were treated with centrally acting agents and six (2.2%) patients treated with six antihypertensive medications. The vast majority of patients received two or three antihypertensive drugs – 46 (34.3%) and 48 (35.8%), respectively – followed by a four-drug regimen – 29 (21.7%) ().
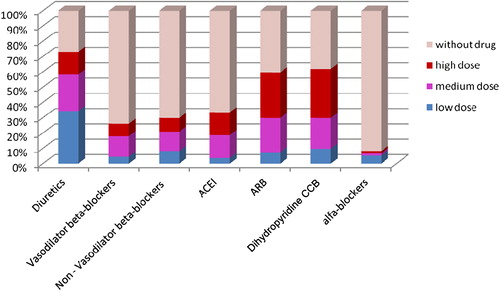
Diuretics were the most used antihypertensive drugs and were prescribed in 71.6% of the study population. The next used antihypertensive drugs were dihydropyridine CCBs (61.9%) and ARBs (56.7%). Beta-blockers were divided in two categories – vasodilator beta-blockers and non-vasodilator beta-blockers – and they were prescribed in 24.6% and 29.8% of patients, respectively. ACE inhibitors were used in 32.8% patients and central acting drugs in 8.1%. Each antihypertensive class was split from dosage point of view in low dose, medium dose and high dose ().
Among the whole study group, 70 (52.2%) patients were diagnosed as normodynamic (SI in normal range: 35–65 ml/m2), 36 (26.9%) as hypodynamic (SI < 35 ml/m2) and 28 (20.9%) as hyperdynamic (SI > 65 ml/m2) (). Hemodynamic state is defined by MAP and blood flow (SI) over one heartbeat interval. During non-invasive hemodynamic assessment, six different hemodynamic states were found: hypertension and hypodynamic in 30 (22.4%) patients, hypertension and normodynamic in 54 (40.3%) patients, hypertension and hyperdynamic in 18 (13.4%) patients, normotension and hypodynamic in six (4.5%) patients, normotension and normodynamic in 16 (11.9%) patients and normotension and hyperdynamic in 10 (7.5%) patients ().
Figure 3. Scattergram of hemodynamic state of all patients measured in the study with superimposed percentage of correspondent hemodynamic states.
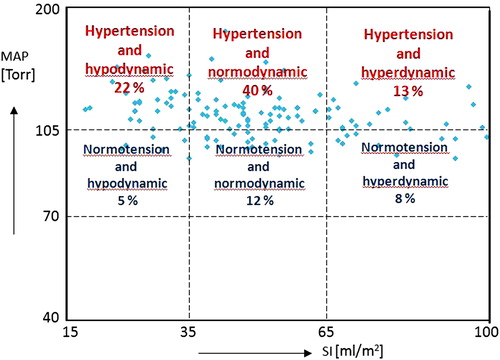
From these six hemodynamic states, hypertension occurred in more than 76% of patients and less than 12% reached the hemodynamic goal, being simultaneously normotension and normodynamic.
Hypertension in any individual is caused by its specific and unique contribution of abnormal levels in hemodynamic modulators. Hemodynamic measurements revealed that most of patients presented intravascular hypervolemia (96.4%), and/or hypoinotropy (42.5%) and/or vasoconstriction (49.3%).
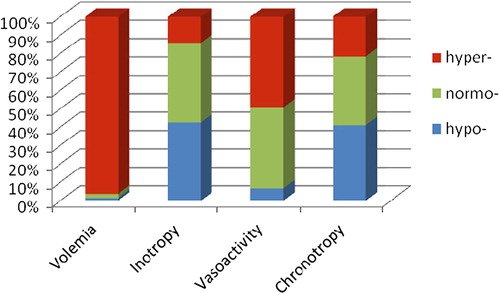
The initial hemodynamic assessment showed the following distribution of the hemodynamic modulators (intravascular volemia, inotropy and vasoactivity), including chronotropy: hypovolemia two (1.5%) patients, normovolemia three (2.2%) patients, hypervolemia 129 (96.3%) patients, hypoinotropy 57 (42.5%) patients, normoinotropy 58 (43.3%) patients, hyperinotropy 19 (14.2%) patients, vasodilation nine (6.7%) patients, normovasoactivity 59 (44%) patients, vasoconstriction 66 (49.3%) patients, hypochronotropy 55 (41%) patients, normochronotropy 50 (37.4%) patients and hyperchronotropy 29 (21.6%) patients ().
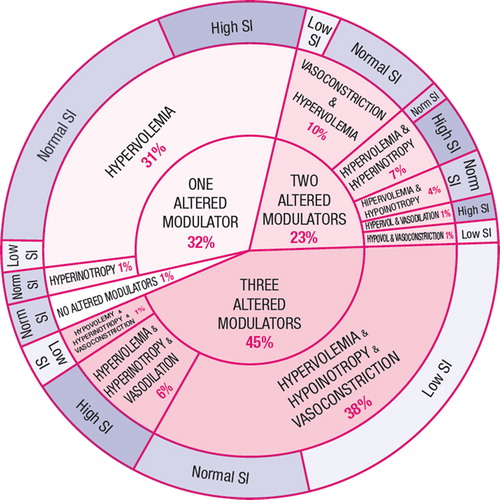
An abnormal hemodynamic state is a result of abnormal levels in one or a combination of hemodynamic modulators. Since any single abnormal hemodynamic modulator (intravascular volume, inotropy and vasoactivity) might be responsible for a hemodynamic disturbance, we divided the study population into four subgroups according to number of altered hemodynamic modulators: (i) all three hemodynamic modulators altered (44.8%), (ii) a combination of two altered hemodynamic modulators (22.4%), (iii) one hemodynamic modulators altered (31.3%), and (iv) no hemodynamic modulators altered (1.5%) ().
The subgroup of patients with three altered hemodynamic modulators was the most numerous (44.8%) in the study population. This subgroup included three different combinations of altered modulators, as shows. In fact, the patients with concomitant hypervolemia+ hypoinotropy+ vasoconstriction represent the biggest homogenous population in the study group. Despite a similar combination of altered modulators, 34 patients in this group were hypodynamic (low SI value) and 17 patients normodynamic. shows the complete hemodynamic profile and antihypertensive drug treatment in all subgroups.
Table II. Complete hemodynamic profile and drug distribution in each subgroup.
A combination of two altered hemodynamic modulators was met in 30 (22.4%) patients and contains five pairs of different altered hemodynamic modulators: hypervolemia+ vasoconstriction, hypervolemia+ hyperinotropy, hypervolemia+ hypoinotropy, hypervolemia+ vasodilation and hypovolemia+ vasoconstriction.
Almost one third of total study patients (31.3%) belonged to the subgroup with one hemodynamic modulator altered. With one exception, this altered hemodynamic modulator was hypervolemia. Again, SI values varied broadly despite similar hemodynamic modulator altered (). Only two patients exhibited normal values for all hemodynamic modulators. This is an interesting finding considering a total of 24 patients with normal BP, because the remaining 22 patients presented normal BP but abnormal hemodynamic profile.
Discussion
BP is a measurable end product of an exceedingly complex series of factors including those that control blood vessel caliber and responsiveness, those which control fluid volume within and outside the vascular bed, and those which control cardiac output. None of these factors is independent: they interact with each other and respond to changes in BP (Citation17). Effective control of BP, may, potentially, be obtained from changes in lifestyle, adequate therapeutic management and compliance to treatment. The main improvements could rise from maximizing the effective use of existing therapeutic strategies and development of new approaches in hypertension management.
In numerous clinical trials, BP control is achieved in one third of patients with monotherapy, even under strict trial conditions. Different classes of antihypertensive agents, when combined, often have better antihypertensive effect than a single one due to synergistic effects and may have better tolerability when two components minimize each other's side-effects. Combination therapy is initiated when monotherapy fails, there is a high CV risk, high BP levels or subclinical organ damage is present (renal, CV damage) (6).
There are a number of likely combinations of drug therapy for hypertension from which the physician can choose, but there is no single optimal treatment for everyone with hypertension. It was noticed that the percentage of patients responsive to any drug class is limited and patients responsive to one drug are often not those responsive to another drug (6).
One major problem that should be reconsidered in the treatment of hypertensive patients is the use of drugs at the correct and most effective dosages. Another problem is that BP elevation is treated like a symptom, without paying attention to the hemodynamic causes. Physicians mainly neglect the other hemodynamic parameters like cardiac output, left ventricle contractility and vascular resistance, despite the fact that used drugs are modifying the entire hemodynamic status. This could be an explanation for the relatively low BP control rates and important associated side-effects.
The primary function of our CV system is not a generation of BP but a delivery of oxygen to all tissues. Oxygen delivery is a phenomenon related to the blood flow and not to BP. Actually, an adequate delivery of oxygen to all organs under all metabolic conditions is the true definition of CV health. In this respect, cardiac output is the ultimate expression of CV performance (Citation18).
A healthy CV system maintains adequate supply of oxygen to all tissues under all metabolic conditions by a dynamic variation of levels of four modulators. Three of them are the systemic hemodynamic modulators (intravascular volume, inotropy and vasoactivity) and one is the perfusion flow modulator (chronotropy) (Citation19,Citation20). The body changes the levels of these four modulators for every heartbeat in response to a varying oxygen demand of all tissues (Citation21).
It was proven that adequate oxygen delivery is the primary determinant in survival of high-risk, critically ill patients (Citation22,Citation23). For hypertensive patients, it is much harder for clinicians to evaluate hemodynamic modulators in the absence of specific evidence. Physician perceptions and patient symptoms are examples of barriers affecting the management and control of hypertension (Citation24). Under these conditions, it is a challenging task for the clinician to determine the optimal therapeutic combination of medications for each patient, mainly uncontrolled but compliant to hypertensive treatment. What is a correct drug and/or drug combination for one patient may be totally inappropriate therapy for another.
Regardless of the therapeutic availabilities of the last few years in the field of hypertension, at the enrollment in our study, the BP of patients who were taking at least two or more antihypertensive drugs was not well controlled. The study population shared six hemodynamic states (pairs of MAP and SI) with different needs in term of treatment in order to achieve the goal of normotension and normodynamism. This situation reflected the total contribution of actual treatment over MAP (76% still exhibiting hypertension) and SI.
Similarly to other studies involving hemodynamic assessment of hypertension (Citation7,Citation9,Citation10), 96.3% of patients present hypervolemia in the absence of edema or other clinical signs of volemic overload. This can be the result of real hypervolemia but also hemodynamic compensatory effect of hypoinotropic patients, since about 40% of patient present simultaneously hypoinotropy. Anyhow, our results indicate that more intensive diuretic therapy is required in about half of the uncontrolled hypertensive patients in this study compared with the empiric selection of drugs (diuretics were used by 71.6% of patients). The issue of unidentified volume expansion is well recognized as a cause for resistance to antihypertensive therapy (Citation25).
Also, considering the number of patients exhibiting hypoinotropy (42.5%), the dosage and/or usage of drugs with negative inotropic mechanism should be reassessed. This suggestion is furthermore sustained by the presence of 41% of patients with hypochronotropy, a possible result of the negative chronotropic effect of beta-blockers.
A significant percentage of patients (49.3%) presented increased peripheral vascular resistance. Vasoconstriction is hard to assess in current practice. These results confirm the known pathophysiology of hypertension and the association between elevated pressures and high peripheral resistance, regardless of the primary etiology. Interestingly, vasoconstriction was present despite the aggressive usage of vasodilating drugs (ACEI, ARB and dihydropyridine CCB): almost the entire population included in the study was treated with at least one vasodilating drug in different dosages – another suggestion that selection of an optimal combination of medications for the uncontrolled hypertensive patient is often empiric.
Different combinations of altered hemodynamic modulators were met in study subjects. Only two patients exhibit concomitant normal values for hemodynamic modulators. Our study provided information to confirm an important variation of hemodynamic modulators, which defined the hemodynamic profile in hypertensive patients. Comparing hemodynamic modulators in different uncontrolled hypertensive patients, a major discrepancy was noticed in term of number (from none to all abnormal hemodynamic modulators) and degree of alteration. In a prospective study, the selection of therapeutic agents based on the hemodynamic profile specific to each patient provided by TEB hemodynamic measurements led to a better control of hypertension in 84% of the studied population (Citation10). Thoracic bioimpedance provides the clinician with reliable hemodynamic information that could only previously be obtained in the critical care unit of a hospital using a pulmonary artery catheter. Implementation of this hemodynamic information aids in identifying the hemodynamic components of hypertension, allowing the initiation and titration of medications that act more effectively.
In conclusion, our data suggest a strong relation between hypertension and abnormal hemodynamic modulators, with significant individual variation of the hemodynamic profile. Careful analysis of all hemodynamic modulators could precede pharmacological treatment modification in order to achieve a normohemodynamic status. Non-invasive hemodynamic measurements with TEB characterize hemodynamic profile and may be helpful for diagnostic and prognostic purposes, and for therapeutic decision making in hypertensive patients. The clinical benefits potentially offered by a greater use of this technique in the daily management of patients would require testing by future longitudinal outcome studies.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
This study was supported by the European Union through the European regional Development Fund.
References
- Graham I, Atar D, Borch-Johnsen K, Boysen G, Burell G, Cifkova R, et al. European guidelines on cardiovascular disease prevention in clinical practice: Executive summary. Eur Heart J. 2007;28:2375–2414.
- Grassi G, Cifkova R, Laurent S, Narkiewicz K, Redon J, Farsang C, et al. Blood pressure control and cardiovascular risk profile in hypertensive patients from central and eastern European countries: Results of the BP-CARE study. Eur Heart J. 2011;32:218–225.
- Almgren T, Persson B, Wilhelmsen L, Rosengren A, Andersson OK. Stroke and coronary heart disease in treated hypertension – A prospective cohort study over three decades. J Intern Med. 2005;257:496–502.
- Ezzati M, Oza S, Danaei G, Murray CJ. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117:905–914.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913.
- Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G. 2007 ESH–ESC Practice Guidelines for the Management of Arterial Hypertension: ESH–ESC Task Force on the Management of Arterial Hypertension. Eur Heart J. 2007;28:1462–1536.
- Smith R, Levy P, Ferrario C. Efficacy of noninvasive hemodynamic monitoring to target reduction of blood pressure levels (CONTROL). Am J Hypertens. 2005:18:94A.
- Sharman DL, Gomes CP, Rutherford JP. Improvement in blood pressure control with impedance cardiography-guided pharmacologic decision making. Congest Heart Fail. 2004;10:54–58.
- Taler SJ, Textor SC, Augustine JE. Resistant hypertension: Comparing hemodynamic management to specialist care. Hypertension. 2002;39:982–988.
- Badila E,Dorobantu M, Bartos D, Iorgulescu C. The role of thoracic electrical bioimpedance in the control of high blood pressure. Romanian J Cardiol. 2006;21:13–22.
- Neath SX, Lazio L, Guss DA. Utility of impedance cardiography to improve physician estimation of hemodynamic parameters in the emergency department. Congest Heart Fail. 2005;11:17–20.
- Van De Water MJ, Miller WT, Vogel LR, Mount EB, Dalton LM. Impedance cardiography: The next vital sign technology?. Chest. 2003;123:2028–2033.
- Thangathurai D, Charbonnet C, Roessler P, Wo CC, Mikhail M, Yoahida R, et al. Continuous intraoperative noninvasive cardiac output monitoring using a new thoracic bioimpedance device. J Cardiothorac Vasc Anesth. 1997;11:440–444.
- Abdelhammed AI, Smith RD, Levy P, Smits GJ, Ferrario CM. Noninvasive hemodynamic profiles in hypertensive subjects. Am J Hypertens. 2005;18:51S–59S.
- Sramek BB, Ph.D. Systemic hemodynamics and hemodynamic management. InstantPublisher.com; 2002.
- HOTMAN System-integrated hemodynamic management system, Operator's manual. Sedona, AZ: HEMO SAPIENS; 2011.
- Kaplan NM, Kaplan's Clinical hypertension, 10th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2010.
- Bonow R. Braunwald's Heart disease. A textbook of cardiovascular medicine. 9th ed. Philadelphia, PA: WB Saunders Co.; 2008. p. 467.
- Ferrario CM, Page IH. Current views concerning cardiac output in the genesis of experimental hypertension. Circ Res. 1978;43:821–831.
- Davidson RC, Ahmad S. Hemodynamic profiles in essential and secondary hypertension. In: Izzo JL, Black HR, editors. Hypertension primer. 3rd ed. Dallas, TX: Council on High Blood Pressure Research, American Heart Association; 2003. p. 349–351.
- Sramek BB. Hemodynamics and its role in oxygen transport. Biomechanics of the cardiovascular system, Prague: Czech Technical University & Foundation for Biomechanics of Man;1995. p. 209–231.
- Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–1186.
- Kern JW, Pharm D, Shoemaker WC. Meta-analysis of hemodynamic optimization in high-risk patients. Crit Care Med. 2002;30:1686–1692.
- Sanford T, Treister N, Peters C. Use of noninvasive hemodynamics in hypertension management. Am J Hypertens. 2005;18 Suppl:87S–91S.
- Gaddam K, Nishizaka M, Pratt-Ubunama M, Pimenta E, Aban I, Oparil S, Calhoun D. Characterization of resistant hypertension : association between resistant hypertension, aldosterone, and persistent intravascular volume expansion. Arch Intern Med. 2008;168:1159–1164.