Abstract
Objective: Platelet endothelial aggregation receptor 1 (PEAR1) is a membrane protein involved in platelet contact-induced activation and sustained platelet aggregation. Experimental studies identified PEAR1, as a candidate gene that may be linked to the blood-pressure driven kidney injury in salt-sensitive Dahl rats. Aim: In a family-based European population study (mean age 39.7 years; 52.2% women), we searched for association of changes in blood pressure or incidence of hypertension with genetic variation in PEAR1. Methods: Among 1973 randomly recruited people, genotyped for PEAR1, we measured blood pressure at baseline and follow-up. Results: Median follow-up was 10.0 years. While accounting for family clusters and blood pressure at baseline and with adjustments applied for sex, age, body mass index, smoking and drinking, total cholesterol, and antihypertensive drug treatment, all associations of systolic and diastolic blood pressure changes with nine single nucleotide polymorphisms (SNPs) in PEAR1 were all non-significant (p ≥ 0.059). With similar adjustments, the incidence of hypertension (397 cases among 1532 participants were normotensive at baseline [25.9%]) was not related to the SNPs in PEAR1 (hazard ratios ≤ 1.09; p ≥ 0.09). Conclusion: Our study suggests that PEAR1 is not a hypertension susceptibility gene in humans.
Introduction
Platelet endothelial aggregation receptor 1 (PEAR1) is a recently discovered membrane protein involved in platelet contact-induced activation (Citation1) and sustained platelet aggregation (Citation2), and is highly expressed in platelets and endothelial cells. Genetic variants in PEAR1 are associated with increased platelet responses to agonists (Citation3) and the inter-individual variability in the response to antiplatelet drugs (Citation4,Citation5). A further study (Citation4) addressed the association between cardiovascular outcomes and genetic variation in PEAR1 in two independent aspirin-treated cohorts: 227 percutaneous coronary intervention patients and 1000 patients of the International Verapamil SR/Trandolapril Study Genetic Substudy (INVEST-GENES). In 144 white and 83 black patients undergoing percutaneous coronary intervention (Citation4), A-allele carriers of rs12041331 were more likely to experience a cardiovascular event or death compared with GG homozygotes (hazard ratio = 2.62; 95% confidence interval, CI, 0.96–7.10; p = 0.059; and hazard ratio = 3.97; 95% CI 1.10–14.31; p = 0.035, respectively). In aspirin-treated INVEST-GENES patients (Citation4), rs12041331 A-allele carriers had significantly increased risk of myocardial infarction compared with GG homozygotes (odds ratio = 2.03; 95% CI 1.01–4.09; p = 0.048).
Experimental studies identified PEAR1 as a candidate gene that may be linked to kidney injury in the salt-sensitive Dahl rat (Citation6), which developed kidney injury that became more severe as blood pressure rose in response to salt loading. Renal biopsies revealed a significantly lower nephron number in this strain compared with controls (Citation6), suggesting a possible link between kidney damage and the development of hypertension. Furthermore, the endothelium plays a pivotal role in the regulation of arterial resistance through its sensing and paracrine function (Citation7). We therefore searched for association between changes in blood pressure and the incidence of hypertension and genetic variation in PEAR1.
Methods
Recruitment for the Flemish Study on Environment, Genes, and Health Outcomes (FLEMENGHO) started in 1985. From 1985 to 1990 (Citation8,Citation9), a random sample of the households living in a geographically defined area of Northern Belgium was investigated with the goal to recruit an equal number of participants in each of six strata by sex and age (20–39, 40–59 and ≥ 60 years). From 1996 until 2004, recruitment of families continued using the former participants as index persons. The participants were repeatedly followed up. In all study phases, we used the same standardized methods to measure blood pressure and to administer questionnaires. The European Project on Genes in Hypertension (EPOGH) recruited participants from 1999 to 2001 (Citation10,Citation11). The EPOGH investigators applied the same protocol, questionnaires and follow-up procedures, as used in FLEMENGHO. The last follow-up examination took place from 2005 to 2008 in FLEMENGHO and from 2006 to 2008 in EPOGH (Citation11). Both studies complied with the Helsinki Declaration for investigation of human subjects. Each local institutional review board approved the study protocol. Participants gave written informed consent.
At baseline and follow-up, experienced observers measured each participant's anthropometric characteristics and blood pressure, and administered the standardized questionnaire to collect information on medical history, smoking and drinking habits, and use of medications. At each contact, blood pressure was the average of five consecutive auscultatory readings in the sitting position. Digit and number preference was checked at 6month intervals (Citation10). Hypertension was an untreated blood pressure of at least 140 mmHg systolic or 90 mmHg diastolic or use of antihypertensive drugs. For adolescents (n = 33), we used the thresholds specified by the European Society of Hypertension, which are stratified by sex, age and height percentiles (Citation12).
From 4535 subjects who initially agreed to participate in FLEMENGHO (n = 3343) and EPOGH (n = 1192), 65 participants were excluded because the baseline blood pressure measurements were missing), leaving 4470 subjects with a full set of required baseline measurements. Of these, 3085 subjects participated in at least one follow-up examination. We excluded 1112 participants from analysis, because the blood pressure measurements were missing (n = 40) or because their DNA was of bad quality (n = 115). Furthermore, 957 participants were not genotyped for PEAR1, because this gene was not included in a 16K custom-designed chip, used in addition to the Illumina 1M-Duo array and the 200K Cardio-Metabochip. Thus, the blood pressure cohort used to study change in blood pressure included 1973 participants. Changes in blood pressure during follow-up were calculated as the last minus the baseline blood pressure. The hypertension cohort used to study the incidence of hypertension encompassed 1532 participants, who were normotensive at baseline. We censored subjects from further analysis after occurrence of the first diagnosis of hypertension.
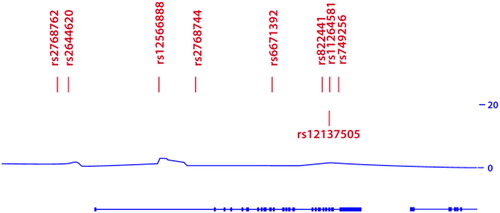
PEAR1 (size 22704 base-pairs) maps to a genomic area characterized by low linkage disequilibrium () on chromosome 1. We selected nine tagging single nucleotide polymorphism (SNPs; rs2768762, rs2644620, rs12566888, rs2768744, rs6671392, rs822441, rs11264581, rs12137505 and rs749256) that are in high linkage disequilibrium (R2 > 0.80) with ∼50 SNPs, covering the entire PEAR1 gene and having a minor allele frequency ≥ 1%. After extraction of genomic DNA from peripheral blood cells, the SNPs were genotyped using the TaqMan® Open Array™ Genotyping System (Life Technologies, Foster City, CA). All DNA samples were loaded at 50 ng per microliter and amplified on customized arrays following the manufacturer's instructions. For analysis of the genotypes, we used autocalling methods implemented in the TaqMan Genotyper software version 1.3 (Life Technologies). Next, genotype clusters were evaluated manually with the call rate set above 0.90. Sixteen duplicate samples gave 100% reproducibility. The overall call rate was 98%.
Statistical analysis was performed using SAS software, version 9.3. We applied a generalization of the standard linear model, as implemented in the PROC MIXED procedure of SAS package, to investigate the associations between the change in blood pressure over the time and explanatory variables, while accounting for relatedness among study participants and adjusting for covariables. A multivariable- adjusted Cox model was performed to study the incidence of hypertension in the population.
Results
The blood pressure cohort (n = 1973) included 1029 (52.2%) women. All participants were white Europeans. Age averaged (± SD) 39.7 years (range 19.5–83.5). Blood pressure at enrolment averaged 124.3 ± 16.5 mmHg systolic and 75.7 ± 10.5 mmHg diastolic. At baseline, 441 (22.4%) participants had hypertension, of whom 170 (38.5%) were on antihypertensive drug treatment. The hypertension cohort consisted of the 1532 participants, who were normotensive at baseline. In a randomly selected group of unrelated participants (n = 738), randomly selected from the blood pressure cohort, the frequencies of nine SNPs in PEAR1 did not deviate from Hardy– Weinberg equilibrium (0.11 < p < 0.99).
Follow-up data were available at one, two or three or more occasions in 3474 and 1496 participants, respectively. Median follow-up was 10.0 years (5th–95th percentile interval, 2.2–24.0 years). While accounting for family clusters and blood pressure at baseline and with adjustments applied for sex, age, body mass index, smoking and drinking, total cholesterol, and antihypertensive drug treatment, the associations between change in systolic or diastolic blood pressures with the nine SNPs in PEAR1 were all non-significant (). The incidence of hypertension among 1532 participants who were normotensive at baseline amounted to 397 (25.9%). With adjustments applied as before, incident hypertension was not associated with the SNPs in PEAR1. The hazard ratios were all smaller than 1.09 (p ≥ 0.09).
Table I. Multivariable-adjusted associations between blood pressure changes and PEAR1 single nucleotide polymorphism (SNPs).
Discussion
We could not confirm our working hypothesis that change in blood pressure over time or the incidence of hypertension are associated with genetic variation in PEAR1. The current literature data are based on genome-wide association studies (Citation3) and further genotyping that identified rs12041331 (Citation4,Citation5) as the SNP was associated with inter-individual variability in the responses to antiplatelet drugs and cardiovascular outcomes in aspirin-treated patients with coronary heart disease. In our current study, rs12566888 is a proxy of rs12041331with a D’ equal to 1 and Rsq of 0.85 with a distance of 667 base pairs. To cover the entire gene region, we selected in total nine tagging SNPs that are in high linkage disequilibrium with other known SNPs in PEAR1 (n = 50).
Recent experimental studies identified PEAR1 as an active determinant of different Akt driven endothelial functions, ranging from endothelial cell proliferation, migration and ultimately tube formation. Increasing PEAR1 expression during maturation of endothelial cells progressively activates Notch signalling, driving angiogenesis towards completion (Citation13). In 2012, compared with the spontaneously hypertensive rats (SHR), a major locus on chromosome 2 was identified that increases proteinuria in Dahl salt-sensitive (DSS) rats (Citation14). Williams and coworkers evaluated blood pressure, proteinuria and renal haemodynamics in congenic strains with small segments of the protective SHR genome on the DSS rat background (Citation6). Proteinuria and renal function were significantly improved in the congenic strains compared with the DSS rat. The causative locus interval was narrowed to less than 375 kb on the basis of congenic strains, haplotype data, comparative mapping and concordance with human genetic studies (Citation6). Sequencing of the coding region of genes in this region identified 36 SNPs (13 non-synonymous and 23 synonymous). Gene expression profiling indicated that only a few genes exhibited differential expression, including PEAR1 (Citation6). The homologous region in humans was found to be associated with estimated glomerular filtration rate in the Candidate Gene Association Resource population (Citation6). In spite of the well-known association between blood pressure and renal function in humans (Citation15), we could not find any association with change in blood pressure or incidence of hypertension and genetic variation in PEAR1.
The present study must be interpreted within the context of its potential limitations. First, our sample size was relatively small and 957 participants had no PEAR1 genotypes. Second, our findings were obtained in white Europeans and cannot be extrapolated to other ethnicities. Third, across our FLEMENGHO and EPOGH cohorts, we only assessed albuminuria, using a semi-quantitative dipstick method, so that we could not account for this covariable. However, additional adjustment of the mixed models () or the Cox regression models did not materially alter our results (data not shown). Finally, blood pressure at each visit was the average of only five consecutive blood pressure readings. However, as reported elsewhere, we implemented a stringent quality assurance and quality control programme (Citation10). In conclusion, based on our current observations in humans and pending confirmation in population studies with larger sample size, PEAR1 should not be considered as a hypertension susceptibility gene in humans.
Conflict of interest: None.
Funding
The European Union (HEALTH-2011.2.4.2-2-EU-MASCARA, HEALTH-F7-305507 HOMAGE and the European Research Council Advanced Researcher Grant-2011-294713-EPLORE), the Fonds voor Wetenschappelijk Onderzoek Vlaanderen, Ministry of the Flemish Community, Brussels, Belgium (G.0881.13 and G.088013) currently support the Studies Coordinating Centre in Leuven. The Genomic and Bioinformatics Units, Filarete Foundation, Milan received support from the InterOmics Project (PB05 MIUR-CNR Italian Flagship Project). The centre for Molecular and Vascular Biology receives support from the University of Leuven via the granting programs Programmafinanciering (PF/10/014) and Geconcerteerde Onderzoeksacties (GOA 2009/13) and from the Fonds voor Wetenschappelijk Onderzoek Vlaanderen (grants 11F2512N, 1801414N and G0A6514N).
References
- Nanda N, Bao M, Lin H, Clauser K, Komuves L, Quertermous T, et al. Platelet endothelial aggregation receptor 1 (PEAR1), a novel epidermal growth factor repeat-containing transmembrane receptor, participates in platelet contact- induced activation. J Biol Chem. 2005;280:24680–24689.
- Kauskot A, Di Michele M, Loyen S, Freson K, Verhamme P, Hoylaerts MF. A novel mechanism of sustained platelet αIIbβ3 activation via PEAR1. Blood. 2012;119:4056–4065.
- Johnson AD, Yanek LR, Chen MH, Faraday N, Larson MG, Tofler G, et al.Genome-wide meta-analyses identifies seven loci associated with platelet aggregation in response to agonists. Nature genet. 2010;42:608–613.
- Lewis JP, Ryan K, O’Connell JR, Horenstein RB, Damcott CM, Gibson Q, et al. Genetic variation in PEAR1 is associated with platelet aggregation and cardiovascular outcomes. Circ Cardiovasc Genet. 2013;6:184–192.
- Xiang Q, Cui Y, Zhao X, Zhao N. Identification of PEAR1 SNPs and their influences on the variation in prasugrel pharmacodynamics. Pharmacogenomics. 2013;14:1179–1189.
- Williams JM, Johnson AC, Stelloh C, Dreisbach AW, Franceschini N, Regner KR, et al.Genetic variants in arhgef11 are associated with kidney injury in the dahl salt-sensitive rat. Hypertension. 2012;1157–1168.
- Aird WC. Phenotypic heterogeneity of the endothelium. I. Structure, function, and mechanisms. Circ Res. 2007;100: 158–173.
- Staessen JA, Wang JG, Brand E, Barlassina C, Birkenhäger WH, Herrmann SM, et al. Effects of three candidate genes on prevalence and incidence of hypertension in a Caucasian population. J Hypertens. 2001;19:1349–1358.
- Li Y, Zagato L, Kuznetsova T, Tripodi G, Zerbini G, Richart T, et al.Angiotensin-converting enzyme I/D and α-adducin Gly460Trp polymorphisms. From angiotensin-converting enzyme activity to cardiovascular outcome. Hypertension. 2007;49:1291–1297.
- Kuznetsova T, Staessen JA, Kawecka-Jaszcz K, Babeanu S, Casiglia E, Filipovsky J, et al. Quality control of the blood pressure phenotype in the European Project on Genes in Hypertension. Blood Press Monit. 2002;7:215–224.
- Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, et al. Fatal and nonfatal outcomes, incidence of hypertension and blood pressure changes in relation to urinary sodium excretion in White Europeans. JAMA. 2011;305:1777–1785.
- Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, et al.Management of high blood pressure in children and adolescents: Recommendations of the European Society of Hypertension. J Hypertens. 2009;27:1719–1742.
- Vandenbriele C, Kauskot A, Luttun A, Jassens S, Hoylaerts M, Verhamme P. Platelet endothelial aggregation receptor-1 is a critical determinant of endothelial cell function. Circulation. 2012;126:A11115.
- Regner KR, Harmon AC, Williams JM, Stelloh C, Johnson AC, Kyle PB, et al.Increased susceptibility to kidney injury by transfer of genomic segment from SHR onto Dahl S genetic background. Physiol Genomics. 2012;44:629–637.
- Freedman BI, Iskandar SS, Appel RG. The link between hypertension and nephrosclerosis. Am J Kidney Dis. 1995;25:207–221.
