Abstract
The aim of this study was to assess sustained hypertension in children and its impact on cardiovascular target organ damage (TOD). Blood pressure (BP) was measured in children in Beijing in 2009. Primary hypertension was diagnosed based on three separate visits. Hypertensive children and normotensive children were followed up in 2011. According to these evaluations, three groups were defined: sustained hypertension, non-sustained hypertension and normotensive. Cardiovascular TOD and metabolic disorders were evaluated using pulse-wave velocity (PWV), carotid intima–media thickness (cIMT), and assessments of left ventricular structure and kidney function. A total of 3032 children aged 9–15 years participated in this survey, of whom 128 were diagnosed with hypertension after three separate BP measurements. Eighty out of 128 (62.5%) hypertensive and 158 normotensive children were available for follow-up in 2011. Forty-eight children were defined as having sustained hypertension, 38 as non-sustained hypertension and 152 as normotensive. Mean levels of brachial–ankle PWV (baPWV), left ventricular mass, left ventricular mass index (LVMI) and cIMT were significantly different between the three groups (p < 0.01). Compared to normotensives, the odds ratios and 95% confidence intervals for elevated LVM and cIMT were 5.27 (1.57–17.66) and 2.88 (1.03–8.09) in the non-sustained hypertensive group, and 3.28 (1.00–10.74) and 7.25 (2.69–19.58) in the sustained hypertensive group. The children with sustained hypertension have the highest risk of developing arterial stiffness, left ventricular hypertrophy and early blood vessel endothelium damage. The indices of cIMT, LVMI and PWV were useful to identify children at high risk of cardiovascular TOD.
Introduction
Hypertension is associated with an increased risk of myocardial infarction, stroke and cardiovascular mortality in adults (Citation1). Blood pressure (BP) tends to track from childhood into adulthood (Citation2,Citation3), and childhood hypertension has become a widely investigated topic within the past decade owing to its increasing prevalence. Even mildly elevated BP can have an adverse effect on target organs such as the arteries, heart, brain, kidney and retinal artery. However, the association between hypertension and target organ damage (TOD) in children has not been established. Assessment of subclinical TOD is helpful for predicting future cardiovascular disease (CVD) and establishing interventions for individuals with latent CVD. Recognition of high-risk populations at an early age may provide an opportunity for the reduction of TOD (Citation4). Several markers of damage, including pulse-wave velocity (PWV), left ventricular mass index (LVMI), carotid intima–media thickness (cIMT) and microalbuminuria (mA1b), have been applied to evaluate subclinical TOD. In the current study, we recruited hypertensive and normotensive children, and followed them for 2 years to evaluate the TOD, involving the heart, artery, kidney and fundus artery, and related conditions such as dyslipidemia and impaired fasting glucose (IFG). These parameters were used to select sensitivity indices for subclinical TOD. Screening for these early indices will provide opportunities for early identification and early intervention for populations at high risk of TOD.
Methods
Ethics statement
Written informed consent was obtained from each participant and/or their parents or guardians. The study protocol was approved by the Institutional Review Boards and Ethics Committees of the Capital Institute of Pediatrics, China.
Patients
A total of 3032 children aged 9–15 years were selected using stratified cluster sampling to participate in this BP survey in Beijing, China, in 2009.
Exclusion criteria were: diagnosed with hypertension by doctors; diagnosed with hypertension according to the physical examination record in the previous year; reported as having hypertension by themselves in the standard questionnaire performed in the first step of the current study; and children with renal or renal vascular diseases, central nervous system diseases and endocrine diseases, according to the information in the standard questionnaire performed in the first step of the current study.
In the end, 128 children were diagnosed with hypertension after three separate BP measurements with an interval of 15 days. Eighty out of 128 (62.5%) hypertensive and 158 normotensive children were available for follow-up in 2011. The 158 normotensive children were recruited by matching for gender and age with the hypertensive children to take part in the clinical examination of TOD evaluation in 2011.
Questionnaire
Information including physical activity, sleep time, parents’ educational level and history of hypertension was collected using a self-administered questionnaire conducted by the children and their parents.
Anthropometric measurements
At the initial visit, measurements were performed in a quiet, temperate room by trained clinical officers. Standing height without shoes was measured twice using a standard scale to the nearest 0.1 cm. Weight was measured with light clothing to the nearest 0.1 kg (Citation5). Body mass index (BMI) was calculated as weight divided by height squared (kg/m²).
Blood pressure measurement and hypertension screening procedure
BP was measured by trained examiners using a mercury sphygmomanometer in a sitting position according to a standard protocol (Citation6). After each subject had rested for at least 15 min, BP was measured on the right upper arm at the level of the heart. The cuff size was determined according to the size of the subject's arm to cover at least two-thirds of the upper arm. BP was measured three times on each visit. The three measurements were separated by intervals of at least 1 min. Korotkoff phase 1 (K1) and Korotkoff phase 4 (K4) were used to define systolic blood pressure (SBP) and diastolic blood pressure (DBP), respectively. Heart rate was recorded in beats/minute at each visit. BP was measured on up to two additional visits in children with elevated BP at 15 day intervals (Citation7).
All those who were hypertensive at baseline were advised to control their weight, limit salt intake, have enough sleep time and have proper physical activity in daily life. Those with severe hypertension (SBP and/or DBP above the 99th percentile by gender and age) were advised to see a specialist or physician to determine whether antihypertensive treatment was needed.
Pulse-wave velocity
An Omron VP-1000 vascular profiler (BP203RPE-II, Omron Corp, Tokyo, Japan) was used. Participants rested in the spine position with cuffs of appropriate sizes placed around the ankles and upper arms. Brachial–ankle pulse-wave velocity (baPWV) and carotid–femoral pulse-wave velocity (cfPWV) were calculated as the distance between two sensors divided by the time interval.
Left ventricular mass index and carotid intima–media thickness
B-mode Doppler ultrasonography (Sonos 5500, Andover, MA, USA), guided by two-dimensional echography, was performed by a single trained doctor. cIMT measurements were taken from the far wall of the artery in the two-dimensional presentation of the longitudinal view of the vessel, 1–2 cm below the bifurcation and along a 1 cm distance. Systolic and diastolic diameters were measured in B-mode presentation. Mechanical parameters of common carotid arteries were calculated from measurements taken in B-mode presentation of the artery. Left ventricular mass (LVM) was assessed by following the American Society of Echocardiography recommendations (Citation8). LVM was calculated using the formula of Devereux and colleagues (Citation9) and LVM index (LVMI = LVM/ height2.7) by De Simone's method (Citation10).
Biochemical index
After a minimum 10 h overnight fast, urine and venous blood samples were collected and analyzed for the concentrations of total cholesterol (TC), triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein (HDL), plasma glucose, high-sensitivity C-reactive protein (hs-CRP), cystatin-C (Cys-C) and urine mA1b/creatinine.
Classifications and definition
According to the Chinese Children Blood Pressure Reference (Citation11), elevated BP in children was defined as SBP and/or DBP ≥ 95th percentile by age and gender. Normotensive was defined as both SBP and DBP < 95th percentile by age and gender. Hypertension was defined as elevated BP on all three visits with a 15 day interval.
Children who remained hypertensive from baseline to follow-up were defined as sustained hypertensive, those who remained at a normal level over this period were defined as normotensive, and those whose BP status changed from normotensive to hypertensive or from hypertensive to normotensive were defined as non-sustained hypertensive.
Overweight and obesity were defined according to the “BMI classification reference for screening overweight and obesity in the Chinese school age children and adolescents” (Citation12).
Elevated cfPWV was defined as cfPWV ≥ 95th percentile by age and gender, and “normal” cfPWV as < 95th percentile by age and gender (Citation13).
Left ventricular hypertrophy (LVH) was defined as LVMI ≥ 95th percentile (Citation14) or relative wall thickness (RWT) ≥ 95th percentile by age and gender (Citation15), and both LVMI and RWT < 95th percentile by age and gender were classified as normal.
Fundus artery stiffness was hierarchically diagnosed according to the international Keith–Wagener method.
Early kidney damage was defined as random urine mA1b ≥ 20 mg/l or fasting serum Cys-C ≥ 1.0 mg/l.
IFG was defined as fasting glucose ≥ 5.6 mmol/l (Citation16). Dyslipidemia was defined as having one of the following: TC ≥ 5.18 mmol/l, TG ≥ 1.70 mmol/l, LDL-C ≥ 3.37 mmol/l and/or HDL-C < 1.04 mmol/l (Citation17).
The amount of physical activity, sleep sufficiency and parents’ educational level were evaluated based on the questionnaire (Citation7).
Statistical analysis
The t test and analysis of covariance were used to assess differences in mean BP, biochemical and TOD indices, respectively. Chi-squared and trend chi-squared tests were performed to describe the changes in TOD prevalence. Multivariable linear regression and logistic regression were performed to assess the association between BP and TOD. Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. Statistical significance was set at p < 0.05. Data were analyzed with SPSS, version 18.0 (SPSS, Chicago, IL, USA).
Results
A total of 3032 children (males 49.2%) aged 9–15 years participated in this survey. The BMI and prevalence of overweight and obesity in males (19.4 ± 0.1 kg/m², 15.6% and 17.0%, respectively) were significantly higher than in females (18.7 ± 0.1 kg/m², 13.0% and 11.9%, respectively, p > 0.05).
In total, 80 children with hypertension (62.5%, 80/128) and 158 age- and gender-matched normotensive children were available for follow-up. The gender ratio and age were not statistically different between the hypertensive and normotensive groups at baseline (p > 0.0.5). The levels of BMI, SBP and DBP were higher in the hypertensive group (26.2 ± 0.5 kg/m², 123.9 ± 1.2 mmHg and 76.9 ± 1.0 mmHg, respectively) than in the normotensive group (20.5 ± 0.4 kg/m², 105.4 ± 0.9 mmHg and 65.1 ± 0.7 mmHg, respectively). The prevalence of obesity was 66.3% in the hypertensive group, higher than that in the normotensive group (13.9%) at baseline (p < 0.05). There were no statistical differences between the entire hypertensive group and this follow-up group of 80 subjects with hypertension ().
Table I. Comparison of the characteristics between the follow-up and total hypertensive groups.
During the follow-up period, 152 children were considered normotensive, 48 children had sustained hypertension and 38 children were defined as having non-sustained hypertension. (Thirty-two hypertensive children in 2009 changed into normotensive in 2011, and six normotensive children in 2009 were determined as being de novo hypertensive in 2011; there were no statistical differences between the two groups of children, so they were combined together as one group.) The characteristics of the three groups are presented in .
Table II. Characteristics of blood pressure groups at follow-up.
Differences in TOD level were evaluated using analysis of covariance adjusted for gender, age and puberty status. Levels of baPWV, LVM, LVMI, RWT, cIMT and hs-CRP were higher in the sustained hypertensive group than in the non-sustained hypertensive and normotensive groups (p < 0.05) (). The changes in TOD prevalence were analyzed using the chi-squared test ().
Table III. Levels of target organ damage (TOD) index in different groups of blood pressure changes.
Table IV. Prevalence of target organ damage (TOD) in different groups of blood pressure changes.
Multiple linear regression was performed to assess the association of TOD index with the potential risk factors, with each TOD index as the dependent variable, and gender, age, puberty status, heart rate, SBP, DBP, BMI, family history of hypertension, sleep time, physical activity, parents’ education, fasting plasma glucose and blood lipids as the independent variables. Details of significant risk factors for each TOD index are shown in . Among them, BMI, SBP and DBP had stronger associations with most TOD indices than the other variables.
Table V. Risk factors for target organ damage.
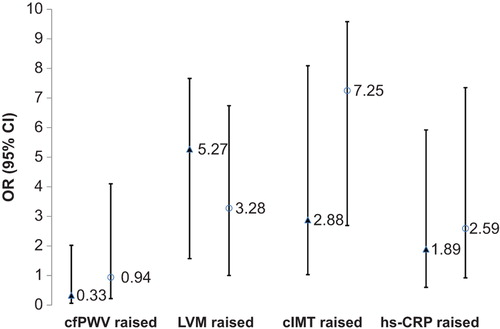
After adjusting for gender, age and puberty status, bivariate logistic regression was performed. Compared with the normotensive group, the risk of non-sustained hypertension and sustained hypertension on TOD was analyzed. For each TOD index, the OR and 95% CI are shown in , with the normotensive group as control.
Figure 1. Effects of blood pressure on cardiovascular target organ damage. Normotensive as control; black triangles represent non-sustained hypertension; white circle represent sustained hypertension; black line represents 95% confidence interval (CI). OR, odds ratio; cfPWV, carotid–femoral pulse-wave velocity; LVM, ventricular mass index; cIMT, carotid intima–media thickness; hs-CRP, high-sensitivity C-reactive protein.
Discussion
The current study found that baPWV, LVM, LVMI and cIMT were elevated in non-sustained hypertension and sustained hypertension. The prevalence rates of elevated LVMI, cIMT and hs-CRP were 14.6%, 47.9% and 31.1% in the sustained hypertension group, which were all statistically higher than in the non-sustained hypertension group (10.5%, 31.6% and 22.9%) and the normotensive group (2.0%, 12.5% and 9.7%). The risks of elevated LVM and cIMT were high, being 5.27 and 2.88 in the non-sustained group, and 3.28 and 7.25 in the sustained hypertension group, respectively.
There is ample evidence that the process of arteriosclerosis starts from childhood (Citation18,Citation19). However, hard endpoints, such as stroke and ischemic heart disease, are lacking in the pediatric population. Therefore, there is an increasing need to establish validated non-invasive tools to forecast cardiovascular risk in youth (Citation20). The results of this study confirm this view and provide further evidence- based data.
cfPWV has been considered the non-invasive gold-standard index of arterial stiffness (Citation21). However, measurement of baPWV is widely used in the general population since it has a good reproducibility and does not require special technical skills (Citation22). Moreover, several studies have reported that baPWV is an index of arterial stiffness showing similar characteristics and good correlation to aortic PWV (Citation23), and that a higher baPWV is associated with more advanced latent and clinical atherosclerotic lesions of the arterial wall in hypertension, diabetes and end-stage renal disease. That is the reason why the current study selected baPWV and cfPWV as the index to evaluate arterial stiffness in childhood, and the results supported this view.
The present study indicated that the baPWV increased significantly in relation to BP. This result is consistent with other studies, and indicates that the functions of vessels change when an increase in BP causes an augmentation of vascular tension. The prevalence of high cfPWV did not increase with elevated BP. The PWV standards should be ethically and regionally specific; the reference used in present study was based on 1008 Hungarian children (Citation13). Similar to studies in adults, we have shown that baPWV can be applied in routine clinical use and can be a powerful tool for the early diagnosis of atherosclerosis in medical institutions (Citation24,Citation25), The present study indicates that the measurements of baPWV may offer a simple and potentially useful approach for evaluating CVD, even in early childhood.
Pathological studies show that the increase in cIMT is an early process beginning in childhood, with fatty streaks observed in the aorta and the carotid arteries of children (Citation26). There is a positive correlation between the extent of the early atherosclerotic lesions in the aorta and coronary arteries and cardiovascular risk factors, such as BP, cholesterol concentrations, BMI and impaired glucose tolerance (Citation27).
The Bogalusa Heart Study cohort reported that CVD risk factors such as dyslipidemia, elevated BP and obesity identified in youth predict subclinical markers of atherosclerosis in the form of lesions in the aorta and coronary arteries measured at autopsy, as well as cIMT measured by non-invasive ultrasound (Citation28). Recent improvements in imaging technology (increased resolution and accuracy) have identified early vascular changes that can be assessed non-invasively using ultrasound. These early changes include thickening of vessel walls and impairment of arterial vasodilatory function. Studies in adults have shown that measurement of the thickness of cIMT represents an excellent marker of subclinical atherosclerosis (Citation29). Similarly, studies in children with hypercholesterolemia have demonstrated elevated cIMT compared with control children (Citation30).
In the current study, the elevated cIMT in hypertensive children confirmed the results obtained in mature adults and in young adults (Citation31), and the elevated cIMT in obese children confirmed the results in other studies (Citation32). This implies that cIMT could be taken as a sensitive index for screening high-risk populations for TOD in early childhood.
With hypertension, the cardiovascular system adapts to the varying neurohumoral and hemodynamic changes, and this may lead to the development of different left ventricular geometric patterns, each carrying a different risk profile for major adverse cardiovascular events (Citation33,Citation34). In children, LVH is the most prominent clinical evidence of TOD caused by hypertension. With the use of echocardiography to measure BP, LVH has been reported in 34–38% of children with mild, untreated BP elevation (Citation35). LVH is well established as an independent risk factor for cardiovascular morbidity and mortality in adults (Citation36). In children, LVH may result from cardiac congenital malformations, such as valvular aortic stenosis or familial hypertrophic cardiomyopathy.
The measurement and definition of LVH are important in the stratification of cardiovascular risk, which may affect treatment decisions in conditions such as extreme overweight, systemic hypertension, dilated cardiomyopathy and kidney failure in children. However, the complex relationship between myocardial growth and body growth in children has made indexing difficult for this age group. Different LVM indexing methods have been proposed in pediatric patients (Citation37,Citation38). The LVM of children with hypertension is greater than that of normotensive children. In a cross-sectional study of children with primary hypertension, the prevalence of LVH was 15.5% and 41.1% based on adult and pediatric criteria, respectively (Citation39). Other studies have emphasized the increased risk of LVH among children with hypertension and/or obesity (Citation40).
The measurements of mA1b and Cys-C had only weak associations with BP or BP changes in the current study, probably because kidney damage occurs later in the history of hypertension. Another reason may be that the mA1b was measured with urine collected in the morning, not 24 h urine, which may not represent the real concentrations of mA1b in blood. No fundus arteriosclerosis was found in either the normotensive or sustained hypertensive group, and therefore fundus arteriosclerosis may not be a sensitive early index of TOD in hypertensive children.
There were three reasons to select K4 as DBP in this study. The first is that K4 has been used as DBP in clinical and research experience in China for a long time. The second is that many studies have proved that the association between K4 and CVD is stronger than that between K5 and CVD. The last, but not least important reason is that many of the measurements of K5 were zero or close to zero, especially in younger children in China. Therefore, K4 was selected as DBP in the current study.
The study has a number of limitations. First, there is some heterogeneity in using the indices PWV, LVM, LVMI, cIMT and other TOD indices, even though this heterogeneity is taken into account by defining them according to age and gender. Further, the characteristics of one ethnic group may differ from those of another, and there are not enough specific reference data for Chinese children. No suitable baPWV reference for children could be found to clarify the use of baPWV, and only changes in the level of baPWV were analyzed in the current study. Secondly, the follow-up duration was only 2 years, which is a relatively short period in which to identify the development of TOD and could therefore potentially lead to biased conclusions. Additionally, BP was measured three times on only one occasion during the follow-up study, and was not based on repeated BP measurements as was the case at baseline.
In conclusion, children with sustained hypertension have the highest risks of developing arterial stiffness, LVH and early blood vessel endothelium damage. CIMT, LVMI and PWV are useful indices to identify children at high risk of TOD.
Acknowledgements
We gratefully acknowledge the contributions of data collection teams at all measurement time-points across the surveys. In particular, we thank the individuals who participated in the BP survey and the TOD estimation clinical examination. We also thank the staff of Beijing Centers for Diseases Control and Prevention and Beijing Maternal and Child Health Care Hospital.
Author contributions: JM contributed to the concept and design of the study. LM, DH, XZ, YH, JL and YY performed the data acquisition. LM performed the data analysis and interpretation. LM wrote the manuscript. All authors critically revised the manuscript for intellectual content and approved the final version. JM is the guarantor.
What is known about the topic: TOD not only happens in adults, and there is ample clinical evidence that the process starts from childhood. There is thus an increasing need to establish validated non-invasive tools to forecast TOD and cardiovascular risk in youth.
What this study adds: TOD and CVD could be assessed in hypertensive children in school- based surveys. cIMT, LVMI, and PWV subclinical indices are helpful in predicting future CVD and establishing interventions for children with latent CVD.
Financial Supports: The study has received the financial support from the National Nature Science Foundation of China (81172746) and the National “Twelfth Five-Year” Plan for Science & Technology Support Program (2012BAI03B03).
Declaration of interest: The authors have no conflicts of interest to disclose.
References
- Chaturvedi S. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): is it really practical? Natl Med J India. 2004;17:227.
- Iu K, Zh M, Misiavichene I, Shachkute A. Blood pressure dynamics and prognostication of hypertension: 20-year follow-up of children's cohort. Kardiologiia. 2004;44:30–4.
- Lauer RM, Mahoney LT, Clarke WR. Tracking of blood pressure during childhood: the Muscatine Study. Clin Exp Hypertens A. 1986;8:515–37.
- Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of systolic blood pressure during childhood: a 15-year follow-up population-based family study in eastern Finland. J Hypertens. 2002;20:195–202.
- World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1–452.
- Lawes CM, Vander HS, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part 1: Estimates of blood pressure levels. J Hypertens.2006;24:413–22.
- Meng L, Liang Y, Liu J, Hu Y, Yan Y, Mi J. Prevalence and risk factors of hypertension based on repeated measurements in Chinese children and adolescents. Blood Press. 2013;22:59–64.
- Henry WL, DeMaria A, Gramiak R, King DL, Kisslo JA, Popp RL, et al. Report of the American Society of Echocardiography Committee on Nomenclature and Standards in Two-dimensional Echocardiography. Circulation. 1980; 62:212–7.
- Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
- De Simone G, Devereux RB, Daniels SR, Koren MJ, Meyer RA, Laragh JH. Effect of growth on variability of left ventricular mass: assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am Coll Cardiol. 1995;25:1056–62.
- Mi J, Wang TY, Meng LH, Zhu GJ, Han SM, Zhong Y, et al. Development of blood pressure reference standards for Chinese children and adolescents. Chin J Evid Based Pediatr. 2010;5:4–14.
- Ji C. Body mass index reference norm for screening overweight and obesity in Chinese children and adolescents. Chin J Epidemiol. 2004;25:125–8.
- Reusz GS, Cseprekal O, Temmar M, Kis E, Cherif AB, Thaleb A, et al. Reference values of pulse wave velocity in healthy children and teenagers. Hypertension. 2010;56:217–24.
- Khoury PR, Mitsnefes M, Daniels SR, Kimball TR. Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr. 2009;22: 709–14.
- De Simone G, Daniels SR, Kimball TR, Roman MJ, Romano C, Chinali M, et al. Evaluation of concentric left ventricular geometry in humans: evidence for age-related systematic underestimation. Hypertension. 2005;45:64–8.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(Suppl 1):S64–71.
- Health of Children Group affiliated to Chinese Medical Association, Cardiovascular Group of Pediatric subassociation affiliated to Chinese Medical Association, Editorial Board of Chinese Journal of Pediatrics. Prevention and treatment of dyslipidemia in children and adolescents expert consensus. Chin J Pediatr. 2009;47:426–8.
- Juonala M, Jarvisalo MJ, Maki-Torkko N, Kahonen M, Viikari JS, Raitakari OT. Risk factors identified in childhood and decreased carotid artery elasticity in adulthood: the Cardiovascular Risk in Young Finns Study. Circulation. 2005;112: 1486–93.
- Aggoun Y, Szezepanski I, Bonnet D. Noninvasive assessment of arterial stiffness and risk of atherosclerotic events in children. Pediatr Res. 2005;58:173–8.
- Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the council on cardiovascular disease in the young and the council for high blood pressure research. Hypertension. 2008;52:433–51.
- Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–605.
- Munakata M, Ito N, Nunokawa T, Yoshinaga K. Utility of automated brachial ankle pulse wave velocity measurements in hypertensive patients. Am J Hypertens. 2003;16:653–7.
- Tsuchikura S, Shoji T, Kimoto E, Shinohara K, Hatsuda S, Koyama H, et al. Brachial–ankle pulse wave velocity as an index of central arterial stiffness. J Atheroscler Thromb. 2010;17:658–65.
- Lee NB, Park CG. Reproducibility of regional pulse wave velocity in healthy subjects. Korean J Intern Med. 2009;24:19–23.
- Maple-Brown LJ, Piers LS, O’Rourke MF, Celermajer DS, O’Dea K. Increased arterial stiffness in remote indigenous Australians with high risk of cardiovascular disease. J Hypertens. 2007;25:585–91.
- Stary HC. Lipid and macrophage accumulations in arteries of children and the development of atherosclerosis. Am J Clin Nutr. 2000;72(5 Suppl):1297–306S.
- McGill HC Jr, McMahan CA, Herderick EE, Tracy RE, Malcom GT, Zieske AW, et al. Effects of coronary heart disease risk factors on atherosclerosis of selected regions of the aorta and right coronary artery. PDAY Research Group. Pathobiological Determinants of Atherosclerosis in Youth. Arterioscler Thromb Vasc Biol. 2000;20:836–45.
- Magnussen CG, Venn A, Thomson R, Juonala M, Srinivasan SR, Viikari JS, et al. The association of pediatric low- and high-density lipoprotein cholesterol dyslipidemia classifications and change in dyslipidemia status with carotid intima–media thickness in adulthood evidence from the cardiovascular risk in Young Finns study, the Bogalusa Heart study, and the CDAH (Childhood Determinants of Adult Health) study. J Am Coll Cardiol. 2009;53:860–9.
- Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima–media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. 1997;96:1432–7.
- Pauciullo P, Iannuzzi A, Sartorio R, Irace C, Covetti G, Di Costanzo A, et al. Increased intima–media thickness of the common carotid artery in hypercholesterolemic children. Arterioscler Thromb. 1994;14:1075–9.
- Masoura C, Pitsavos C, Aznaouridis K, Skoumas I, Vlachopoulos C, Stefanadis C. Arterial endothelial function and wall thickness in familial hypercholesterolemia and familial combined hyperlipidemia and the effect of statins. A systematic review and meta-analysis. Atherosclerosis. 2011;214:129–38.
- Urbina EM, Kimball TR, McCoy CE, Khoury PR, Daniels SR, Dolan LM. Youth with obesity and obesity-related type 2 diabetes mellitus demonstrate abnormalities in carotid structure and function. Circulation. 2009;119:2913–9.
- Safar ME, Siche JP, Mallion JM, London GM. Arterial mechanics predict cardiovascular risk in hypertension. J Hypertens. 1997;15:1605–11.
- Lopez RM, Gomez CJ, Barbado HFJ.[Endothelial dysfunction and vasculitis: a close relationship]. Rev Clin Esp. 2006; 206:199–201.
- Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113:328–33.
- Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med. 1990;322:1561–6.
- Foster BJ, Mackie AS, Mitsnefes M, Ali H, Mamber S, Colan SD. A novel method of expressing left ventricular mass relative to body size in children. Circulation. 2008;117: 2769–75.
- Cain PA, Ahl R, Hedstrom E, Ugander M, Allansdotter-Johnsson A, Friberg P, et al. Physiological determinants of the variation in left ventricular mass from early adolescence to late adulthood in healthy subjects. Clin Physiol Funct Imaging. 2005;25:332–9.
- Hanevold C, Waller J, Daniels S, Portman R, Sorof J. The effects of obesity, gender, and ethnic group on left ventricular hypertrophy and geometry in hypertensive children: a collaborative study of the International Pediatric Hypertension Association. Pediatrics. 2004;113:328–33.
- Brady TM, Fivush B, Flynn JT, Parekh R. Ability of blood pressure to predict left ventricular hypertrophy in children with primary hypertension. J Pediatr. 2008;152: 73–8, 78.e1.
