Abstract
Background: The Brief Obsessive Compulsive Scale (BOCS), derived from the Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) and the children's version (CY-BOCS), is a short self-report tool used to aid in the assessment of obsessive–compulsive symptoms and diagnosis of obsessive–compulsive disorder (OCD). It is widely used throughout child, adolescent and adult psychiatry settings in Sweden but has not been validated up to date. Aim: The aim of the current study was to examine the psychometric properties of the BOCS amongst a psychiatric outpatient population. Method: The BOCS consists of a 15-item Symptom Checklist including three items (hoarding, dysmorphophobia and self-harm) related to the DSM-5 category “Obsessive–compulsive related disorders”, accompanied by a single six-item Severity Scale for obsessions and compulsions combined. It encompasses the revisions made in the Y-BOCS-II severity scale by including obsessive–compulsive free intervals, extent of avoidance and excluding the resistance item. 402 adult psychiatric outpatients with OCD, attention-deficit/hyperactivity disorder, autism spectrum disorder and other psychiatric disorders completed the BOCS. Results: Principal component factor analysis produced five subscales titled “Symmetry”, “Forbidden thoughts”, “Contamination”, “Magical thoughts” and “Dysmorphic thoughts”. The OCD group scored higher than the other diagnostic groups in all subscales (P < 0.001). Sensitivities, specificities and internal consistency for both the Symptom Checklist and the Severity Scale emerged high (Symptom Checklist: sensitivity = 85%, specificities = 62–70% Cronbach's α = 0.81; Severity Scale: sensitivity = 72%, specificities = 75–84%, Cronbach's α = 0.94). Conclusions: The BOCS has the ability to discriminate OCD from other non-OCD related psychiatric disorders. The current study provides strong support for the utility of the BOCS in the assessment of obsessive–compulsive symptoms in clinical psychiatry.
Obsessions and compulsions are considered the main features of obsessive–compulsive disorder (OCD); however in the DSM-5, body dysmorphic disorder, hair-pulling, hoarding and skin-picking are all included under the new chapter “Obsessive–compulsive related disorders”, reflecting the association between one another and OCD. Moreover, obsessive–compulsive symptoms have a high frequency of comorbidity with a range of other psychiatric disorders (Citation1–3).
Although the core symptoms of OCD are easily identified, most outpatients with OCD remain unrecognized by their psychiatrist (Citation3). The use of rating scales, however, may improve and facilitate the assessment of OCD. The Yale–Brown Obsessive–Compulsive Scale (Y-BOCS) is regarded as the gold standard (Citation4, Citation5). A very similar version for children (CY-BOCS) was introduced in 1997 (Citation6). Both versions have been widely used in research and in clinical settings (Citation7, Citation8). A second edition of the Y-BOCS (Y-BOCS-II) differed from the original by including assessments of obsessive–compulsive free intervals and extent of avoidance (Citation9). Both Y-BOCS versions, as well as CY-BOCS, consist of two parts: first part consisting of an extensive symptom checklist of 54 items in the Y-BOCS and more than 60 items in the CY-BOCS, followed by a second part made up of a separate clinician-rated scale measuring symptom severity. A self-rated version of Y-BOCS (Citation10) has shown a good agreement with the Y-BOCS (Citation11) however less for obsessions than for compulsions (Citation12).
Today an array of self-reports for OCD are available but each one has limitations (Citation13, Citation14). In short, either they are too extensive or repetitive, hampering their clinical use (Citation10, Citation15, Citation16), lack discriminative power (Citation17–19), have low convergence with Y-BOCS (Citation20–23), include items that are not associated with OCD (Citation24) or do not measure severity (Citation25).
Succinct and psychometrically valid instruments for identifying obsessive–compulsive symptoms and assessing their severity, tested in large psychiatric populations, are still lacking. In view of this, a shortened self-rated version of Y-BOCS and CY-BOCS combined, developed 1997–2002 was the Brief Obsessive–Compulsive Scale (BOCS) (Citation26). It consists of both a symptom checklist section illustrated with examples and a severity scale section. Today, the BOCS is in wide use throughout child, adolescent and adult psychiatry settings in Sweden. The aim of the present study was to evaluate psychometrically the BOCS—assessing its internal consistency, factor structure, sensitivity and specificity in OCD versus autism spectrum disorder (ASD), attention-deficit/hyperactivity disorder (ADHD) and a mixed non-OCD group of adult psychiatric patients.
Material and methods
Patient characteristics
The main sample consisted of 402 psychiatric outpatients (range 18–82 years) recruited through a number of different clinical and non-clinical services in Sweden. Sample characteristics are shown in . The patients were divided into four diagnostic groups: 1) OCD, consisting of patients with a diagnosis of OCD, with or without psychiatric comorbidity; 2) ASD without a diagnosis of OCD but possibly with other types of psychiatric comorbidity; 3) ADHD without a diagnosis of OCD or ASD but possibly with other types of psychiatric comorbidity, and 4) a mixed psychiatric group without a diagnosis of a comorbid OCD, ASD or ADHD.
Table 1. Patient characteristics.
Ninety-four of these patients had a primary diagnosis of OCD. Information on patients’ affiliation, diagnostic instrument used, year of enrolment and settings are shown in . All patients who completed the BOCS in a structured way were included.
Table 2. Affiliation, recruitment, setting and diagnostic procedures in study participants.
A subgroup consisting of 12 OCD outpatients was included from a cognitive behavioural therapy (CBT) treatment programme at a psychiatric outpatient unit in Stockholm. These patients were assessed with the NIMH-GOCS (National Institute of Mental Health Global Obsessive Compulsive Scale (Citation27))—a single-item expert rating of the overall severity of obsessive–compulsive symptoms—in addition to self-assessment with BOCS prior to and post-treatment.
Patients with primary diagnoses of ADHD or ASD were recruited through consecutive referrals to St Göran hospital in Stockholm, or to the Gothenburg Neuropsychiatric Genetic Project. If the SCID I interview (Citation28) implied the presence of any obsessions or compulsions the patient was further assessed with the BOCS.
The mixed psychiatric group consisted of patients with primary diagnoses of (non-OCD) anxiety disorders, tic disorders, depression, eating disorders and personality disorders. They were recruited through the specialized outpatient clinic at St Göran hospital, the Gothenburg Neuropsychiatric Genetic Project or through a research project on social anxiety disorder. The study was approved by the medical ethical review boards at each site.
All patients were interviewed face-to-face and diagnosed by a senior psychiatrist. Forty-two patients were diagnosed earlier, according to DSM-III-R (Citation29), while the other patients were diagnosed according to DSM-IV (Citation30), assessed through the Clinical Interview for DSM-IV—Axis I Disorders (SCID-I) (Citation31) or a structured DSM-IV-based clinical interview. The gender ratio varied across the diagnostic groups, with a male predominance among patients with ASD, and more females in the OCD group (chi-square 11.96, df = 3, P = 0.008). Mean Global Assessment of Functioning (GAF) score (Citation29, Citation30) was significantly lower in patients with ASD in comparison with the other groups (P ≤ 0.05 in a post hoc analysis).
Development of the symptom checklist
The symptom checklist of the self-report Y-BOCS and the CY-BOCS were combined into a 62-item checklist and divided into sections roughly in accordance with the 13 main pre-set symptom categories of the Y-BOCS (Citation32). The order of the checklist items was rearranged so that an item related to a specific obsession was immediately followed by an item relating to the corresponding compulsion. For example, “I am concerned that I may contaminate others by spreading dirt or germs” was followed by “I wash my hands excessively or in a ritualized way in order to avoid contamination”, with examples provided. Each checklist item was followed by a request to specify if each symptom was present “right now” (i.e. during the past week), “in the past” or “has never been present”. Next, the given examples were rephrased into less personal, more casual formulations. To make the examples less personal “you” was replaced by “one”. The type of obsession, e.g. whether it was the need for “the just right feeling” or a magical (i.e. superstitious) belief that preceded the ritual, was specifically targeted in order to distinguish different justifications for the compulsion. This distinction is not accommodated by the Y-BOCS but is considered of great clinical relevance. This 62-item checklist was completed by 61 of the OCD patients.
The final symptom checklist items were selected to fulfil the following: if any of these 61 patients had endorsed only one item within a section, this item should be included. For those endorsing more than one item within a section, at least one of these items should be included. As within each section some items were much more often endorsed than others, it turned out that only one or two items per section were necessary in order to fulfil these requirements. Thus the remaining items were considered superfluous and excluded from the checklist. This “pruning” of the Y-BOCS/CY-BOCS symptom checklist resulted in 14 hierarchically superordinate and highly relevant items. In addition, one item reflecting self-harm (included in the Miscellaneous compulsions section of the Y-BOCS checklist) was added based on the clinical observation that patients with comorbid ASD, tic disorders and borderline personality disorder occasionally harm themselves in a compulsive or ritualized manner. This was considered clinically important to include.
In sum, 11 symptom areas—(A) contamination/cleanliness, (B) harming obsessions, (C) sexual obsessions, (D) checking, (E) religious/magical thoughts/superstition, (F) morality and justice, (G) symmetry/exactness/ordering, (H) just right/repeating rituals/counting, (I) hoarding and saving, (J) somatic obsessions and (K) self-harming behaviours—covered by 15 items, formed the BOCS symptom checklist. In addition, the respondent was invited to also add additional information if s/he had any other symptoms not included in the checklist as an addition to the list of the most troublesome symptoms.
The obsession and compulsion ratio and inter-rater reliability
The Y-BOCS provides sub-scores on obsessions and compulsions. In order to estimate the percentage of obsessive and compulsive symptoms respectively, the BOCS asks: “What is worse, your obsessions or your compulsions? If you separate your obsessions and your compulsions, what percent are the former and what the latter?” If this question was incomprehensible to the patient, an alternative version with a circle divided into eight sections was presented, followed by the question: “Obsessions and compulsions should together fill the circle. Please dash the sections that correspond to your compulsions/habits. The empty sections correspond to your obsessions/thoughts”.
Sixty patients with OCD completed the BOCS and were interviewed with Y-BOCS in the same session. The aim was to investigate the inter-rater reliability between patient and expert ratings of the obsession and compulsion quotient. The order of the two scales was randomly administrated.
The severity scale
The BOCS severity scale includes six questions measuring the severity of the disorder. These questions are based on the Y-BOCS severity rating but have been reduced in number. While the Y-BOCS, CY-BOCS and the Y-BOCS-II have separate severity ratings for obsessions and compulsions, the BOCS severity rating refers to both obsessions and compulsions. Response options range from none to extremely, scored from 0 to 4, and thus identical to the original Y-BOCS and CY-BOCS scorings. The BOCS encompasses the revisions made in the Y-BOCS-II severity scale by including obsessive–compulsive free intervals, extent of avoidance and excluding the resistance items.
Scale scoring
For the purpose of psychometric testing, all scale scores were calculated as mean scores. The scores were first summed to a total score, and then divided by the number of items to which the patient had responded. If the patient had more than two missing responses, the mean score was set as a missing value.
Statistical analysis
Statistical calculations and analyses were performed with SPSS version 19. Data were summarized using standard descriptive methods, such as frequency, mean and standard deviation. The intercorrelation matrix was studied through principal component analysis (Oblimin rotation). Five factors were extracted (adjusted for low (< 0.35) communalities). For calculations of sensitivity and specificity, cross-tables and the receiver operating characteristics (ROC) curves between diagnosis and score were established. Scores were then dichotomized using values as close to the median as possible. Internal consistencies were expressed as Cronbach's alphas and mean inter-item correlation coefficients. Correlations between total BOCS scale scores and age, GAF and NIMH-GOCS were expressed as non-parametric Kendall's rank correlation coefficients (τ). The correlation between the obsessions and compulsions in Y-BOCS and BOCS was expressed as Pearsons’ product-moment correlation coefficient. Differences between diagnostic groups in age and GAF scores were analysed with one-way analysis and post hoc tests with Tukey's HSD test. Differences between diagnostic groups in item scores were analysed with a non-parametric Kruskal–Wallis test also corrected for multiple testing. The significance level in all analyses was set at 5% (two-tailed). Since most of the analyses had an implicit directed hypothesis this is, in fact, mostly equivalent to a significance level of 2.5%.
Results
The symptom checklist
Endorsement
Frequencies of endorsement of the BOCS symptom checklist items are presented in . Eight items (listed from highest to lowest endorsement: 6, 1, 2, 11, 12, 10, 3, 5) significantly distinguished the OCD patients from all the other diagnostic groups. However, for five items (Citation4, Citation7, Citation14, Citation15, Citation16), no significant differences were found between the diagnostic groups.
Table 3. Frequency of endorsement of Brief Obsessive–Compulsive Scale (BOCS) Symptom Checklist items in psychiatric patients.
Factor structure
All the variables were entered in a principal component analysis. The first analysis of the symptom checklist items identified four components. The communalities and correlations of six items were however, very low. Therefore, a second analysis was performed with five extracted components with acceptable levels of the communalities (). The components were denoted: (I) “Symmetry”, (II) “Forbidden thoughts”, (III) “Contamination”, (IV) “Magical thoughts” and (V) “Dysmorphic thoughts”. Based on the factor structure subscales were established. In , the mean scores of the subscales are presented for the four diagnostic groups. The OCD group had the highest score on all subscales compared with all other groups. The largest difference was found for the Contamination subscale [F(3,398) = 26,25, P < 0.001]. A Tukey test revealed significant differences between the OCD population in comparison with the other diagnostic groups on most subscales. The exception was the Magical thoughts subscale, where the OCD group did not differ significantly from the mixed psychiatric group.
Table 4. Factor loadings of BOCS Symptom Checklist items.
Internal consistency
The internal consistency of the total symptom checklist () was good (> 0.80); however, this was lower for the subscales. Three of the subscales had Cronbach's alphas close to 0.70 and mean inter-item correlations ranging from 0.31 to 0.52. The mean inter-item correlation for the total symptom checklist was 0.22.
Sensitivity and specificity
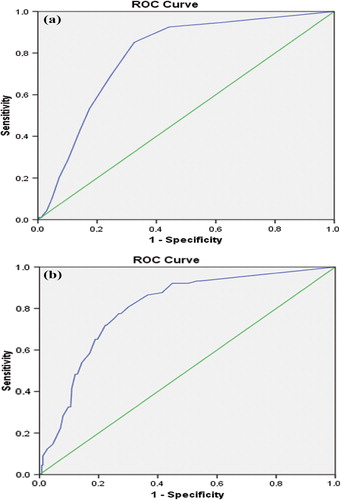
Sensitivity and specificity for OCD diagnosis for the symptom checklist was calculated. The cut-off score was set to 0.15 representing a mean endorsement of 15% of the items; this divided the total sample into two equally sized groups (55% below and 45% above the cut-off). The sensitivity was very high with 85% of the OCD patients being correctly identified. The specificity was somewhat lower; 62% of the patients with ASD, 69% of the ADHD patients, and 70% of the patients with other various diagnoses were correctly identified as not having an OCD diagnosis. A ROC curve of the BOCS checklist yielded an area under the curve (AUC) of 0.79 and 0.80 for the BOCS severity scale ().
Obsession and compulsion ratio and inter-rater reliability
The distribution of self-rated obsessions vs. compulsions did not differ significantly between the OCD group and the other diagnostic group combined (P = 0.27). Among the OCD group, obsessions and compulsions were equally common (50%:50%), whereas in the other diagnostic groups, obsessions were slightly more common than compulsions (56%:44%). The distribution between obsessions and compulsions in the Y-BOCS subscales was highly correlated with the distribution between self-rated obsessions and compulsions in the BOCS (r = 0.67, P < 0.001). The administration order of the two measures had no significant effect on the results.
The BOCS severity scale
Means and standard deviations for the six items measuring severity are presented in . Patients were asked to complete these items only if s/he endorsed any of the symptom checklist items. If they had not, the score of these items were set to zero (“0”). Also, some patients refrained from completing this section even though they had scored on the symptom checklist items. For those reasons, the total number of people in this analysis was different from that in . As can be seen in , the OCD patients scored significantly higher on each item in the severity scale. The factor analysis performed yielded a single factor. The internal consistency of the severity scale was, thus, very high (Cronbach's alpha = 0.94 and the mean inter-item correlation was 0.73). The mean cut-off score was 1.50, and divided the sample into two groups of severity (low = 65% vs. high = 35%, n = 354). Seventy-two per cent of the OCD patients were correctly identified, as were 75% of the ASD patients, 76% of the ADHD patients and 84% of the patients with mixed psychiatric disorders.
Table 5. Mean and standard deviation of Severity Scale items and total score for psychiatric patients diagnosed with obsessive–compulsive disorder (OCD), autism spectrum disorders (ASD), attention deficit/hyperactivity disorder (ADHD) and the mixed psychiatric group.
Correlations between the BOCS and the global assessment of functioning
There were modest negative correlations between the mean number of endorsed items in the symptom checklist and the mean of the severity scale, and GAF (rxy = − 0.17, P = 0.004 and rxy = − 0.28, P < 0.001, respectively) indicating that higher scores on the symptom checklist and severity scale were associated with lower level of global functioning.
Sensitivity to change
The self-rated BOCS severity rating before and after CBT treatment, strongly and positively correlated with clinician NIMH-GOCS ratings before and after treatment (τ = 0. 93, P < 0.001, n = 12).
Discussion
This paper has presented the BOCS, a shortened and modified self-administered version of the Y-BOCS and CY-BOCS, consisting of a 15-item checklist and a six-item severity scale (Please find this material with the following direct link to the article: http://dx.doi.org/10.3109/08039488.2014.884631) Since its introduction in Sweden more than a decade ago, it has been widely used in assessment of OCD, which illustrate its face validity. The current study provides strong support for the utility of the BOCS in the assessment of OCD in adults.
Psychometric properties
The BOCS symptom checklist showed good to excellent psychometric properties, with a high sensitivity (85%) and specificity (67%), especially considering that the comparison group consisted of cohorts of psychiatric patients and not of healthy controls. The mean inter-item correlations describe how different items are related to one another. Ideally, they should fall between 0.15 and 0.50. A mean inter-item correlation of 0.22 was obtained for the total BOCS symptom checklist, and fell between 0.31 and 0.52 for the separate subscales. This is a strong indication that the BOCS subscales indeed measure different properties, related to but nevertheless different from one another. Also, sensitivity and specificity of the six items in the BOCS severity scale, performed well in discriminating OCD from other psychiatric diagnoses.
Clinical usefulness
Together, the findings indicate that BOCS can successfully identify individuals who are likely to match the diagnostic criteria for OCD. As expected, some psychiatric patients without an OCD diagnosis have obsessions and/or compulsions. This was especially common among patients with ASD, in which ritualistic behaviours and hoarding is often part of the clinical profile (Citation33). However, the OCD patients showed BOCS scores almost twice as high as that of the ASD patients (). In addition, the obsessive–compulsive characteristics that are typically to be expected in patients with ASD were most frequent in component I denoted “Symmetry”. In the study, we chose to categorize ASD patients with a comorbid OCD as “OCD”, and this may have attenuated loading on component I ().
The subscale structure of the BOCS
The five components that were extracted by the factor analysis of the symptom checklist bear clinical relevance for OCD and cover some of the symptomatology described as the broader OCD phenotype. Component I includes items that regard symmetry, ordering and “just right” (items 10–12) that are common in tic disorders and ASD (Citation34, Citation35). Preoccupation with morality and justice (item 9), and collecting and hoarding (item 14) characterize both obsessive–compulsive personality disorder and ASD but could also be expected to be rather common in the general population. We expect, this is the reason those items showed a low communality. Aggressive and sexual obsessions (i.e. items 3, 4, 5) and self-harm (item 16) showed a high loading (> 0.5) in component II. Both skin-picking and hair-pulling, included in the new category of obsessive–compulsive related disorders in DSM-5, could be endorsed as self-harming behaviours. As expected, washing and fear of germs (items 1 and 2 in component III) most convincingly discriminated the OCD group from other psychiatric patients, mainly because these symptoms are highly specific for OCD. Magical and religious obsessions constitute component IV, the singular component that did not discriminate OCD from other psychiatric disorders. Although magical thinking is very common among people in general, it rarely becomes problematic. However, because people with OCD often are unable to trust their own senses, they are susceptible to superstitious beliefs and magical rituals for reassurance. For this reason item 13, the unlucky number, is absent in the BOCS checklist.
The two items in component V, checking electrical appliances (item 6) and worries about one's appearance (item 15), showed a lower internal consistency than the other factors. This could be attributed to the unspecific nature of these symptoms; apparently, they are very common in the general population (Citation36).
Similarities and differences in the factor analysis of Y-BOCS, CY-BOCS and BOCS
A large meta-analysis published by Bloch and co-workers on the Y-BOCS and CY-BOCS symptom checklists based on the 13 main pre-set symptom categories resulted in a four-factor solution (Citation32). The four symptom dimensions identified were (Citation1) Symmetry: obsessions and repeating, ordering and counting compulsions; (Citation2) Forbidden thoughts: aggression, sexual and religious obsessions and checking compulsions; (Citation3) Cleaning: cleaning and contamination, and (Citation4) Hoarding: hoarding obsessions and compulsions. Our findings were slightly different, presumably because we included patients with ASD, ADHD and other psychiatric disorders, whereas Bloch restricted his selection to studies on OCD patients only. Nevertheless, the BOCS is constructed of five factors recognised as representing discrete variants of OCD. Specifically: the BOCS-component I “Symmetry” corresponds to the collapsed dimensions “Symmetry” and “Hoarding” in Y-BOCS and CY-BOCS. Noteworthy, a forced three-factor solution of CY-BOCS and Y-BOCS lumped hoarding and symmetry/ordering together, indicating that these are closely linked. Similarly, when the Y-BOCS checklist symptoms were classified into categories as either being “absent”, “present” or “prominent”, hoarding and symmetry/ordering loaded into a common factor (Citation32). The component II “Forbidden thoughts” corresponded roughly to the second factor in the Y-BOCS, although the BOCS, in contrast to the Y-BOCS and CY-BOCS, categorize religious and somatic obsessions into other components. However, the relationship between aggressive, sexual, religious and somatic obsessive–compulsive symptom dimensions in the Y-BOCS and CY-BOCS is unclear and further investigation on singular item level has been recommended (Citation32). While the BOCS component III “Contamination” is identical to the Y-BOCS and CY-BOCS contamination dimension, the fourth component (IV) “Magical thoughts” constitutes a major difference. This component consists of a superstitious and a religious item both showing a high loading on the factor. Presumably, the emergence of this “new factor” is attributed to the fact that the BOCS specifically distinguishes between compulsions performed due to the need for “the just right feeling” or those performed due to magical thinking. Finally component V “Dysmorphic thoughts”, includes items regarding worry about own appearance and checking compulsions. The corresponding items (somatic obsession and checking) were problematic in the meta-analysis of the Y-BOCS and the CY-BOCS by showing divergent loading patterns between the two instruments; moreover, the checking compulsion items were associated with almost all factors in the Y-BOCS and the CY-BOCS (Citation32). In addition, when a five-factor solution was forced, checking and somatic obsessions were separated out as a fifth factor (Citation32) identical to the BOCS component Dysmorphic thoughts.
Limitations
This study has limitations that should be addressed. Firstly, the patients were assessed with different DSM criteria because some patients were diagnosed before 1994 and not re-diagnosed at the introduction of the DSM-IV. However, the diagnostic criteria for OCD are almost identical in the DSM-III-R compared with the DSM-IV, thus they are widely viewed as interchangeable (Citation37), which also applies to the corresponding DSM-5 criteria. However, hoarding is now categorized as a separate diagnosis, similar to dysmorphic obsessions in body dysmorphic disorder. The two corresponding BOCS items, in addition to the self-harm item, can be helpful in identifying disorders within the new category of obsessive–compulsive related disorders in the DSM-5, thus suggesting an extended utility for the BOCS.
Although each patient was diagnosed through a structured interview lasting for several hours, the SCID-I Interview was not completed for all patients. However, the gestalt of OCD is remarkably consistent, irrespective of diagnostic instrument. Almost all OCD patients have a history of typical washing, checking and/or repeating compulsions. Accordingly, it seems reasonable to combine patients from various clinical settings.
Data on the number of OCD patients that had received successful treatment was unfortunately not available in this study. Some of the patients in the OCD group were treated and therefore may score lower on the BOCS than prior to treatment. Thus, the sensitivity of the BOCS in treatment-naïve OCD patients is presumably higher than reported here.
Unfortunately, only a small sample of 12 OCD patients was followed while receiving CBT treatment. Nevertheless, the trial illustrated that the expert assessment and the patient rated BOCS reached high agreement, indicating that BOCS was indeed sensitive to change.
Conclusions
In clinical practice, time for assessing OCD symptoms in detail is rarely available, and co-existence of signs and symptoms from different diagnostic categories is extensive among psychiatric patients. Self-rating scales must be brief but still provide comprehensive information, be valid and user-friendly, reliable, flexible and free of charge (Citation38). Hopefully, future studies will confirm that the BOCS encompasses all these qualities and affirm its validity amongst other populations.
BOCS Brief Obsessive Compulsive Scale
Download PDF (177.3 KB)Acknowledgements
This project was supported by grants from the Swedish Research Council (No 523-2011-3646 and 523-2011-3807). Financial support was also provided through the regional agreement on medical training and clinical research (ALF) between the Stockholm County Council and the Karolinska Institutet. The funders did not interfere with the study design, the data collection, data analysis or manuscript preparation or decisions on the manuscript. We want to express our gratitude towards all patients who agreed to sign up for the study and to Stephanie Plenty and Aida Malovic for reviewing the manuscript.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Supplemental Material
Supplemental data for this article can be accessed on the http://dx.doi.org/10.3109/08039488.2014.884631.
References
- Murphy DL, Timpano KR, Wheaton MG, Greenberg BD, Miguel EC. Obsessive–compulsive disorder and its related disorders: A reappraisal of obsessive–compulsive spectrum concepts. Dialogues Clin Neurosci 2010;12:131–48.
- Okasha A, Lotaief F, Ashour AM, el Mahalawy N, Seif el Dawla A, el-Kholy G. The prevalence of obsessive compulsive symptoms in a sample of Egyptian psychiatric patients. Encephale 2000;26:1–10.
- Wahl K, Kordon A, Kuelz KA, Voderholzer U, Hohagen F, Zurowski B. Obsessive–compulsive disorder (OCD) is still an unrecognised disorder: A study on the recognition of OCD in psychiatric outpatients. Eur Psychiatry 2010;25:374–7.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale–Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006–11.
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, et al. The Yale–Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry 1989;46:1012–6.
- Scahill L, McDougle CJ, Williams SK, Dimitropoulos A, Aman MG, McCracken JT, et al. Children’s Yale–Brown Obsessive Compulsive Scale modified for pervasive developmental disorders. J Am Acad Child Adolesc Psychiatry 2006;45:1114–23.
- Leckman JF, Grice DE, Boardman J, Zhang H, Vitale A, Bondi C, et al. Symptoms of obsessive–compulsive disorder. Am J Psychiatry 1997;154:911–7.
- Nikolajsen KH, Nissen JB, Thomsen PH. Obsessive–compulsive disorder in children and adolescents: Symptom dimensions in a naturalistic setting. Nord J Psychiatry 2011;65:244–50.
- Storch EA, Larson MJ, Price LH, Rasmussen SA, Murphy TK, Goodman WK. Psychometric analysis of the Yale–Brown Obsessive–Compulsive Scale Second Edition Symptom Checklist. J Anxiety Disord 2010;24:650–6.
- Baer L. Getting control: Overcoming your obsessions and compulsions. Boston, MA: Little, Brown & Company; 1991.
- Steketee G, Frost R, Bogart K. The Yale–Brown Obsessive Compulsive Scale: Interview versus self-report. Behav Res Ther 1996;34:675–84.
- Federici A, Summerfeldt LJ, Harrington JL, McCabe RE, Purdon CL, Rowa K, et al. Consistency between self-report and clinician-administered versions of the Yale–Brown Obsessive– Compulsive Scale. J Anxiety Disord 2010;24:729–33.
- Matsunaga H, Hayashida K, Kiriike N, Maebayashi K, Stein DJ. The clinical utility of symptom dimensions in obsessive–compulsive disorder. Psychiatry Res 2010;180:25–9.
- Overduin MK, Furnham A. Assessing obsessive–compulsive disorder (OCD): A review of self-report measures. J Obsessive Compuls Relat Disord 2012;1:312–24.
- Abramowitz JS, Deacon BJ, Olatunji BO, Wheaton MG, Berman NC, Losardo D, et al. Assessment of obsessive–compulsive symptom dimensions: Development and evaluation of the Dimensional Obsessive–Compulsive Scale. Psychol Assess 2010;22: 180–98.
- Gönner S, Ecker W, Leonhart R, Limbacher K. Multidimensional assessment of OCD: Integration and revision of the Vancouver Obsessional–Compulsive Inventory and the Symmetry Ordering and Arranging Questionnaire. J Clin Psychol 2010;66:739–57.
- Clark DA, Antony MM, Beck AT, Swinson RP, Steer RA. Screening for obsessive and compulsive symptoms: Validation of the Clark–Beck Obsessive–Compulsive Inventory. Psychol Assess 2005;17:132–43.
- Gönner S, Ecker W, Leonhart R. The Padua Inventory: Do revisions need revision?Assessment 2010;17:89–106.
- Storch EA, Kaufman DA, Bagner D, Merlo LJ, Shapira NA, Geffken GR, et al. Florida Obsessive–Compulsive Inventory: Development, reliability, and validity. J Clin Psychol 2007;63:851–9.
- Burns GL, Keortge SG, Formea GM, Sternberger LG. Revision of the Padua Inventory of obsessive compulsive disorder symptoms: Distinctions between worry, obsessions, and compulsions. Behav Res Ther 1996;34:163–73.
- Anholt GE, van Oppen P, Emmelkamp PM, Cath DC, Smit JH, van Dyck R, et al. Measuring obsessive–compulsive symptoms: Padua Inventory-Revised vs. Yale–Brown Obsessive Compulsive Scale. J Anxiety Disord 2009;23:830–5.
- Aldea MA, Geffken GR, Jacob ML, Goodman WK, Storch EA. Further psychometric analysis of the Florida Obsessive–Compulsive Inventory. J Anxiety Disord 2009;23:124–9.
- Seol SH, Kwon JS, Shin MS. Korean self-report version of the Yale–Brown obsessive–compulsive scale: Factor structure, reliability, and validity. Psychiatry Investig 2013;10:17–25.
- Watson D, Wu KD. Development and validation of the Schedule of Compulsions, Obsessions, and Pathological Impulses (SCOPI). Assessment. 2005;12:50–65.
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive–Compulsive Inventory: Development and validation of a short version. Psychol Assess 2002;14:485–96.
- Bejerot S. Brief obsessive compulsive scale (BOCS). In: 11th European Psychiatric Association Congress. Vol. 17. Stockholm; 2002;161S.
- Insel TR, Murphy DL, Cohen RM, Alterman I, Kilts C, Linnoila M. Obsessive–compulsive disorder. A double-blind trial of clomipramine and clorgyline. Arch Gen Psychiatry 1983;40:605–12.
- First MB. Structured clinical interview for DSM-IV axis I disorders: SCID–I: Clinician version. Washington, DC: American Psychiatric Press; 1997.
- APA. Diagnostic and statistical manual of mental disorders (DSM-III-R), Third edition, revised edn. Washington, DC: APA (American Psychiatric Association); 1987.
- APA. Diagnostic and statistical manual of mental disorders (DSM-IV), Fourth edn. Washington, DC: APA (American Psychiatric Association); 1994.
- Spitzer RL, Williams, J.B.W, Gibbon, M. Structured Clinical Interview for DSM-III-R New York: New York State Psychiatric Institute, Biometrics Research; 1987.
- Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF. Meta-analysis of the symptom structure of obsessive–compulsive disorder. Am J Psychiatry 2008;165:1532–42.
- Pertusa A, Bejerot S, Eriksson J, Fernández de la Cruz L, Bonde S, Russell A, et al. Do patients with hoarding disorder have autistic traits?Depress Anxiety 2012;29:210–8.
- Ferrão YA, Shavitt RG, Prado H, Fontenelle LF, Malavazzi DM, de Mathis MA, et al. Sensory phenomena associated with repetitive behaviors in obsessive–compulsive disorder: An exploratory study of 1001 patients. Psychiatry Res 2012;197:253–8.
- Ruta L, Mugno D, D’Arrigo VG, Vitiello B, Mazzone L. Obsessive–compulsive traits in children and adolescents with Asperger syndrome. Eur Child Adolesc Psychiatry 2010;19:17–24.
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive–compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry 2010;15:53–63.
- Crino R, Slade T, Andrews G. The changing prevalence and severity of obsessive–compulsive disorder criteria from DSM-III to DSM-IV. Am J Psychiatry 2005;162:876–82.
- Reininghaus U, Priebe S. Measuring patient-reported outcomes in psychosis: Conceptual and methodological review. Br J Psychiatry 2012;201:262–7.