Abstract
A 59-year-old diabetic man was admitted for severe acute renal failure. Clinical signs were compatible with an acute tubular necrosis but no etiology was found. Kidney biopsy showed an osmotic nephrosis. Resumption of interrogatoire reveals consumption of Artemisia herba-alba accused in very few experimental studies to cause a lesion indicative of osmotic nephrosis.
CASE REPORT
In July 2009, a 59-year-old male mechanic was admitted to our unit for severe renal failure, whose serum creatine was 1260 μmol/L 6 mL/min and hyperkalemia level was 7.88 mmol/L.
He has diabetes mellitus and arterial hypertension from past 15 years. His usual medication was glibenclamide, metformin, and nifedipine. He had no known diabetic complications, especially, no proteinuria and his serum creatinine was 102 μmol/L (68 mL/mn) in February 2009.
One week prior to the admission, he had fever, asthenia, anorexia, vomiting, and bilateral lumbalia. A urinary examination requested by his family doctor showed a leukocyturia of 1300/mm3, a hematuria of 300/mm3, and a negative culture. He was prescribed paracetamol and ofloxacin with no improvement in his condition.
On physical examination, the patient presented no fever, a blood pressure of 150/90 mmHg, and an oliguria of 300 mL/24 hours. Urinalysis showed proteinuria (+) with no hematuria. Pulmonary examination showed cruces on the lower part of both lungs. Eye ground examination showed a moderate nonproliferative diabetic retinopathy. Electrocardiogram showed tenting of the T-waves.
Biological checklist: arterial pH: 7.2 arterial; bicarbonatemia: 7.3 mmol/L; oxygensaturation: 97%; glycemia: 0.6 g/L; hemoglobin: 12.2 g/L; plasmatic anion gap: 68 mmol/L; proteinuria: 2g/24 hours; urinary sodium: 87 g/L; urinary potassium: 10 mmol/L; plasma urea concentration: 29.9 mmol/L; urinary urea: 49.9 mmol/L. The rest of biology was unremarkable (hepatic features, lactic dehydrogenase, C protein kinase).
Renal duplex ultrasonography showed no vascular blockage, no pelvicaliceal dilation, a right kidney of 14 cm, and a left kidney of 15 cm in length. All medications were stopped; the patient was dialyzed and resuscitated. He remained oliguric for 5 days and necessitated three dialysis sessions.
It was evident that he had acute renal failure complicated by lactic acidosis because of metformin medication. Tubular injury was the likely etiology because of several features especially that of a urinary sodium to urinary potassium ratio greater than 1 and a urinary urea to serum urea less than 10.
No cause of acute tubular injury was found: there were no signs of shock and no nephrotoxic medication; although ofloxacin can cause interstitial injury. Also, there was no hemolysis or rhabdomyolysis.
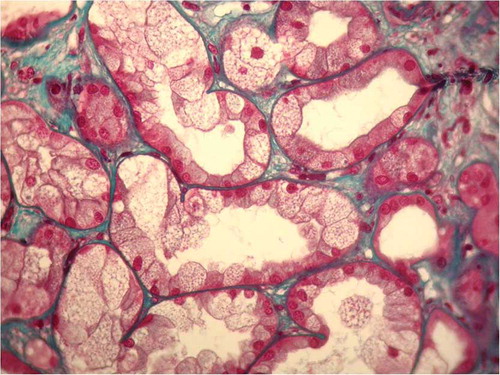
A kidney biopsy was performed and an osmotic nephrosis associated with a diabetic glomerusclerosis was concluded ( and ).
FIGURE 1. Renal biopsy specimen showed massive clear-cell transformation of the tubules; glomeruli showed a diffuse mesangial matrix increase and a thickening of basement membrane. It is also associated with tubular interstitial fibrosis (trichrome stain × 40).
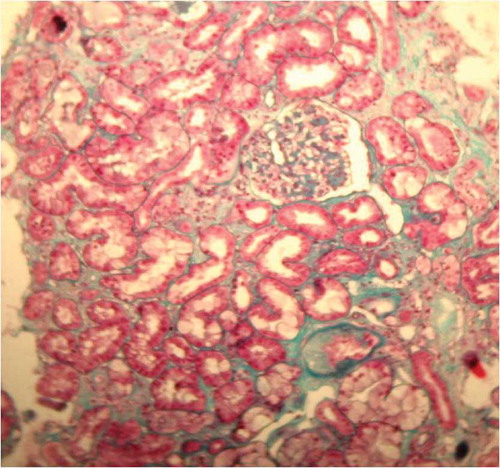
FIGURE 2. Proximal tubular cells are massively swollen with small vacuoles and nuclei are displaced toward the base of the cells in addition to isometric vacuolization (trichrome stain × 400).
To establish an etiologic diagnosis, we requestioned the patient and we found that he had taken an aqueous extract (two cups a day for two consecutive days) of Artemisia herba-alba.
Fifty days after a supportive therapy, the patient recovered a subnormal renal function (105 μmol/L:67 mL/mn). Artemisia herba-alba was not advised for our patient.
DISCUSSION
Osmotic nephrosis is rarely reported, although causative agents are frequently used. This is because it may develop and disappear with and without clinical signs.Citation1 Clinical signs are acute tubular necrosis – like inCitation1, so kidney biopsy is not usually practiced. Urinalysis may show tubular proteinuria or characteristic vacuolated tubular cells. Kidney ultrasound studies show no specific changes or, like in our patient, enlarged kidney.Citation2
Kidney biopsy is the gold standard of diagnosis. It shows a focal or sometimes a diffuse clear-cell transformation of proximal tubular epithelial cells showing isometric small vacuoles. Distal tubules and collecting ducts are frequently unchanged.Citation3 Careful examination is required for differential diagnosis, which includesCitation1: tubular calcineurin-inhibitor toxicity, ischemic damage, foam cells in lipid storage, potassium depletion, ethylene glycol intoxication, rapamycin therapy, diabetic hyperglycemia, and renal clear-cell carcinoma. Renal replacement therapy may be indicated in up to 34% of patients.Citation3
Causative agents are intravenous immune globulins with glucose- or derivative-based stabilizers,Citation4 mannitol,Citation2 dextran,Citation5 contrast mediaCitation6 hydroxyethyl starch, and glucose.Citation2 Discontinuation of the causative agent leads to recovery from osmotic nephrosis. Persistent chronic renal disease rarely occurs.Citation1 None of those agents was used by our patient.
Artemisia herba-alba is a very popular remedy in Tunisia (North Africa) and is locally known as chih. It is used in folk medicine as an antihelminthic, antispasmodic, antirheumatic, and antidiabetic agent. Many other species are used in Afro-Asian countries. There is no case of renal injury caused by Artemisia herba-alba in literature. Marrif et al.Citation7 reported mild hydropic degeneration in proximal convoluted tubules in rabbits and mice having an aqueous extract of Artemisia herba-alba. Adam et al.Citation8 reported small fatty vacuoles in the cells of the renal proximal convoluted tubules in rats fed on a diet consisting of 10% Artemisia abyssinica. This pathologic aspect is indicative of osmotic nephrosis. The mechanism whereby the plant constituents injure the kidney is unknown. The known renal effect of Artemisia herba-alba is a diuretic effect.Citation9 Further experimental investigations into the confirmation of the renal injury due to this plant and into the appropriate isolation and characterization of its active constituents are necessary for elucidating their modes of action.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Dickenmann M, Oettl T, Mihatsch MJ. Osmotic nephrosis: Acute kidney injury with accumulation of proximal tubular lysosomes due to administration of exogenous solutes. Am J Kidney Dis. 2008;51(3):491–503.
- Cornu P, Caulin C, Marsan C, Osmotic nephropathy: Specific iatrogenic disease or nonspecific tubular reaction? Sem Hop. 1973;49:1429–1430.
- Gras V, Andrejak M, Decocq G. Acute renal failure associated with intravenous immunoglobulins. Pharmacoepidemiol Drug Saf. 1999;8(Suppl. 1):S73–S78.
- Chacko B, John GT, Balakrishnan N, Osmotic nephropathy resulting from maltose-based intravenous immunoglobulin therapy. Ren Fail. 2006;28:193–195.
- Fillastre JP, Mignon F, Sraer JD, Acute reversible renal insufficiency after prolonged treatment with dextran. Presse Med. 1967;75:2535–2538.
- Moreau JF, Droz D, Noel LH, Tubular nephrotoxicity of water-soluble iodinated contrast media. Invest Radiol. 1980;15(Suppl. 6):S54–S60.
- Marrif HI, Ali BH, Hassen KM. Some pharmacological on Artemisia herba-alba (Asso.) in rabbits and mice. J. Ethnopharmacol. 1995;49:51–55.
- Adam SEI, Al-Qarawi AA, Elhag EA. Effects of various levels of dietary Artemisia abyssinica leaves on rats. Lab Anim. 2000;34:307–312.
- Zeggwagh NA, Farid O, Michel JB, Eddouks M. Cardiovascular effect of Artemisia herba-alba aqueous extract in spontaneously hypertensive rats. Methods Find Exp Clin Pharmacol. 2008;30(5):375–381.