Abstract
Temporary or permanent central venous catheter (CVC) insertion has been performed frequently for hemodialysis treatment. One of the most important long-term complications of CVC is the central venous occlusion (CVO). Treatment of CVO consists of percutaneous angioplasty (PTA), PTA and stent implantation, or surgical procedure for resistant occlusions. Clinical outcome and long-term results of the revascularization procedures are well documented. However, there is no clear information about acute medical complications of the procedures. High-output heart failure (HOHF) is associated with several diseases including chronic anemia, psoriasis, systemic arteriovenous fistula, sepsis, hypercapnia, multiple myeloma, and hyperthyroidism. Herein, we report a case of chronic kidney disease with CVO that developed acute HOHF immediately after the revascularization procedure (PTA and stenting).
INTRODUCTION
Temporary or permanent central venous catheter (CVC) insertion has been performed frequently for hemodialysis (HD) in patients with end-stage renal disease.Citation1 One of the most important long-term complications of CVC is the central venous occlusion (CVO).Citation2 HD patients with arteriovenous fistula (AVF) and without a previous history of a central venous catheterization may also develop CVO. Treatment of CVO consists of percutaneous angioplasty (PTA), PTA and stent implantation, or surgical procedure in the presence of resistant occlusion. Clinical outcome and long-term results of the revascularization procedures are well documented.Citation2 However, there is no clear information about acute medical complications of the procedures. Herein, we report a case of chronic kidney disease with CVO that immediately developed acute high-output heart failure (HOHF) following PTA and stenting procedure.
CASE REPORT
A 69-year-old female patient was admitted to our hospital with complaint of swelling, pain, and severe venous collateral on her left arm and left hemithorax. Her past medical history revealed the diagnosis of diabetes mellitus and hypertension for 20 years. Seven years earlier, she experienced unclassified acute renal failure and received HD treatment initially via left internal jugular CVC for 28 days and then via AVF created on left radial snuff box for 3 months. After this period, as her renal functions recovered, HD treatment was no longer needed. Six months earlier, she had experienced gradually increased swelling and pain, and collateral veins on her left arm and left hemithorax. At this period, she was on a treatment of insulin, nifedipine, and acetylsalicylic acid.
On admission, no abnormal findings except for venous collaterals, left internal jugular venous distention, and severe swelling on her left arm were observed on physical examination. Her blood pressure was 135/80 mmHg and pulse was 82 beats/min, regular. No thrill was observed on her old AVF created on left radial snuff box. Laboratory findings were hemoglobin 10 g/dL, creatinine 2.62 mg/dL, and fasting blood glucose 165 mg/dL. Urine examination revealed 3.7 g/d proteinuria. Arterial blood gas analysis and oxygen saturation were not measured.
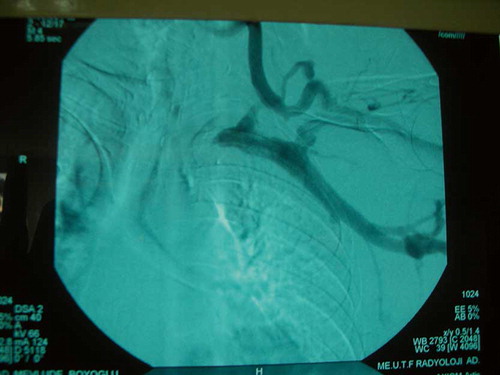
After initial evaluation, fistulography was performed and left brachiocephalic vein occlusion was detected (). During fistulography procedure, PTA and stent implantation was performed successfully (). Two hours following the procedure, the patient experienced acute respiratory distress. At this time, her physical examination revealed bilateral jugular venous distention at 45°, bilateral crackles at the lower fields of the lung, and tachycardia. Chest X-ray revealed pulmonary edema. Arterial blood gas analysis revealed the following values: pH = 7.29, PO2 = 65 mmHg, PCO2 = 29 mmHg, oxygen saturation = 78%, and HCO3 = 21 mEq/L. On echocardiographic examination, hyperdynamic heart, septal hypertrophia (1.5 mm), and mild mitral regurgitation were detected. Left and right ventricular contractility was good and ejection fraction (EF) was 60%. Cardiac index was calculated as 5.2 L/min/m2. After initial evaluation, nasal oxygen, intravenous loop diuretic, and nitroglycerine were started and tourniquet was applied on her left arm proximal to AVF. Respiratory distress rapidly improved after 15 min of medical treatment. Tourniquet was gradually terminated within 2 h. All the arterial blood gas parameters returned to normal values within 8 h. As the patient remained asymptomatic following 36 h, she was discharged. She was well and asymptomatic after 3 months of follow-up.
DISCUSSION
CVSs are suitable in the setting of acute kidney injury or as an intermediate measure while waiting for the maturation of a permanent arteriovenous access for chronic HD. These devices could be complicated in many ways; one of the major complications is CVO.Citation2 Most important risk factors of CVO are catheter duration time, repeated catheter insertion, long-term dialysis via CVC, catheter-related infections, and left side inserted catheters.Citation2 CVO may also develop in HD patients without a previous history of CVC.Citation3 Turbulence of high flow rate AVFs, especially more proximal AVFs, may cause a venous injury, intimal hyperplasia, and thrombosis.Citation3 In our patient, risk factors for the development of CVO consisted of previous history of placing a subclavian HD catheter and having an AVF.
Only a small portion of patients with CVO become symptomatic. They present with swelling and pain on ipsilateral extremity and chest wall. Venous hypertension and swelling gradually increase, especially in patients with active AVF. HD sessions may cause pain on the ipsilateral extremity. Our patient experienced unclassified acute renal failure and received HD treatment for 4 months via both CVC and AVF. About 6 years after the termination of HD treatment, she had gradually become symptomatic over 6 months.
Treatments of CVO consist of PTA, PTA and stent implantation, or surgical procedure in the presence of resistant occlusion. Clinical outcome and long-term results of the revascularization procedures are well documented.Citation2 However, there is no clear information about the acute medical complications of the procedures. To the best of our knowledge, this is the first case report reporting the development of acute HOHF immediately following the correction of CVO via PTA and stent implantation.
HOHF is defined as cardiac index > 3.9 L/min/m2 and associated with several diseases including chronic anemia, psoriasis, systemic AVF, sepsis, hypercapnia, multiple myeloma, and hyperthyroidism.Citation4 There are no data about the incidence or prevalence of HOHF in such conditions. The underlying primary physiological problem is of reduced systemic vascular resistance due to either arteriovenous shunting or peripheral vasodilatation. On the other hand, HOHF may occur physiologically in the presence of anxiety, stress, exercise, pregnancy, and fever.Citation5 In our patient, except mild anemia, there was no physiological or pathological condition which may be associated with HOHF. Data about HOHF are very rare and based on case reports.Citation4 Proximal AVF, AVF flow rate over 30% of cardiac output, moderate to severe anemia, male gender, and a previous history of heart disease are the risk factors for the development of HOHF in HD patients.Citation6 Diagnosis is made by detection of underlying related factors, heart failure symptoms, chest X-ray findings, blood gas analysis, and echocardiographic findings. Systolic performance of the patients with HOHF is protected (EF > 45–50%) and mixed venous oxygen saturation (MVOS) is >75%. In our patient, EF, cardiac index, and MVOS were 60%, 5.2 L/min/m2, and 78%, respectively. Treatment of CVO, sudden increase in venous drainage, older age, mild anemia, and chronic kidney disease might trigger the development of HOHF in our patient.
Treatment approaches of the HOHF are generally based on the case reports. Renin–angiotensin system blockers and beta blockers can cause deterioration in HOHF.Citation4 Furthermore, treatment options of low-output heart failure can cause worsening of the HOHF symptoms. In our patient, we used nitroglycerine and low-dose loop diuretic and applied tourniquet on the left upper arm and her symptoms disappeared within a short period of time.
In conclusion, based on our case report, it should be kept in the mind that treatment of CVO with serious venous congestion may result in the development of HOHF. Before the revascularization procedure, cardiac functions and factors associated with the development of HOHF should be evaluated carefully in HD patients with CVO. Furthermore, reporting of the post-procedural acute complications will improve the awareness and preventive measures.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Cetinkaya R, Odabas AR, Unlu Y, Selcuk Y, Ates A, Ceviz M. Using cuffed and tunnelled central venous catheters as permanent vascular access for hemodialysis: A prospective study. Ren Fail. 2003;25(3):431–438.
- Yevzlin AS. Hemodialysis catheter-associated central venous stenosis. Semin Dial. 2008;21(6):522–527.
- Oguzkurt L, Tercan F, Yildirim S, Torun D. Central venous stenosis in hemodialysis patients without a previous history of catheter placement. Eur J Radiol. 2005;55(2):237–242.
- Mehta PA, Dubrey SW. High output heart failure. Q J Med. 2009;102:235–241.
- Carbillon L, Uzan M, Uzan S. Pregnancy, vascular tone, and maternal hemodynamics: A crucial adaptation. Obstet Gynecol Surv. 2000;55(9):574–581.
- Mac Rae JM, Pandeya S, Humen DP, . Arteriovenous fistula-associated high-output cardiac failure: A review of mechanisms. Am J Kidney Dis. 2004;43(5):e17–e22.