Abstract
Objective: Tunneled cuffed dual-lumen catheters (TCCs) are commonly used for vascular access in hemodialysis (HD) patients. Catheter-related bloodstream infection (CRBSI) is the major problem leading to morbidity and mortality. We investigated whether 26% NaCl solution has any favorable effect on the infections and thrombosis caused by HD catheters. Methods: TCCs were locked with either 26% NaCl and heparin or standard heparin. The primer end point of the study was the CRBSI or thrombosis of the TCC. We compared the antimicrobial activity of the NaCl solutions (6.5%, 13%, 26%) with 0.9% NaCl solution by time–kill kinetic assay. All tests were performed in triplicate by incubation of test fluids with Escherichia coli, Pseudomonas aeruginosa, Staphylococcus aureus, and Staphylococcus epidermidis. Results: The mean catheter survival was significantly higher in the 26% NaCl and heparin group (129.5 ± 50.1 catheter days to 103.3 ± 59.8, p = 0.008). CRBSI rates (10–15.4%) did not differ significantly between the two groups (p = 0.54). The hypertonic 13% NaCl solution had bactericidal effects on E. coli and P. aeruginosa, but had bacteriostatic effect on S. aureus and S. epidermidis. Conclusion: In this study we demonstrated that the 13% NaCl solution and more hypertonic NaCl solutions revealed potent in vitro antimicrobial properties against all checked Gram-negative microorganisms.
INTRODUCTION
The best long-term method for hemodialysis (HD) blood access is to create a fistula and, when that is impossible, an alternative is to create an arteriovenous graft.
Because it is not possible to use fistulas for permanent vascular access immediately after they are surgically created, tunneled cuffed dual-lumen catheters (TCCs) are the first choice of vascular access devices in a significant number of patients. The major complication that limits their long-term use is catheter thrombosis or infections.
Central venous catheter-related bloodstream infection (CRBSI) is a serious problem leading to mortality and morbidity among HD patients. The incidence ranges from 2.5 to 5.5 episodes/1000 catheter days or 0.9–2 episodes per patient year in patients who use them for vascular access.Citation1 About one-third of CRBSI episodes require inpatient hospitalization and the mortality rate is about 5–10% for each CRBSI event.Citation2
Despite the beneficial effect of antibacterial catheter lock solutions (CLSs) on catheter-related bacteremia and associated morbidity and mortality, there are many side effects with their prophylactic use. The spillage of up to 15% of the catheter volume into the patients’ blood can result in the development of antibiotic-resistant bacteria, allergic reactions due to the antibiotic, systemic toxicity of the antibiotic, and systemic anticoagulation due to heparin and citrate.Citation3
Because of the growing number of cases of antibiotic resistance, new CLSs rather than antibiotics are being studied. Antiseptic CLSs show their effects by physical pathways and are routinely used in some centers, but the high costs limit their use.
Hypertonic NaCl solution has a different mechanism of action. The high tonicity of 26% NaCl has a bacteriostatic or bactericidal effect on microorganisms and it has been shown that it prevents the development of infections and promotes recovery when it is applied locally to the injury site.Citation4 According to previous observations that hypertonic saline impairs motility and blocks the spreading of Pseudomonas aeruginosa, and as a result of the beneficial effects of hypertonic saline (7%) aerosols in cystic fibrosis patients, it has been proposed that it can be used in other lung diseases.Citation5
There are no data in the literature on the antimicrobial properties and the prophylactic use of 26% NaCl and heparin in combination as a CLS. In our study, we investigated whether 26% NaCl solution can prevent CRBSI and whether 26% NaCl and heparin combination therapy has any favorable effect on the infections and thrombosis caused by TCC.
MATERIALS AND METHODS
This study is composed of two parts. In the laboratory assessment of the study, we used bacteria tests and time–kill kinetic assay to determine the antibacterial activity of the solutions. In the clinical part of the study, the TCCs of the HD patients were locked with either of the solutions and in every HD session, the TCCs and patients were evaluated if CRBSI or thrombosis occurred.
Part 1
We undertook a randomized controlled trial comparing the efficacy of 26% NaCl solution and heparin versus standard heparin as CLS for HD catheters. All the patients were recruited between August 2009 and August 2010 from the dialysis unit in the Department of Nephrology, Erciyes University, Kayseri, and from associated satellite dialysis units.
Inclusion criteria were as follows: adult men and women (age >18 years) receiving HD through a central venous TCC were eligible. This included patients with acute renal failure and those with chronic end-stage renal disease, both incident and prevalent.
Patients were excluded if they were less than 18 years old, were pregnant, had active sepsis, were on antibiotic therapy, or if they needed the reinsertion of a TCC through the same exit site or a new entry site or if the TCC was used for another purpose other than HD.
The primary outcome measure was defined as the rate of CRBSI per 1000 catheter days in patients using CLSs versus heparin-only group and rates of catheter thrombosis (defined as thrombosis or need for thrombolytic therapy or removal of the TCC because of flow problems defined as a blood flow rate of <200 mL/min for three consecutive dialysis sessions).
The TCCs [Hemo-Cath, 24 cm (used for the right jugular vein) or 28 cm (used for the left jugular vein), 14.5 F Medcomp, Medical Components, Inc. Harleysville, PA, USA] used for dialysis were inserted by experienced radiologists under direct image guidance.
All patients had a chlorhexidine body wash and strict asepsis was used before TCC insertion. The exit site was covered with a transparent, oxygen permeable dressing. The TCC exit sites were inspected at each dialysis and cleaned with chlorhexidine or iodine and covered with a new transparent dressing after each treatment. The TCC dressings and the application of povidone-iodine ointment at the TCC exit site were carried out by trained dialysis staff, wearing facial masks, sterile gloves, and a sterile gown. Block randomization using random number tables was performed. The randomization procedure was carried out independent of the place of TCC insertion. The study was double-blinded and only the nurses knew in which group the patient was. The study was approved by the Ethics Committee of Erciyes University and all subjects gave written informed consent.
Patients were randomly assigned to have both lumens of their TCC locked with either unfractionated sodium heparin (5000 U/mL heparin in a 3 mL syringe) or 26% NaCl solution and heparin (1 mL of 26% NaCl and 500 U/mL heparin in a 3 mL syringe).
After HD treatment had been completed, each lumen of the TCC was flushed with 10 mL of 0.9% NaCl and locked with the CLS using a volume exactly equivalent to the internal volume of the lumen noted on the TCC. The syringe had to be filled with the amount of locking solution necessary to lock one lumen of the TCC to prevent accidental infusion of the locking solution.
The patients’ demographic data included age, gender, etiology of renal disease, use of warfarin therapy, and history of malignancy, diabetes, and cardiovascular disease. The time of insertion of the TCC, and time for TCC removal were recorded. If CRBSI or thrombosis occurred, the day of complication was recorded and the patient was excluded from the study.
Part 2
Bacteria tests
The antibacterial properties of the 26% NaCl solution were tested on four standardized reference strains from the American Type Culture Collection: on Gram-positive strains of Staphylococcus aureus (ATCC 25923) and Staphylococcus epidermidis (ATCC 12228), and on Gram-negative strains of P. aeruginosa ATCC (27853) and Escherichia coli (ATCC 25922).
Single colonies from fresh trypticase soy agar plates with sheep blood were used for preparation of overnight inocula. The 26% NaCl solution was manufactured from raw base by the Department of Pharmacy at Erciyes University’s Medical Center in Kayseri, Turkey. The solutions were heat sterilized for 16 min at 121°C and the pH was controlled at between 6.4 and 7.5. The 0.9% NaCl solution was used as the control solution.
Time–kill kinetic assay
The antimicrobial activity of the solutions was investigated by time–kill methods, essentially performed according to the National Committee for Clinical Laboratory Standards Guidelines.Citation6
Inocula were prepared overnight to match 0.5 McFarland standards and then further diluted 1:10 with Mueller Hinton broth to a final inoculum of 105 colony-forming units per mL (cfu/mL). Each microbial suspension of 20 μL was added separately to each 2000 μL of 26%, 13%, 6.5%, and 0.9% NaCl solutions. The final bacterial concentration of 103 cfu/μL of the test organism was achieved and the time–kill curves of the control solution were made at this concentration.
A 100 μL of the suspension was taken from the tubes at time 0 and was placed on 5% sheep blood agar and subsequently incubated overnight at 35°C. Samples were taken at time intervals of 0, 8, and 24 h for plating as described above. The sheep blood agars were again incubated overnight at 35°C. Afterward the colonies were counted and recorded, taking the dilution factor into account. Time–kill curves were constructed from the calculated cfu/μL. Each experiment was repeated 3 times.
The bacterial growth was compared between the four different NaCl solutions (i.e., control vs. experimental) and expressed as the natural logarithm of the ratio. If the colony count reduced ≥3 log due to the initial value, it was defined as bactericidal activity (99.9% death). If the growth reduction was 2 log, then it was defined as bacteriostatic activity (99.9% growth inhibition), and growth reduction ≤1 log was accepted as insignificant.
Assessment of infection
CRBSI was defined according to the criteria of the Centers for Disease Control.Citation7 The following were the diagnostic criteria: CRBSI defined as fever (temperature >38°C) and one positive blood culture result with no other obvious source of infection (at least two blood cultures either from the TCC or from a peripheral vein were taken) or possible blood stream infection defined as defervescence after removal of TCC in the absence of laboratory confirmation of blood stream infection in a symptomatic patient with no other apparent source of infection. The incidence of CRBSI and catheter thrombosis was reported as episodes/1000 catheter days.
Exit-site infection was defined as the development of redness or tenderness and/or induration within 2 cm of the exit site with or without a purulent exudate around the site not resulting from residual stitches or microbiologic exit-site infection where the exudate yields a microorganism on culture.
Statistical analysis
All computations were performed using SPSS software (version 15.0; SPSS Inc., Chicago, IL, USA). Data are presented as mean ± SD. The distribution of the parameters was analyzed by Shapiro–Wilk test. Independent t-tests were used to compare continuous variables between groups. Skewed variables were described using median (range) and were compared using the Mann–Whitney U test.
A Kruskal–Wallis test was used to compare the effect of four different NaCl solutions on the bacterial growth of the tested bacteria. A χ2-test was used to compare the categorical variables among groups. p-Values of <0.05 were considered significant.
RESULTS
Part 1
Of 56 eligible patients, 26 patients were randomized to the 26% NaCl group and 30 patients to the standard heparin group (). The baseline characteristics of the patients were similar in the two treatment groups (). Patients were followed up for 3368 catheter days in the 26% NaCl and heparin group and for 3099 catheter days in the standard heparin group. The groups differed significantly with respect to catheter days, being more prominent in the 26% NaCl and heparin group. The mean TCC survival was significantly higher in the 26% NaCl and heparin group than in the heparin group (129.5 ± 50.1 catheter days to 103.3 ± 59.8 catheter days, p = 0.008).
Table 1. Baseline characteristics of patients with tunneled hemodialysis (HD) catheters.
All the TCCs (n = 56) were double-lumen polyurethane TCC and most of them were jugular. Only a limited number of subclavian TCCs (3 of 56; 5%) were used in the study and no femoral TCCs were used.
During the study follow-up period, none of the patients died (from randomization to CRBSI or censored event). A total of three episodes of CRBSI occurred in the patients who were randomized to the heparin-locking group (3 of 30) compared with 4 patients who were assigned to the 26% NaCl and heparin-locking group (4 of 26). The majority of infections (42.8%) were caused by coagulase-positive staphylococci, and S. epidermidis accounted for 14.2% of the infections (). The CRBSI rates (10–15.4%) did not differ significantly between the two groups (p = 0.54). The incidence of CRBSI was 1.1 episodes/1000 catheter days in the 26% NaCl and heparin group and 0.96 episodes/1000 catheter days in the heparin group (p > 0.05).
Table 2. Microorganisms causing infections.
Table 3. The incidence and thrombosis days of the groups.
Time to infection was 98.2 ± 52.4 days in the 26% NaCl and heparin group and 92.3 ± 88.6 days in the heparin group. Time to thrombosis was 79.7 ± 24.4 days in the patients who were randomized to the 26% NaCl and heparin-locking group and 51.6 ± 21.0 days in the standard heparin group. Time to infection and time to thrombosis did not differ significantly between the groups (p = 0.92; p = 0.16).
Insufficient dialysis due to flow problems because of intraluminal thrombosis occurred in 4 of the 26 TCCs assigned to the 26% NaCl and heparin-locking group and the TCCs had to be removed. Three of the 30 TCCs assigned to the heparin-locking group also had to be removed because of persistent flow problems (15.4% to 10%). The percentage of TCC that had to be removed prematurely did not differ significantly when the two groups were compared (p = 0.54) ().
Part 2
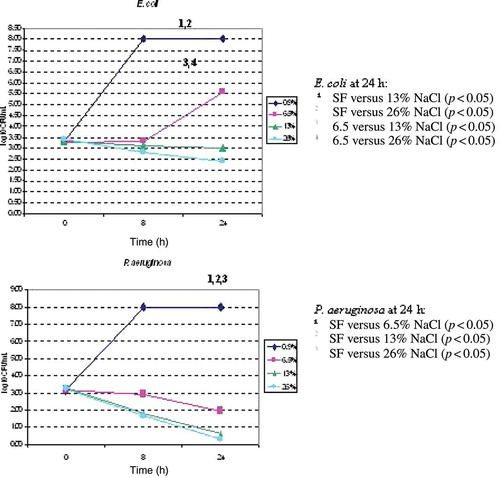
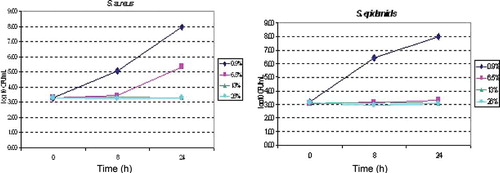
The time–kill curves for the four tested bacteria in all concentrations of the NaCl solutions are presented in and .
NaCl 6.5% and the more concentrated NaCl solutions showed a statistically significant bactericidal effect (downward-directed slope) on P. aeruginosa and E. coli over 8 h (p = 0.028 and 0.033). However, the solutions had a bacteriostatic effect on the growth of Gram-positive bacteria at 8 h.
When the colonies were compared with 0.9% NaCl solution at 24 h, the 13% NaCl and the 26% NaCl solutions showed a statistically significant bactericidal effect (the slope approached 0 at 24 h) on E. coli and P. aeruginosa (p = 0.019 and 0.030). Only a modest reduction (2 log) in the living cells of S. aureus and S. epidermidis could be achieved after 24 h incubation with the three NaCl solutions, and the effect was defined as bacteriostatic (p = 0.096 and 0.085).
The 6.5% NaCl solution showed significant growth inhibition of P. aeruginosa at 8 h (colonies started to decrease at 8 h and the effect persisted over 24 h) (p = 0.028). The growth of the Gram-negative strains of E. coli was also significantly affected at 8 h by the 6.5% NaCl solution, but the bactericidal effect did not persist, and the effect of the 6.5% NaCl solution remained bacteriostatic over 24 h (p = 0.019).
DISCUSSION
CRBSI is associated with high mortality and morbidity rates among HD patients. Strict hygienic rules, prophylactic use of topical agents, tunneling of central venous catheters, cuffing of the catheter hub, and the use of CLS achieved a reduction in the incidence of CRBSI and associated morbidity and mortality.Citation8
The most important source of CRBSI is intraluminal colonization of the TCC and the development of a biofilm. In order to prevent the interdialytic clotting of TCC, they are filled with heparin solution after each use.Citation9 Heparin exerts its anticoagulant effect mainly through the activation of antithrombin III, and it is effective in concentrations as low as 1 U/mL blood. However, between uses of a TCC, blood can enter the tip of the TCC and wash out residual heparin, resulting in clotting of the TCC. Heparin has neither the ability to lyse preformed thrombi or fibrin sheaths nor any antibacterial properties.Citation10
The risk of CRBSI can be diminished if the solution prevents the formation of a biofilm. In vitro studies have shown that approximately 100-fold higher concentrations of antibiotics are effective against the microbes in the tunnel of the catheters.Citation11 Moreover, antimicrobial solutions like taurolidine, trisodium citrate 30%, and ethanol 70% also showed bactericidal effects in in vitro studies.Citation11 However, there are no data in the literature on the use of 26% NaCl solution as a CLS.
In this study we examined the in vitro antimicrobial activity of different concentrations of NaCl solutions (0.9%, 6.5%, 13%, and 26%) on four bacterial strains commonly found in CRBSI. We found that the hypertonic 13% NaCl solution had bactericidal effects on E. coli and P. aeruginosa over 24 h, but had a bacteriostatic effect on S. aureus and S. epidermidis. Our results are in concordance with the study of Weijmer et al. In that study they compared different concentrations of citrate solutions with 0.9%, 6.1%, and 12.2% NaCl solutions. They found that the 12.2% NaCl solution progressively reduced the E. coli and P. aeruginosa count to an undetectable level after 24 h (colonies started to decrease at 4 h and the slope approached 0 at 24 h).Citation12 As we repeated the experiments 3 times, we observed that the exposure of E. coli and P. aeruginosa to 13% and 26% NaCl solutions for 24 h twice resulted in the total elimination of living cells. In addition, after 8 h treatment, in two of the repeated experiments the Gram-negative strains were completely killed and viable bacteria were not detected with both of the solutions described above. In the study of Weijmer et al., they found that neither of the NaCl solutions were effective on Gram-positive strains, but in our study when the solutions were compared with the control solution, we demonstrated that all of them showed a bacteriostatic effect on Gram-positive bacteria.
In 2004, there were 308,000 HD patients in the United States and of these patients 25%, or 77,000, used dialysis catheters for vascular access. The results of several trials on CLS demonstrated a prevalence of CRBSI of approximately 4/1000 patient days in these patients.Citation13 In our study we compared a 26% NaCl and heparin combination with standard heparin. Although the heparin concentration in the combination group was 10 times lower than the standard heparin group, the CRBSI and thrombosis rates did not differ significantly between the two groups. CRBSI prevalence per 1000 catheter days was 1.1 in the 26% NaCl and heparin-locking group and 0.96 in the heparin-locking group (p > 0.05). The percentage of TCC that had to be removed prematurely was 15.4% in the combination group and 10% in the heparin group (p = 0.54).
CRBSI rates are approximately 35% in a 3-month period but the incidence rises to 48% when the TCCs are used for 6 months.Citation14 Although in our study the TCC stayed in for a longer period in the 26% NaCl and heparin group than in the standard heparin group (129.5–103.3 catheter days), the difference did not cause an increase in the CRBSI or thrombosis rates. This may be due to the preventive effect of hyperosmolar NaCl as a CLS.
In a systematic review and meta-analysis of randomized controlled trials, antibiotic CLSs and two nonantibiotic antimicrobial CLSs were analyzed (1 trial with taurolidine and citrate and 4 with 30% citrate solution). The antibiotic CLS used in these trials was gentamicin in 3 trials, gentamicin and citrate in 3 trials, gentamicin and vancomycin in 1 trial, gentamicin and cefazolin in 1 trial, cefotaxime in 2 trials, and minocycline with ethylene diamine tetra acetic acid in 2 trials. It has been reported that when interventions were compared with heparin as CLS, they statistically significantly reduced infection and catheter removal rates in the range of 50–100% (except for the citrate and taurolidine trial which showed a nonsignificant reduction in infection-related outcomes).Citation1
Gentamicin is not effective against staphylococcal bacteria in normal serum concentrations, but when it is employed as a CLS it reaches high concentrations in the intraluminal side of the catheter and has a toxic effect on these bacteria. The most common solutions are gentamicin–citrate and gentamicin–heparin combinations. In a randomized controlled trial, gentamicin 5 mg/mL and 5000 U/mL heparin were used and gentamicin significantly reduced the CRBSI rates (0.3/1000 vs. 4/1000 catheter days).Citation13 It is known that gentamicin–heparin combinations are considered to be incompatible because of solubility problems. When they are used as a CLS, visual precipitation occurs, but this complication was not seen in the three previously mentioned studies.Citation15–17 In our study we used a 26% NaCl solution, and no other concentration, because of the solubility problem we observed (crystallization occurred) with more hyperosmolar NaCl solutions.
Ototoxicity is another issue when gentamicin solutions are used for catheter locking. This can be seen when a concentration of amikacin as low as 10 mg/mL is used.Citation15 To avoid this complication, authors recommend the use of very small (5 mg/mL) concentrations of gentamicin in combination with heparin as CLS.Citation15
Another concern when antibiotics are used for TCC locking is the development of antibiotic-resistant bacteria. Although this is a well-known result of long-term antibiotic use, it was stated in one gentamicin–heparin CLS study that no resistance was seen despite a 1-year follow-up.Citation18 In this study we used a hyperosmolar NaCl solution. It is known that bacteria cannot develop resistance to this solution because hyperosmolar NaCl solution exerts its effects by the osmotic pathways.
The instillation of TCC with citrate is often used in HD centers to reduce CRBSI rates. In an in vitro study, it was concluded that 30% citrate had an inhibitory effect on microbial growth and it was the most potent antimicrobial-locking solution when compared with other citrate concentrations.Citation2 In this concentration, citrate has anticoagulant and antimicrobial effects. That study demonstrated that citrate statistically significantly reduced CRBSI rates. The most important side effect of citrate when it is used in high concentrations is the spillage of citrate into the systemic circulation causing hypocalcemia and related ventricular arrhythmia and sudden cardiac death. A total of 46.7% of citrate solutions have not been available in HD centers in the United States since April 2000 because of a case of cardiac arrest following the instillation of this solution.Citation19 However, there were no such reported events in the Netherlands, although over 20,000 doses of lower concentration citrate-prefilled syringes were used for catheter locking.Citation13 Patients complain of metallic taste or perioral paresthesias immediately after TCC locking with citrate and symptoms do not resolve with the installation of smaller volumes of catheter lock.Citation13 Another complication that limits the use of citrate locking is the bleeding related to systemic leak and when it is used in lower volumes, this leads to thrombosis of the catheter and effects catheter survival.Citation13 In our study we did not observe any side effects for the 26% NaCl solution. If inadvertent instillation of the solution occurred, the total volume of the systemic leak would equal 1/10 of the daily salt intake of an individual, and this is not harmful.
In our study, in the 26% NaCl and heparin group (n = 26), patients were followed up for 3368 catheter days; catheter thrombosis was found in four patients and CRBSI was assessed in four. In the standard heparin group (n = 30), patients were followed up for 3099 catheter days; thrombosis was observed in three patients and infection in three. Although the patients in the combination group were followed up for a longer period, no difference occurred between the groups for thrombosis or CRBSI rates, and time to thrombosis or time to infection. We did not observe any of the side effects seen in other CLSs that are presently available. NaCl does not lead to antibiotic resistance because its antimicrobial effects arise from hyperosmolality. Despite the 10-fold reduction in the heparin concentration of the combination group, lower concentrations of heparin did not enhance the thrombosis rates of the combination group. This is perhaps due to another mechanism of the NaCl solution rather than hyperosmolality. To use heparin in lower concentrations reduces costs and it is also possible to prevent the bleeding complications due to heparin in this way.
In most countries, CLS cannot be used because of the lack of reimbursement. Gentamicin-containing solutions are the most preferred CLS because of their low cost, but antibiotic resistance limits their use. Citrate-containing CLSs seem to be the ideal solutions but obstacles to their use have not yet been overcome.
In conclusion, the objective of our study was to assess the efficacy of 26% NaCl and heparin CLSs for the prevention of catheter-associated infections and thrombosis in patients undergoing HD. This study demonstrated that the 13% NaCl and more hypertonic NaCl solutions revealed potent in vitro antimicrobial properties against all checked Gram-negative microorganisms and showed a bactericidal effect on E. coli and P. aeruginosa and a bacteriostatic effect on S. aureus and S. epidermidis. This is a promising finding as to the use of the solution as a CLS. However, our results showed that, despite the antibacterial effects of hypertonic NaCl, it was not superior to heparin as a CLS. Our study has several limitations: first, the study included a relatively small number of participants and second, the number of end points for the outcome analysis was small; this may have reduced the strength of the study. The long-term effects of hypertonic NaCl solution on the TCC material are not known; therefore, further investigations in larger, prospective, randomized, blinded clinical trials are necessary for the use of NaCl solutions as a CLS.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Yahav D, Rozen-Zvi B, Gafter-Gvili A, Leibovici L, Gafter U, Paul M. Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: Systematic review and meta-analysis of randomized, controlled trials. Clin Infect Dis. 2008; 47:83–93.
- Weijmer MC, van den Dorpel MA, Van de Ven PJ, . Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J Am Soc Nephrol. 2005;16:2769–2777.
- Polaschegg HD, Shah C. Overspill of catheter locking solution: Safety and efficacy aspects. ASAIO J. 2003;49:713–715.
- Mangete ED, West KS, Blankson CD. Hypertonic saline solution: An effective wound dressing solution. East Afr Med J. 1993;70:104–106.
- Havasi V, Hurst CO, Briles TC, . Inhibitory effects of hypertonic saline on P. aeruginosa motility. J Cyst Fibros. 2008;7:267–269.
- National Committee for Clinical Laboratory Standards. Performance Standards for Antimicrobial Disk Susceptibility Tests (Approved Standard M2-A5). Villanova, PA: National Committee for Clinical Laboratory Standards; 1993.
- Dogra GK, Herson H, Hutchison B, . Prevention of tunneled hemodialysis catheter-related infections using catheter-restricted filling with gentamicin and citrate: A randomized controlled study. J Am Soc Nephrol. 2002;13:2133–2139.
- Lok CE, Stanley KE, Hux JE, Richardson R, Tobe SW, Conly J. Hemodialysis infection prevention with polysporin ointment. J Am Soc Nephrol. 2003;14:169–179.
- Schwab SJ, Beathard G. The hemodialysis catheter conundrum: Hate living with them but can’t live without them. Kidney Int. 1999;56:1–17.
- Gagnon RF, Harris AD, Prentis J, Richards GK. The effects of heparin on rifampin activity against Staphylococcus epidermidis biofilms. Adv Perit Dial. 1989;5:138–142.
- Allon M. Prophylaxis against dialysis catheter-related bacteremia: A glimmer of hope. Am J Kidney Dis. 2008;51:165–168.
- Weijmer MC, Debets-Ossenkopp YJ, Van De Vondervoort FJ, ter Wee PM. Superior antimicrobial activity of trisodium citrate over heparin for catheter locking. Nephrol Dial Trans. 2002;17:2189–2195.
- Bleyer AJ. Use of antimicrobial catheter lock solutions to prevent catheter-related bacteremia. Clin J Am Soc Nephrol. 2007;2:1073–1078.
- Lee T, Barker J, Allon M. Tunneled catheters in hemodialysis patients: Reasons and subsequent outcomes. Am J Kidney Dis. 2005;46:501–508.
- McIntyre CW, Hulme LJ, Taal M, Fluck RJ. Locking of tunneled hemodialysis catheters with gentamicin and heparin. Kidney Int. 2004;66:801–805.
- Zhang P, Zhang W, He Q, . A randomized controlled study on prevention of cuff-tunneled catheter related bacteremia with gentamicin-heparin lock solution: The metaphase result [Abstract]. J Am Soc Nephrol. 2006;17:SA-PO073.
- Feely T, Copley A, Bleyer AJ. Catheter lock solutions to prevent bloodstream infections in high-risk hemodialysis patients. Am J Nephrol. 2007;27:24–29.
- Fluck R, McIntyre C, Taal M. A one-year experience single center with antibiotic locking for tunneled venous catheters [Abstract]. J Am Soc Nephrol.2006;17:SA-PO069.
- FDA issues warning on tricitrasol dialysis catheter anticoagulant. Available at: http://www.fda.gov/bbs/topics/ANSWERS/ANS01009.html. Accessed July 26, 2007.