Abstract
We report the fifth, to our knowledge, published case of spontaneous intraperitoneal bladder rupture after normal, vacuum-assisted in this occasion, vaginal delivery of a 29-year-old female patient. Diagnosis was established not by imaging or intraoperative findings, but, rather, by the examination and comparison of patient’s blood, urine, and peritoneal fluid urea and creatinine levels, which, due to the patient’s delayed referral and sequent development of uroperitoneum and hyponatremic renal pseudofailure, were abnormal and characteristic of her medical condition. The patient was successfully managed conservatively and was discharged the sixth day after admission. Due to the rare nature of such medical condition and based on the relative literature, we propose a diagnostic and management algorithm for such cases.
INTRODUCTION
Although intraperitoneal bladder rupture following a cesarean section is a rather rare but well-established complication,Citation1 spontaneous rupture of urinary bladder following normal vaginal delivery still remains a diagnostic and therapeutic challenge due to lack of current published literature and, of course, the extreme rarity of the event. We report a case of spontaneous rupture of the urinary bladder following vaginal, vacuum-assisted, delivery complicated with massive uroperitoneum and hyponatremic renal pseudofailure.
CASE REPORT
A 29-year-old woman with no prior medical history presented with acute abdominal pain and gradually progressing distention 7 days following a vacuum-assisted vaginal delivery. Upon arrival, her abdomen was extremely distended with clinical signs of severe ascitic fluid present, as well as abdominal tenderness, minimal bowel sounds, and respiratory distress (tachypnea). The delivery, although successful, was prolonged, and the whole labor process lasted over 29 h. It was the patient’s first child, the pregnancy lasted approximately 40 weeks (healthy, full-term baby), and no serious complications were recorded during this period. After delivery, the patient complained of lower abdominal pain with radiation to her back, a gradually progressing abdominal distention, and a significant reduction of her urine output.
Figure 1. Diagram demonstrating the changes noticed in patient’s creatinine plasma, urine, and peritoneal fluid levels.
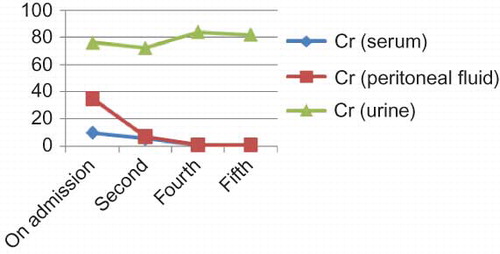
Figure 2. Algorithm for diagnosis and treatment of patients with possible urinary ascites—renal pseudofailure.
On admission, she presented with tachycardia, hyponatremia (Na = 127 mmol/L), hyperkalemia (K = 5.8 mmol/L), and acute renal failure (creatinine = 10.08 mg/dL and urea = 181 mg/dL), as well as elevated white blood cell count. Metabolic acidosis from the arterial blood gases (pH 7.290, cHCO3 = 11.5 mmol/L) was also observed. The initial clinical and laboratory findings (tachycardia, elevated white blood cells, and creatinine levels) suggested the patient suffered from severe sepsis of unknown origin. An abdominal ultrasonogram revealed large amount of free peritoneal fluid, with no sign of free peritoneal air. The urine analysis revealed pyuria and hematuria.
Following initial evaluation, a Foley catheter was placed and a puncture of the peritoneal cavity was carried out. Within 1.5 h more than 3500 cc of urine was drained from the Foley catheter and approximately 900 cc of peritoneal fluid from the peritoneal cavity. The macroscopic view of both fluids was identical (light blood-stained urine).
Biochemical analysis of both fluids revealed an increased creatinine level of the peritoneal fluid, Cr = 35 mg/dL (more than three times higher than serum creatinine levels and only half as high compared with urine creatinine levels). Protein concentration in ascitic fluid was 0.41 g/dL.
The following day, after proper renal prophylaxis taken,Citation2 the patient underwent computed tomography angiography of the abdomen and pelvis, which revealed excess ascitic fluid but no other useful findings. As a result, hyponatremic renal pseudofailure due to prolonged uroperitoneum and “reverse” auto-peritoneal dialysis, following explosive rupture of the urinary bladder during vaginal delivery, was seriously considered as the underlying cause of the patient’s condition.Citation3,4
Sequent retrograde cystography and computed tomography cystography failed to demonstrate a defect of the urinary bladder wall, while in an intravenous pyelogram both ureters were intact. Based on these findings, which suggested that the bladder’s wall defect had healed or most likely was intermittently sealed by overlying abdominal structures (such as omentum) or even a blood clot,Citation5 the choice for initial conservative treatment was made.
The patient received 3 L of intravenous fluids daily, in order to correct the apparent dehydration and the electrolyte imbalance, as well as empiric intravenous antibiotics and nitrofurantoin as urine bactericidal.
On the first day after admission, significant amount of fluids was drained from the peritoneal cavity, approximately 2 L, and the urinary bladder, more than 3.5 L. On the following day significant reduction in the drained peritoneal fluid was noticed, till the fifth day after admission in which less than 200 cc was drained and the decision to remove it was made. Also a significant reduction of creatinine levels in the peritoneal fluid was noticed, reaching reference levelsCitation6 ().
Furthermore, the electrolyte and acid–base imbalances and white blood cell count were back to normal and, by the sixth day, the patient was allowed to leave the hospital, while the Foley catheter remained for another week for precaution.
DISCUSSION
Uroperitoneum, that is, the extravasation of urine into the peritoneal cavity, has been documented as a cause of serious disproportion between the blood urea nitrogen and serum creatinine values since 1972.Citation7
The incidence of intraperitoneal bladder rupture after normal vaginal delivery is extremely rare; therefore, the diagnosis may be critically delayed. The first reported case in the literature was in 1995.Citation8 Since then, few (three to our knowledge) similar case reports have been published.Citation5,9 In our case, we were not able to confirm whether the patient’s bladder was catheterized during labor, but even if it was, that alone would not necessarily have prevented the bladder’s injury, as reported in previous cases in the literature.Citation5
Delayed diagnosis, leading to prolonged uroperitoneum for several days, may lead to “reverse” auto-peritoneal dialysis and continuous reabsorption of creatinine, urea nitrogen, and potassium in the urine via the peritoneum into the systemic circulation (down-gradient concentration). Instead, sodium and chloride ions travel from the systemic circulation to the uroperitoneum through the peritoneal membranes, causing higher concentration in the bloodstream rather than in the urine. These basic mechanisms lead to the electrolyte and acid–base imbalances, and renal pseudofailure presented in such conditions. Hyponatremia, hyperkalemia, and metabolic acidosis occur even in the first 24 h of uroperitoneum’s development.Citation3,4
Conservative management is the ideal medical treatment, if the patient’s condition and the defect of the urinary bladder allow. It mainly consists of prolonged bladder decompression by the use of a bladder catheter facilitating bladder healing. Also plenty of intravenous fluids and the correction of electrolyte and acid–base imbalances are imperative. A large intraperitoneal defect of the bladder wall may require surgical repair to be corrected.Citation10
Since normal reference values of urea nitrogen and creatinine in peritoneal fluid are equivalent to serum and significantly less than urine levels (47–157 times less),Citation9 elevated levels should immediately raise the suspicion of a possible intraperitoneal urinary leak.Citation3,4
An indispensable diagnostic step () is the puncture of the peritoneal cavity and the biochemical examination of the drained peritoneal fluid which allows the comparison with plasma biochemical markers and leads to early diagnosis and proper treatment.Citation3,4
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Rajasekar D, Hall M. Urinary tract injuries during obstetric intervention. Br J Obstet Gynaecol. 1997;104(6):731–734.
- Thomsen HS. ESUR Guidelines on Contrast Media, Version 7.0. Heidelberg: European Society of Urogenital Radiology; 2008.
- Wystrychowski A, Nowicki M, Kokot F. Hyponatraemic renal pseudo failure–Don’t forget the possibility of uroperitoneum. Nephrol Dial Transplant. 1996;11:2491–2492.
- Heyns CF, Rimington PD. Intraperitoneal rupture of the bladder causing the biochemical features of renal failure. Br J Urol. 1987;60(3):217–222.
- Png KS, Chong YL, Nq CK. Two cases of intraperitoneal bladder rupture following vaginal delivery. Singapore Med J. 2008;49(11):e327–e329.
- Manahan KJ, Fanning J. Peritoneal fluid urea nitrogen and creatinine reference values. Obstet Gynecol. 1999;93:780–782.
- Sullivan MD, Lacener LH, Banowsky LH. Intraperitoneal extravasation of urine. J Am Med Assoc. 1972;221:491–492.
- Kibel AS, Staskin DR, Grigoriev VE. Intraperitoneal bladder rupture after normal vaginal delivery. J Urol. 1995;153:725–727.
- Kekre AN, Kekre N, Nath V. Spontaneous rupture of the urinary bladder in the puerperium. Aust N Z J Obstet Gynaecol. 1997;37:473–474.
- Corriere Jr., JN, Sandler CM. Management of the ruptured bladder: Seven years of experience with 111 cases. J Trauma. 1986;26(9):830–833.
- Chan PND, Abujudeh H, Cushing Jr.,GL. CT cystography with multiplanar reformation for suspected bladder rupture: Experience in 234 cases. AJR. 2006;187:1296–1302.