Abstract
Pruritus is an alarming symptom in patients with end-stage renal disease (ESRD) accompanied by sleep disturbances and physical and mental disorders. Although its prevalence is very high among hemodialysis patients (90%), its etiology and its successful treatment have been unconfirmed (Melo N, Elias R, Castro M, Romao G, Abensur H. Pruritus in hemodialysis patients: The problem still remains. Hemodial Int. 2009;13:38–42.). Common pruritus etiologies, such as high parathyroid hormone levels, dialysis inadequacy, and iron deficiency are matters of conflict. The case of a hemodialysis patient with consistent itching and a variety of cutaneous eruptions, which after performing skin biopsy were explored and cured, is described. This article addresses the possibility of other causes of pruritus in ESRD and encourages watchful waiting with simple medical interventions, which would relieve patients’ symptoms.
INTRODUCTION
Pruritus is an alarming symptom in patients with end-stage renal disease (ESRD) accompanied by sleep disturbances and physical and mental disorders. Although its prevalence is very high among hemodialysis patients (90%), its etiology and its successful treatment have been unconfirmed.Citation1 Common pruritus etiologies, such as high parathyroid hormone levels, dialysis inadequacy, and iron deficiency are matters of conflict. The case of a hemodialysis patient with consistent itching and a variety of cutaneous eruptions, which after the performing of skin biopsy were explored and cured, is described. This article addresses the possibility of other causes of pruritus in ESRD and encourages watchful waiting with simple medical interventions, which would relieve patients’ symptoms.
CASE REPORT
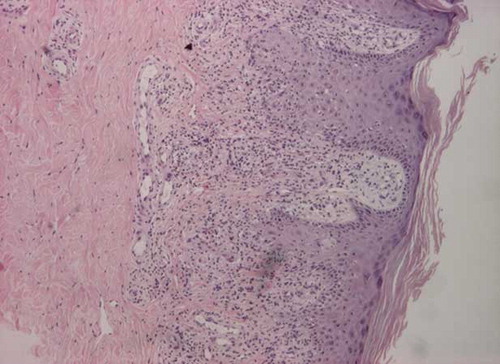
A 55-year-old female patient on maintenance hemodialysis developed pruritic plaque scales and excoriation distributed widely over her body including on the sun-exposed and on the non-sun-exposed areas. Her medical history comprised also of hypothyroidism and severe pruritus that started 1 month before the onset of dialysis. At that time, no medical condition or disease (hyperphosphatemia, hypertransaminasemia, hyperparathyroidism, hypothyroidism, or immune disorder) that could explain either the symptom or the skin eruption was detected. With the initiation of dialysis, the patient noticed increased itching, and 3 months later the symptom reappeared accompanied by slightly scaly patches and digitate dusky violaceous or brown hyperpigmented lesions on the nape, the trunk, the extensor surfaces of forearms, and the inner thighs. Simultaneously, no change was confirmed in euthyroid and parathyroid state, equilibrium, anemia, dialysis adequacy (Kt/V: 1.3), relation with standard dialysis medications, or other systemic diseases. Due to the severity of the itching and the physiological status of the patient, skin biopsy was performed. The histopathologic changes showed epidermis with focal slight degenerate and spinous cells, basal membrane with restricted degeneration and papillary dermis with perivascular infiltrates, and parakeratosis and exocytosis of small lymphocytes, without signs of lichenoid dermatitis. These lymphocytic infiltrations were attributable to nonspecific parapsoriasis (PP) or mycosis fungoides (MF). The patient was treated with local corticosteroids, moisturizers, and sedating antihistamines and was closely monitored. After 1 month of therapy, the skin lesions and pruritus subsided completely. Unfortunately, a similar cutaneous pattern, but with mottle pigmentation and strikingly sparse distribution over the same body parts, was manifested within the following 3 months. Bothersome pruritus and xerosis of the whole body were also predominant symptoms. Once again, pathological findings and irritating triggers (environmental, physiological, and mechanical factors) were absent. Therefore, a new skin biopsy was performed, surprisingly revealing lichenoid inflammatory reaction of lichen planus (). The patient was despondent and not cooperative for further local treatment, so she was commenced on prednisolone 1 mg/kg/day. Within the next few days, her skin lesion improved (so corticosteroids tapered into small doses) and completely resolved after 2 months. Now, 1 year later, the patient remains under hemodialysis without any sign of recurrence (itching or skin eruption) or any other complication.
DISCUSSION
PP describes a group of cutaneous diseases with common features of chronicity, absence of symptoms, resistance to available therapy, and histologically round cell infiltrate in papillary dermis with spongiosis and parakeratosis. When the lesions are localized on the upper trunk and they are up to 6 cm in diameter with a digitate appearance, it is considered a small plaque PP type, whereas if the lesions are larger frequently manifesting on non-sun-exposed areas with atrophy and/or poikiloderma, it is considered a large plaque PP type.Citation2 Although PP has been suggested to be an early manifestation of the cutaneous T-cell lymphoma MF, most times it runs a benign course and remains indolent for many years.Citation2 The predominant histological features of MF are lymphocytic infiltrate in the upper dermis, epidermotropism, haloed lymphocytes in epidermis, Pautrier’s microabscesses, and interface dermatitis.Citation3
ESRD presents a range of cutaneous alterations that have multiplied since the advent of hemodialysis, which prolongs life expectancy and therefore gives time for these changes to manifest.Citation4 Cutaneous involvement in renal disease is due to uremic factors, metabolic disturbances, erythropoiesis stimulating agents, dialysis dose, secondary hyperparathyroidism and deregulating inflammatory responses. Pruritus is the most prevalent complaint (50–90%) among patients undergoing hemodialysis and may result in other dermatologic conditions such as lichen simplex, prurigo nodularis, and keratotic papules. Lichenification consists of isolated circumscribed plaques varying in size from 2 to 10 cm, appearing in the extensor surface of the forearm, in the inguinal and anoperineal areas.Citation1 Our patient presented histopathologic features of PP, MF, dermatitis, and lichen planus. Although she received nonspecific and symptomatic treatment, ultimately she had an excellent response to regular corticosteroid treatment and did not present other clinical manifestations, compatible with cutaneous T lymphoma as described by Miyoshi et al.,Citation5 but only lichenification as described by Simpson and Raj.Citation6 This interesting histopathological variant of cutaneous lesions associated with itching in a patient on maintenance hemodialysis has not been reported until now. It is essential to increase the awareness about pruritus with cutaneous alterations in patients with ESRD undergoing hemodialysis for an early and effective treatment, which will ameliorate the quality of life and will combat mortality and morbidity.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Melo N, Elias R, Castro M, Romao G, Abensur H. Pruritus in hemodialysis patients: The problem still remains. Hemodial Int. 2009;13:38–42.
- Sarveswari KN, Yesudian P. The conundrum of parapsoriasis versus patch stage of mycosis fungoides. Indian J Dermatol Venereol Leprol. 2009;75:229–235.
- Shaikh ZI, Rahman SB. Clinicopathological spectrum of mycosis fungoides type cutaneous T-cell lymphoma. J Coll Physicians Surg Pak. 2006;16(3):171–174.
- Udayakumar P, Balasubramanian S, Ramalingam KS, Lakshmi C, Srinivas CR, Mathew AC. Cutaneous manifestations in patients with chronic renal failure on hemodialysis. Indian J Dermatol Venereol Leprol. 2006;72(2):119–125.
- Miyoshi M, Ubara Y, Tagami T, . Mycosis fungoides in a hemodialysis patient with intractable pruritus. Ther Apher Dial. 2006;10(3):296–300.
- Simpson J, Raj T. A case of lichen simplex in a patient with prolonged hyperphosphatemia. Nephrol Dial Transplant. 2007;22:655.