Abstract
Fibrillary glomerulonephritis (FGN) is a rare cause of progressive renal dysfunction resulting in fibrillary deposits in the mesangium and/or glomerular basement membrane (GBM). Some case reports have shown FGN in patients with rheumatoid arthritis and other autoimmune diseases. This is the first case report of FGN in a patient with Behçet’s syndrome. The most common renal histological finding in Behçet’s syndrome is secondary amyloidosis. A 46-year-old woman with a 4-year history of Behçet’s syndrome was referred to the nephrology clinic with foamy urine with non-selective proteinuria (urine protein-to-creatinine ratio was 1400 mg protein/g creatinine) and microscopic hematuria. Serum and urine protein electrophoresis showed no evidence of monoclonal gammopathy. A renal biopsy was performed. Light microscopy showed mesangial widening and nodular expansion with hyaline deposits. Immunofluorescence microscopy revealed immunoglobulin M deposits in the mesangium. Congo red staining was negative. Electron microscopy showed fibrillary deposits on the GBM. Pathological findings were consistent with FGN. She had been taking 50 mg azathioprine and 3000 mg mesalazine per day for 4 years due to Behçet’s syndrome, so we did not add any other immunosuppressive agents or corticosteroids. Treatment of this glomerulopathy is not promising. It has been noted that none of the various approaches, including corticosteroid, plasmapheresis, and cytotoxic therapy, improves prognosis.
INTRODUCTION
Fibrillary glomerulonephritis (FGN) is a rare primary glomerular disease that reveals randomly arranged, non-branching fibrillary deposits 15–30 nm in diameter, mainly in the mesangium and/or glomerular basement membranes (GBMs), with negative Congo red staining.Citation1,2 FGN is encountered in 0.5–1% of native kidney biopsies.Citation3 Most of the previously reported cases were idiopathic and occurred in the absence of other systemic diseases.Citation3–5 However, 15% of patients with FGN had a history of autoimmune diseases, including Crohn’s disease, systemic lupus erythematosus (SLE) with no histological evidence of lupus nephritis, Graves’ disease, idiopathic thrombocytopenic purpura, primary biliary cirrhosis, ankylosing spondylitis, or Sjögren’s syndrome.Citation6 This is the first case report of FGN in a patient with Behçet’s syndrome. The most common renal problems in patients with Behçet’s syndrome are asymptomatic hematuria and proteinuria followed by amyloidosis.Citation7 The association between FGN and Behçet’s syndrome is unclear.
CASE REPORT
A 46-year-old woman was referred to our nephrology clinic with foamy urine in January 2011. In 2007, she was diagnosed with Behçet’s syndrome due to the presence of cutaneous pathergy together with recurrent oral, genital, and colonic ulcers. At the time of her initial visit in 2007, her urine contained blood (++), and microscopic examination of urine revealed 3–5 red blood cells per high-power field. She had been treated with 50 mg of azathioprine and 3000 mg of mesalazine per day since then due to Behçet’s syndrome. In January 2011, she presented with foamy urine and was referred to the nephrology clinic. Her blood pressure at presentation was 120/80 mmHg. Laboratory results showed a hemoglobin concentration of 9.6 g/dL, a white blood cell count of 4170/mm3, a platelet level of 265,000 mm3, and a serum creatinine concentration of 0.53 mg/dL. Her estimated glomerular filtration rate (eGFR) was 114.7 mL/min/1.73 m2. The eGFR was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation. Serum albumin level was 3.3 g/dL, and total cholesterol was 182 mg/dL. Her urine contained blood (++) and protein (+), but the urinary protein-to-creatinine ratio was 1.4. The total 24-h urinary protein excretion was 1868 mg, but her proteinuria could not be detected by conventional dipstick analysis. Therefore, we suggested that she had non-albumin proteinuria (e.g., tubular or light chain proteinuria). Thus, an immunoelectrophoresis test was conducted. Urine protein electrophoresis showed no evidence of monoclonal gammopathy, but serum protein electrophoresis showed polyclonal gammopathy. Tests for ANA, ANCA, dsDNA antibodies, rheumatoid factor, and cryoglobulins were negative. Serology for hepatitis B and C was negative. An ultrasound scan demonstrated normal kidneys.
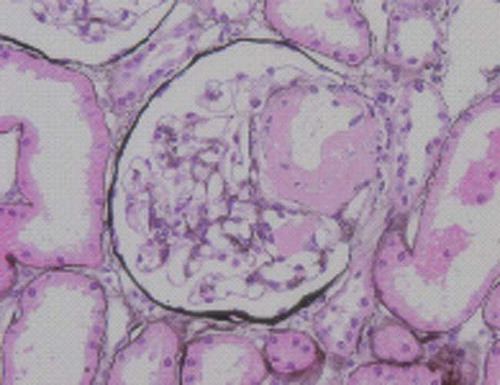
A renal biopsy was performed. Light microscopy showed mesangial widening and nodular expansion with hyaline deposits. Eosinophilic hyaline deposits were seen in the mesangium and the afferent arteriolar wall (). Congo red staining was negative. Immunofluorescence microscopy revealed immunoglobulin M deposits in the mesangium. Electron microscopy showed fibrillary deposits in the mesangium () and in a sub-epithelial zone on the capillary wall (). Pathological findings were consistent with FGN. We did not add any other immunosuppressive agents or corticosteroids.
Figure 1. Eosinophilic hyaline deposits were seen in the mesangium and afferent arteriolar wall. Jones methenamine silver stain, original magnification ×400.
DISCUSSION
FGN was first described by Rosenmann and Eliakim in 1977 as an amyloid-like glomerulopathy, but with negative Congo red staining.Citation1 FGN is characterized by the deposition of randomly arranged fibrils in the mesangium and on the GBM. The fibrils are generally <30 nm in diameter, with the majority measuring approximately 20 nm.Citation1,2 Light microscopy typically demonstrates mesangioproliferative or membranoproliferative glomerulonephritis. On immunofluorescence, the deposits typically stain for polyclonal IgG, and complement IgA, IgM, or C1q deposition is less commonly found.Citation8,9
FGN is most common in adults 46–65 years of age.Citation6 Most patients present with nephrotic-range proteinuria with or without renal insufficiency and hematuria.Citation6 Previous studies have indicated that most cases of FGN are idiopathic.Citation2–4 However, a recent report by Samih et al. indicated that one-third of cases occur in patients with a history of malignancy or autoimmune diseases.Citation6 There have also been rare case reports of FGN associated with systemic lupus erythematosus (SLE), rheumatoid arthritis, primary biliary cirrhosis, hemolytic anemia, HIV infection, essential thrombocytosis, Castleman’s disease, gastric adenocarcinoma, and metastatic hepatocellular carcinoma.Citation4,Citation10–17 To our knowledge, this is the first report of FGN in a patient with Behçet’s syndrome.
The pathogenesis of FGN is thought to result from glomerular localization of immune complexes that have the ability to undergo fibrillogenesis. The source of immune stimulation remains obscure.Citation17 There is, as yet, no definitive treatment for FGN, and the response to treatment is generally poor, with more than half of the patients developing end-stage renal disease within 4 years. Features associated with poor renal outcome include older age, higher creatinine level at biopsy, higher 24-h urinary protein level at biopsy, and higher percentage of globally sclerotic glomeruli.Citation3,6 In our patient, we did not add any other immunosuppressive agents or corticosteroids because her renal function was normal at diagnosis, and she had been taking 50 mg of azathioprine and 3000 mg of mesalazine per day for 4 years due to Behçet’s syndrome. However, an inhibitor of angiotensin-converting enzyme was used to treat her proteinuria.
Considering her proteinuria of >1 g/day, this patient was initially suspected to have renal amyloidosis, given that the most common renal problems in Behçet’s syndrome are asymptomatic hematuria and proteinuria, followed by amyloidosis.Citation7 Unexpectedly, her pathological diagnosis was FGN. Although rare, FGN should be considered as a possible cause of heavy proteinuria in patients with Behçet’s syndrome.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Rosenmann E, Eliakim M. Nephrotic syndrome associated with amyloid-like glomerular deposits. Nephron. 1977;18:301–308.
- Rosenstock JL, Markowitz GS, Valeri AM, Sacchi G, Appel GB, D’Agati VD. Fibrillary and immunotactoid glomerulonephritis: Distinct entities with different clinical and pathologic features. Kidney Int. 2003;63:1450–1461.
- Iskandar SS, Falk RJ, Jennette JC. Clinical and pathologic features of fibrillary glomerulonephritis. Kidney Int. 1992;42: 1401–1407.
- Haas M, Rajaraman S, Ahuja T, Kittaka M, Cavallo T. Fibrillary/immunotactoid glomerulonephritis in HIV-positive patients: A report of three cases. Nephrol Dial Transplant. 2000;15:1679–1683.
- Pronovost PH, Brady HR, Gunning ME, Espinoza O, Rennke HG. Clinical features, predictors of disease progression and results of renal transplantation in fibrillary/immunotactoid glomerulopathy. Nephrol Dial Transplant. 1996;11:837–842.
- Nasr SH, Valeri AM, Cornell LD, . Fibrillary glomerulonephritis: A report of 66 cases from a single institution. Clin J Am Soc Nephrol. 2011;6:775–784.
- Akpolat T, Akkoyunlu M, Akpolat I, Dilek M, Odabas AR, Ozen S. Renal Behçet’s disease: A cumulative analysis. Semin Arthritis Rheum. 2002;31:317–337.
- Fogo A, Qureshi N, Horn RG. Morphologic and clinical features of fibrillary glomerulonephritis versus immunotactoid glomerulopathy. Am J Kidney Dis. 1993;22:367–377.
- Ivanyi B, Degrell P. Fibrillary glomerulonephritis and immunotactoid glomerulopathy. Nephrol Dial Transplant. 2004;19: 2166–2170.
- Menon S, Zeng X, Valentini R. Fibrillary glomerulonephritis and renal failure in a child with systemic lupus erythematosus. Pediatr Nephrol. 2009;24:1577–1581.
- Yun YS, Song HC, Lee K, . Fibrillary glomerulonephritis in rheumatoid arthritis. Nephrology (Carlton). 2010;15: 266–267.
- Kornblihtt LI, Vassalllu PS, Heller PG, Lago NR, Alvarez CL, Molinas FC. Primary myelofibrosis in a patient who developed primary biliary cirrhosis, autoimmune hemolytic anemia and fibrillary glomerulonephritis. Ann Hematol. 2008;87: 1019–1020.
- Asaba K, Tojo A, Onozato ML, . Fibrillary glomerulonephritis associated with essential thrombocytosis. Clin Exp Nephrol. 2003;7:296–300.
- Miadonna A, Salmaso C, Palazzi P, Elli A, Braidotti P, Lambertenghi Deliliers G. Fibrillary glomerulonephritis in Castleman’s disease. Leuk Lymphoma. 1998;28:429–435.
- Abraham G, Bargman JM, Blake PG, Katz A, Oreopoulos DG. Fibrillary glomerulonephritis in a patient with metastatic carcinoma of the liver. Am J Nephrol. 1990;10: 251–253.
- Amir-Ansari B, O’Donnell P, Nelson SR, Cairns HS. Fibrillary glomerulonephritis in a patient with adenocarcinoma of stomach. Nephrol Dial Transplant. 1997;12:210–211.
- Guerra G, Narayan G, Rennke HG, Jaber BL. Crescentic fibrillary glomerulonephritis associated with hepatitis C viral infection. Clin Nephrol. 2003;60:364–368.