Abstract
Sarcoidosis is a systemic disorder with a wide spectrum of clinical involvements. Renal mass is a very rare condition in sarcoidosis. Here, we report a 34-year-old female with renal masses and advanced renal failure. The condition created a lot of diagnosis difficulties. Finally, after histologic diagnosis and corticosteroid therapy, renal masses were resolved and she became free from dialysis.
INTRODUCTION
Renal involvement is a known occurrence in sarcoidosis and happening in as many as 25% of patients, but renal failure is not a common finding, and is reported in 0.7–4.3% of patients.Citation1 The renal disease is commonly related to hypercalcemia with resultant nephrolithiasis and nephrocalcinosis.Citation2
Other manifestations include granulomatous interstitial nephritis (GIN), glomerulonephritis, renal tubular defects, mechanical urinary tract disease, and endovascular diseases.
Nephrocalcinosis is the most common cause of progressive renal failure.Citation2
Granulomatous inflammation, although found in a substantial number of kidneys at autopsy (more than 20%), only represents a very small proportion of clinically relevant renal failure in sarcoidosis.Citation3,4 Renal mass is a very rare manifestation of sarcoidosis and has been reported only in two patients. Herein, we report another patient who presented with renal dysfunction and renal mass and was finally diagnosed as having renal involvement in sarcoidosis.Citation5,6
CASE
A 34-year-female was referred to our nephrology clinic for future evaluation of renal dysfunction. Her blood pressure was 135/75 mmHg; pulse rate was 85/min; and body temperature was 37.0°C. Anemia was apparent on examination. Lung sounds and heart sounds were normal, as were the head and neck, abdomen, and extremities. Neurological examination revealed no abnormality, and superficial lymph nodes were not palpable. She had a history of renal stone passage last year. Laboratory data on admission are shown in .
Table 1. Laboratory findings on admission.
Renal ultrasound study showed a right kidney size of 106 × 31 mm and a left kidney size of 110 × 40 mm with elevated cortical echogenicity on both sides. A round isoechoic mass lesion of 22–25 mm was detected in the lower pole of the left kidney. Ultrasound study revealed normal liver and spleen without lymphadenopathy. Abdominal and pelvic computed tomo‐graphy (CT) demonstrated mass-like densities in middle and lower zones of the left kidney. The results were negative for lymphadenopathy.
Figure 1. Magnetic resonance imaging (MRI, T2) of abdomen and pelvis in a coronal section confirmed the presence of renal mass at the middle zone of the left kidney.

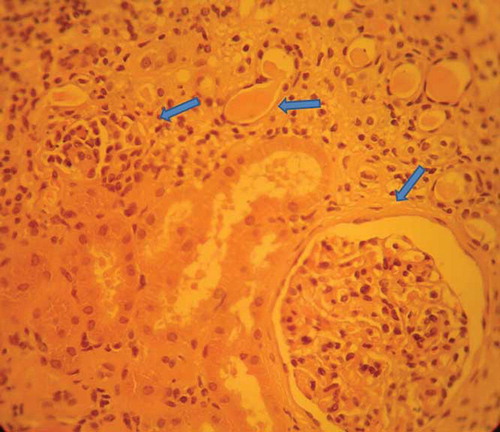
Magnetic resonance imaging (MRI) of abdomen and pelvis in coronal and sagittal views confirmed the presence of two mass lesions, 15 and 18 mm, at middle and lower pole zones of the left kidney (). MRI findings were suggestive of tumor infiltration. Chest radiography and chest CT scan showed mediastinal and hilar lymphadenopathy, with a maximum diameter of 20 mm in the left hilum. Lung parenchyma was normal. Bronchoalveolar lavage was negative for tuberculosis, tumor, or fungi. Electrocardiography showed no arrhythmias or blocks. Echocardiography revealed normal pericardium, septum, chamber size, and normal myocardial contraction. Purified protein derivative (PPD; <5 mm induration) skin test was negative. Serum angiotensin-converting enzyme (ACE) level was 42 IU/L (8–65). The results of urine smear and culture were negative for Mycobacterium tuberculosis. Bone marrow aspiration and trephine needle biopsy disclosed normal marrow without any malignancy or granuloma. Because of her advanced renal insufficiency, hemodialysis was started. She underwent a left hemithorax thoracoscopy to obtain a left hilar lymph node biopsy. The frozen section was negative for malignancy and was positive for granulomatosis inflammation. Histopathological examination revealed non-caseating granulomas composed of aggregates of epithelioid cells and Schaumann bodies without caseating necrosis. Acid-fast bacilli were not detected (). The finding was compatible with sarcoidosis and no evidence of lymphoma was present. She had no occupational or environmental exposure that is known to induce granulomatous disease. A percutaneous needle biopsy of the left kidney showed marked mononuclear interstitial infiltration with occasional aggregate formation and tubular atrophy with mild mesangial widening and periglomerular fibrosis ().
Figure 2. Histopathological examination of left hilar lymph node biopsy revealed non-caseating granulomas composed of aggregates of epithelioid cells and Schaumann bodies without caseating necrosis. Acid-fast bacilli were not detected.

Figure 3. A percutaneous needle biopsy of the left kidney showed mononuclear interstitial infiltration with occasional aggregate formation and tubular atrophy with mild mesangial widening and periglomerular fibrosis.
Treatment with prednisolone (1 mg/kg) was started. The patient’s general condition improved, the urine output gradually increased, and she became free from dialysis. Mediastinal lymph nodes and renal masses disappeared and serum creatinine decreased to 2.5 mg/dL within 2 months. After 1 year of follow-up her serum creatinine level remained below 3.0 mg/dL and she was in a good general condition.
DISCUSSION
The combination of renal mass and hilar lymphadenopathy in the presentation of sarcoidosis creates a great confusion. Meanwhile, this case clearly demonstrated the excellent response of sarcoidosis interstitial nephritis to corticosteroid therapy even in its advanced stages. Renal mass is a very rare finding and causes confusion over correct diagnosis of sarcoidosis. Mass lesions are a common feature of renal lymphoma and renal cell carcinoma and both of them could also manifest with hilar lymphadenopathy.Citation3 Coalescing granuloma and interstitial mononuclear cell infiltration could be responsible for mass-like aggregate in sarcoidosis.Citation5,6
GIN is a typical feature of sarcoidosis interstitial nephritis. However, in a retrospective study, 10 out of 47 patients had interstitial nephritis without granulomas.Citation1 In another report up to 25% of patients with sarcoidosis interstitial nephritis were found without granuloma.Citation7 Lack of granuloma formation could happen in advanced disease stage or just because of the sampling effect. On the other hand, granuloma is a feature of renal tuberculosis, microscopic angitis (previously Wegener), and interstitial nephritis associated with non-steroidal anti-inflammatory medicines.Citation8 Glomerular involvement is an uncommon feature of sarcoidosis and in this case we did not find any glomerular involvement.Citation2,3 The serum level of ACE inhibitor was not elevated in our report. ACE elevation is not reported so frequently and lacks specificity for both the diagnosis and the disease activity.Citation9 Hypercalcemia has been reported in up to 20% of sarcoidosis patients.Citation3,10 Our patient was not hypercalcemic, but she had a history of renal stone passage last year. Different manifestations of sarcoidosis are more common in different populations, such as chronic uveitis in US blacks, lupus pernio in Puerto Ricans, and erythema nodosum in Europeans. Cardiac and ocular sarcoidosis appears to be more common in Japan. We did not find any of the above findings in our patient. In developing regions, more commonly known granulomatous diseases such as tuberculosis, leprosy, and fungal infection can obscure the diagnosis of sarcoidosis.Citation10 Corticosteroid treatment is the cornerstone of treatment, and as we observed in our patients the efficacy of corticosteroids has been demonstrated even in advanced sarcoid tubulointerstitial nephritis.Citation7,10
Sarcoidosis continues to be a disease that confounds and surprises the clinicians. The rare presentation of sarcoidosis such as renal mass could create confusion for unaware clinicians.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Mahevas M, Lescure FX, Boffa JJ, . Renal sarcoidosis, clinical, laboratory, and histologic presentation and outcome in 47 patients. Medicine. 2009;88:98–106.
- Kettritz R. The protean face of sarcoidosis revisited. Nephrol Dial Transplant. 2006;21:2690–2694.
- Gobel U, Kettritz R, Schneider W, Luft FC. The protean face of sarcoidosis. J Am Soc Nephrol. 2001;12:616–623.
- Jose MD, McGregor DO, Lynn KL. Renal sarcoidosis in Christchurch, New Zealand 1970–1998. Aust NZ J Med. 1999;29:770–775.
- Koyama T, Ueda H, Togashi K, Umeoka S, Kataoka M, Nagai S. Radiologic manifestation of sarcoidosis in various organs. Radiographics. 2004;24:87–104.
- Mizunoe S, Yamasaki T, Tokimatsu I, . Sarcoidosis associated with renal masses on computed tomography. Intern Med. 2006;45(5):279–282.
- Rajakariar R, Sharples EJ, Raftery MJ, Sheaff M, Yaqoob MM. Sarcoid tubulo-interstitial nephritis: Long-term outcome and response to corticosteroid therapy. Kidney Int. 2006;70:165–169.
- Miller BW, Miller SB, McKenzie CR, Davila RM. Granulomatous interstitial nephritis: Drug hypertensivity, infection, or sarcoidosis? Am J Kidney Dis. 1997;30:586–588.
- Beneteau-Burnat B, Baudin B. Angiotensin-converting enzyme: Clinical applications and laboratory investigations on serum and other biological fluids. Crit Rev Clin Lab Sci. 1991;28:337–356.
- Statement on sarcoidosis: Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999;160:736–755.