Abstract
Aim: The aim of this study is to assess the prevalence and knowledge of chronic kidney disease (CKD) in those presenting to a District General Hospital (DGH) in the United Kingdom with troponin positive acute coronary syndrome (ACS) as compared to a sample of the general population. Methods: A retrospective observational study. Data were collected from ProForma completed during the 18-month period from 1 November 2007 to 30 April 2009. The stage of CKD and the proportion of undocumented CKD at presentation were calculated and the mean stage was compared with the general practice population (of similar demographics) sampled by de Lusignan et al. (Identifying patients with chronic kidney disease from general practice computer records. Fam Pract. 2005;22:234–241.) using the t-test statistics. Results: A total of 936 patients (600 men and 336 women) presented with troponin positive ACS; their mean stage of CKD = 2.874 ± 0.024. This was significantly different from the mean stage of CKD = 1.999 ± 0.004 found within the general population (p < 0.001). About 58.6% of patients with CKD stages 4 or 5 had no knowledge or documentation of their renal impairment. Conclusions: Among those presenting to hospital with troponin positive ACS were many patients with undocumented severe renal impairment, emphasizing the need for general practitioners to screen for renal disease and refer to specialist nephrology services where appropriate. Joint renal and cardiac clinics may offer better care for this group of patients’ long-term care.
INTRODUCTION
It is well known that chronic kidney disease (CKD) is a risk factor for cardiovascular disease, being documented in papers as early as the 1970s.Citation1 The risk is proportional to the level of renal dysfunction but even minor impairment will increase the likelihood of developing cardiovascular disease.Citation2 Once cardiovascular disease is present or a cardiac event has occurred, CKD becomes an independent predictor of morbidity and mortality.Citation3–5 Matts et al.Citation3 report that following an acute myocardial infarction each increase in creatinine levels of 9 μmol/L above baseline corresponds to a relative risk increase of 36% for overall mortality and 47% for subsequent atherosclerotic coronary heart disease. Even though CKD has a significant impact on patient health, long-term morbidity, and mortality, it is often underdiagnosed.Citation6
The aim of this retrospective observational study was to assess the prevalence of CKD among patients presenting to a large District General Hospital (DGH) with troponin positive acute coronary syndrome (ACS) as compared with a sample of the general population and determine the proportion of undocumented CKD in this patient group.
METHODS
Data were collected from ProForma completed during the 18-month period from 1 November 2007 to 30 April 2009 for patients admitted to a large DGH for Troponin positive ACS. Each ProForma was completed by one of the two specialist cardiac nurse practitioners at the time of admission as part of the National Health Service national myocardial infarction audit. Demographic data, initial creatinine (done at the time of admission to hospital), and whether the patient was documented to have renal impairment prior to admission were recorded.
Glomerular filtration rate (GFR) was estimated using the modification of diet in renal disease equation.Citation7 Stage of CKD was recorded as one of the five stages defined by the National Kidney Foundation Kidney Disease Outcomes Quality Initiative ().Citation8
Table 1. Stages of CKD (from KDOQI CKD guidelines).
Table 2. Age–sex distribution of the prevalence of CKD stage.
Comparison was made with data from the de Lusignan et al.’sCitation9 study as the general practice populations sampled by de Lusignan et al.Citation9 are of a similar ethnic and social composition to the population from which the patients of this study belong. In both this study and that done by de Lusignan et al.Citation9 the presence or absence of microalbuminuria was not known, so it was not possible to determine CKD stages 1 and 2, instead GFR ≥ 90 mL/min/1.73 m2 was regarded as normal and a GFR = 60–89 mL/min/1.73 m2 as mildly impaired.
The t-test statistic was used to compare means. The proportion of undocumented CKD at initial presentation was also calculated.
RESULTS
A total of 936 patients (600 men and 336 women) presented with troponin positive ACS between 1 November 2007 and 30 April 2009 ().
For these patients the mean GFR = 49.74 ± 0.57 and the mean stage of CKD = 2.874 ± 0.024; this was significantly different from the mean stage of CKD = 1.999 ± 0.004 found in the general practice population (of similar demographics) sampled by de Lusignan et al.Citation9 (p < 0.001) ().
Figure 1. Graph showing distribution of stage of CKD comparing general population with those presenting with troponin positive ACS.
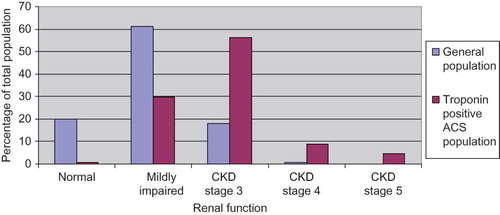
Figure 2. Graph showing percentage of patients within each CKD group who had no documented knowledge of renal impairment.
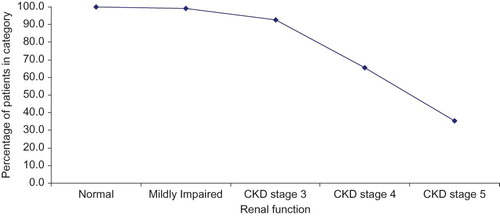
About 35.5% of patients with CKD stage 5, 65.7% of patients with CKD stage 4, and 92.7% of patients with CKD stage 3 had no knowledge or documentation of their renal impairment ().
DISCUSSION
A total of 936 patients presented to hospital with troponin positive ACS during the study period from 1 November 2007 to 30 April 2009. For each patient the GFR was estimated and staging of renal function was done. For all patients the average stage was 2.874, significantly higher than the general population (average stage of CKD = 1.999 ± 0.004). A total of 85.7% of patients with GFR < 60 mL/min/1.73 m2 and thus suffering from CKD as defined by the National Kidney Disease Education ProgramCitation10 had no documented knowledge of their renal impairment and were not known to the local nephrology service.
The Department of Health has given clear guidance to primary care physicians [general practitioners (GPs)] about identifying CKD patients and the management of them in the community. As part of this there is an emphasis on the need for referral to a nephrologist for further input in the care of patients with worsening CKD stage 3 and any patient with CKD stages 4 or 5. It was quite alarming to see a significant proportion of patients within this study with CKD stages 4 and 5 not being identified or referred to the local nephrology service. This is in keeping with data from the UK Renal Registry which reports that a significant proportion (25%) of the patients starting on dialysis in the United Kingdom are “crash landers” (defined as patients not known to a renal service 3 or more months prior to starting dialysis). Our study demonstrates that further education is needed to encourage the identification of patients with CKD and their referral to local nephrology services accordingly. Our results further highlight that patients with cardiovascular disease are a high-risk population for CKD and thus a group to be specifically identified for CKD screening within primary care.
The finding of this study that there is a higher prevalence of CKD among UK patients who have suffered a cardiac event corroborates a similar finding among high-risk cardiovascular patients in Spain.Citation11 Although it has been suggested that CKD may merely reflect an increase in severity of cardiovascular disease,Citation12 it has been demonstrated to be an independent predictor of adverse outcomes in many recent reports in population-based samples, such as the Framingham studyCitation13 and the National Health and Nutrition Epidemiological Survey,Citation14 and also in populations with pre-identified increased cardiovascular risk, such as within the Hypertension Optimal Treatment study.Citation15 Whether this increased risk is directly attributable to CKD or CKD is merely a surrogate of increased severity of cardiovascular disease, the perceived increase in cardiovascular risk mandates a concerted effort to screen cardiovascular patients in order to identify and then aggressively manage those with renal disease to improve outcomes.
Unfortunately, the opposite appears to be the case with 85.7% of patients with CKD 3–5 (35.5% of CKD 5) in this study having no documentation of renal impairment. Although no documentation in admission notes may not mean that renal impairment is unknown to the patient’s GP, there is the high possibility that it does. Given the potential long-term benefit of optimizing the management of renal disease in reducing further cardiovascular events, involvement of nephrologists at this stage would seem ideal (as recommended by the UK Department of Health). Given the seemingly high proportion of patients presenting to hospital with a cardiac event also being newly diagnosed with renal impairment, a joint renal-cardiac follow-up might be appropriate to optimize patient care.
Even short-term benefits could be gained from early nephrologist input. Han et al.Citation4 reported that those with moderate to severe renal impairment were less likely to receive appropriate medical treatment following non-ST elevation ACS. The reason for this was primarily due to safety concerns regarding the potential for adverse medication events when giving medications, such as anticoagulants, β-blockers, and angiotensin-converting enzyme inhibitors, to patients with renal impairment. Specialist knowledge regarding the use of medications in the presence of renal impairment would allow for the best possible optimization for each of these patients during their hospital stay immediately following a cardiac event.
The main limitation of this study is that GFR is estimated for each patient at one point in time; it is therefore not possible to distinguish acute deterioration in renal function from a more chronic disease process. However, the overestimation this could be expected to produce should be in a similar proportion to that in the article by Lusignan et al.,Citation9 thus allowing the two data sets to be legitimately compared.
Given the high prevalence of undiagnosed CKD within the population,Citation6 the importance of medication dose adjustment in those with renal impairment, and the potential benefit to the individual of aggressive management of those with true renal impairment, the renal function of this population group should be monitored closely in both short and longer terms. Although nephrologist involvement would be ideal, given the large numbers of patients that would require a review and that a proportion of those will have only a transient period of renal dysfunction, it is possibly more realistic to ask GPs to follow each of these patients up with repeat tests of renal function and then refer to a nephrologist as appropriate.
GFR was estimated using a formula for which the creatinine values had not been standardized between the various labs involved. This will have led to there being a small amount of error in comparing the two populations; however, this was deemed acceptable. Although the population studied by de Lusignan et al.Citation9 is likely to be very similar to that of this study based on known population demographics of the United Kingdom, they are not the same.
In conclusion, this study has shown that the prevalence of CKD is higher among patients presenting with troponin positive ACS than that of the general population. The large proportion of these patients having unknown renal impairment suggests the need for ongoing encouragement of those in primary care to screen for and refer as appropriate those with renal disease, so that this group might benefit from nephrology input to optimize management and thus help reduce future morbidity and mortality.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Lindner A, Charra B, Sherrard DJ, Scribner BH. Accelerated atherosclerosis in prolonged maintenance hemodialysis. N Engl J Med. 1974;290:697–701.
- Ritz E, McClellan WM. Overview: Increased cardiovascular risk in patients with minor renal dysfunction: An emerging issue with far-reaching consequences. J Am Soc Nephrol. 2004;15:513–516.
- Matts JP, Karnegis JN, Campos CT, Fitch LL, Johnson JW, Buchwald H. Serum creatinine as an independent predictor of coronary heart disease mortality in normotensive survivors of myocardial infarction. POSCH Group. J Fam Pract. 1993;36:497–503.
- Han JH, Chandra A, Mulgund J, . Chronic kidney disease in patients with non-ST-segment elevation acute coronary syndromes. Am J Med. 2006;119(3):248–254.
- Galil AGS, Pinheiro HS, Chaoubah A, Costa DMN, Bastos MG. Chronic kidney disease increases cardiovascular unfavourable outcomes in outpatients with heart failure. BMC Nephrology. 2009;10:31.
- Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12.
- Levey AS, Bosch JP, Lewis JB, . A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med. 1999;130:461–470.
- National Kidney Foundation (NKF) Kidney Disease Outcome Quality Initiative (KDOQI) Advisory Board. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Kidney disease outcome quality initiative. Am J Kidney Dis. 2002;39(Suppl. 2):S1–S246. Available at: http://www.kidney.org/professionals/kdoqi/guidelines_ckd/toc.htm. Accessed August 8, 2010.
- de Lusignan S, Chan T, Stevens P, . Identifying patients with chronic kidney disease from general practice computer records. Fam Pract. 2005;22:234–241.
- US Department of Health & Human Services. National Kidney Disease Education Programme (NKDEP). Definition of Chronic Kidney Disease (CKD). Available at: http://www.nkdep.nih.gov/healthprofessionals/ckdoverview.htm#definition. Accessed August 8, 2010.
- Amenós AC, González-Juanatey JR, Gutiérrez PC, Gilarranz AM, Costa CG. Prevalence of chronic kidney disease in patients with or at a high risk of cardiovascular disease. Rev Esp Cardiol. 2010;63(2):225–228.
- Garg AX, Clark WF, Haynes RB, House AA. Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int. 2002;61:1486–1494.
- Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999;56:2214–2219.
- Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13:745–753.
- Ruilope LM, Salvetti A, Jamerson K, . Renal function and intensive lowering of blood pressure in hypertensive participants of the hypertension optimal treatment (HOT) study. J Am Soc Nephrol. 2001;12:218–225.