Abstract
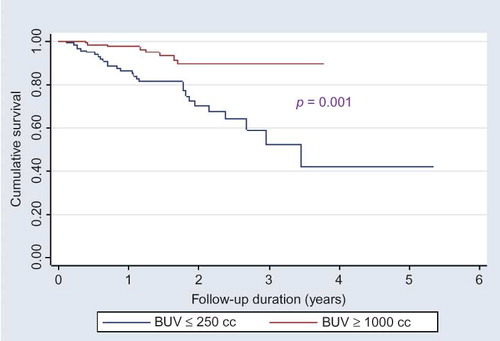
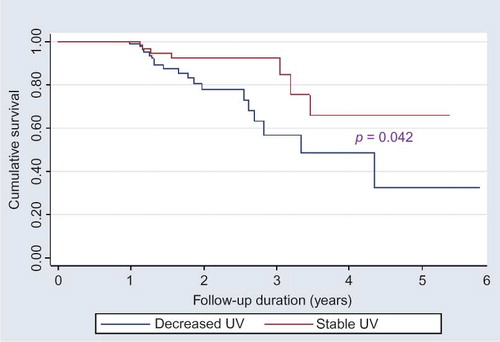
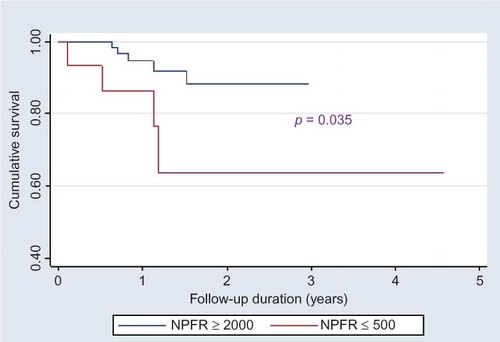
Background: Associations between patient survival and baseline urine volume (UV), ultrafiltration (UF) volume, and combined UV and UF were evaluated in Iranian continuous ambulatory peritoneal dialysis (CAPD) patients. Methods: From 1995 to 2006, data on 1472 CAPD patients from 26 centers were collected. Demographic, clinical, and laboratory characteristics were analyzed using STATA software. Baseline UV was considered as an indicator of residual renal function and patients with an annual decrease of more than 250 cc/day were placed in decreasing UV group. The role of a new variable, net positive fluid removal, which defines as the combination of baseline UV and UF, was also evaluated. Results: Patients with higher baseline UV were significantly more married and educated and candidate for CAPD based on positive selection criteria. In dichotomous categorization, mean of serum creatinine was lower and albumin was higher in patients with UV ≥ 1000 cc/day compared with UV < 250 cc/day. A significant correlation was found between baseline UV <250 cc/day and ≥1000 cc/day and patient survival. Patients with stable UV had better survival compared with patients with decreasing UV (p = 0.04). There was no correlation between UF and patient survival. Remarkable association with patient and technique survival and net positive fluid removal ≥2000 cc/day and <500 cc/day was observed. Multiple Cox regression analysis revealed significant correlation between net positive fluid removal ≥2000 cc/day and higher patient survival [p = 0.01, hazard ratio (HR) = 13.2], higher first albumin (albumin ≥ 3.5 mg/dL, p = 0.01, HR = 0.02), and lower negative selection (p = 0.0001, HR = 11.8). Conclusion: Loss of UV over time and lower net positive fluid removal increase mortality of PD patients.
INTRODUCTION
Preservation of residual renal function (RRF) is important not only for pre-end-stage renal disease (ESRD) patients but also for patients on dialysis.Citation1 RRF is now generally recognized as an important factor determining outcome of peritoneal dialysis (PD) patients.Citation1,2 The rate of RRF decline can predict morbidity and mortality of the patients on PD.Citation3,4 RRF is clinically important as it affects the dialysis adequacy, improved quality of life, and patient survival.Citation2,4
RRF is associated not only with better small solute clearance and volume control but also contributes to the removal of middle molecules and reflects the maintenance of native kidney endocrine and metabolic functions such as erythropoietin and, 1–25 (OH)2 cholecalciferol production, and phosphorus balance.Citation1,4 Moreover, cardiac hypertrophy inversely correlates with RRF. Anuric PD patients usually present with more severe form of left ventricular hypertrophy, a very well-known predictor of mortality in PD patients.Citation4
In PD patients, RRF changes over time; however, majority of studies indicate a survival benefit in those with preserved RRF. Canada–USA (CANUSA) Peritoneal Dialysis Multicenter Study confirmed that preservation of RRF over time in PD patients is a better predictor of patient survival than RRF at the initiation of PD.Citation5 Adequacy of PD in Mexico (ADEMEX) study detected that RRF was the only predictor of patient outcome.Citation6 The Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD) has shown that RRF is better preserved in PD compared with hemodialysis and the effect of RRF was more powerful than Kt/V itself in prediction of patient outcome.Citation7,8
Decline in RRF over time is a conceptual fact in chronic PD patients;Citation1,2,9,10 however, the magnitude and slope of these changes are not the same in all patients. As a result, identifying the factors that play a role in diminution and loss of RRF is an important issue.Citation9–11
Several factors can affect RRF changes in prolonged PD. Presence of diabetes mellitus (DM), higher rate of peritonitis, higher level of blood pressure, and concomitant consumption of several medications are considered as predictors of RRF loss over time.Citation12–14 Higher serum calcium, use of an angiotensin-converting enzyme inhibitor (ACEi), and calcium channel blocker have been shown to independently be associated with the preservation of RRF.Citation15
This study was designed to evaluate the correlation between patient survival and baseline UV, changes in UV over time, ultrafiltration (UF), and combined UV and UF in Iranian CAPD patients based on data retrieved from National PD Registry.
MATERIALS AND METHODS
Study Population
In 2005, a registry system was developed to establish a comprehensive data base and to facilitate and improve the patient’s management.Citation16 In this regard, a questionnaire was designed that included the questions about baseline data of the patients, follow-up visits, medications, laboratory data, PD-related and PD-non-related complications and the causes of patient’s drop out. The questionnaires were distributed to all CAPD centers and the completed forms were sent back to Shafa CAPD Registry center in a monthly basis. The data were entered in a central electronic database using “Hakim” Electronic Health Record developed by Pegahsoft Co. In 2009, the data were extracted from 26 CAPD centers participated in Iran PD Registry. The patients with complete data regarding baseline UV and UF at the initiation of PD were included in this study.
The patients were excluded at the time of data collection if they did not have records of baseline UV, were anuric, or were on PD for less than 3 months.
The follow-up records were evaluated for changes in UV over time. All patients were followed until they were either transferred to hemodialysis, had renal transplantation, or died.
Definition
UV at time of start of PD was considered as an indicator of RRF. UV records were reported as a dichotomous variable, and based on first UV, we categorized the patients into two groups: patients who had UV <250 cc/day and patients with UV ≥ 1000 cc/day. Multiple UV records during the follow up were checked and categorized into stable (with mean annual decline <250 cc/day) and declining UV (with mean annual decline more than 250 cc/day).
Mean of UF within 3 months after starting CAPD was defined as baseline UF. Net positive fluid removal was considered as the sum of baseline UV and UF values.
Negative selection was defined as patients who were selected for PD because of vascular access problems and/or cardiovascular diseases.
Comorbidity diseases consisted of diabetes, hypertension, coronary artery disease, chronic liver disease, cerebrovascular disease, respiratory disease, and malignancy.
Laboratory Evaluation
The demographic data including age, gender, cause of ESRD, presence of diabetes, comorbidity, marital status, education, selection type of patients and baseline laboratory data of serum creatinine, hemoglobin, calcium, phosphorus, iPTH, albumin, cholesterol, and triglyceride were collected. Adequacy of dialysis was measured using PD Adequest software (Baxter, version 2.0, Chicago, IL, USA). The dialysis dose (kt/V) and creatinine clearance were calculated. Additional collected data included: blood pressure measurements, episodes of peritonitis, and causes of drop out and death.
Statistical Analyses
In this historical cohort study, data were analyzed using STATA (9.0) software (StataCorp LP, TX, USA). Parametric values were expressed as mean ± SD. The chi-square test and the Fisher’s exact test were used for comparison of proportions. The Kaplan–Meier method was used to assess patient and technique survival. A p value of <0.05 was considered statistically significant.
RESULTS
The data of 1472 patients through Iran PD Registry were reviewed; but only in 477 (32%) patients, the baseline UV was recorded. The mean duration of follow-up was 4.3 years. The mean age of participants was 47.5 ± 17.4 years and 43% were male. The major causes of ESRD were diabetes (53%), hypertension (22%), and chronic glomerulonephritis (11%).
Evaluation of multiple baseline UV cutoffs showed that a significant correlation was existed between patient survival and baseline UV < 250 cc/day and ≥1000 cc/day. Based on this observation, we divided our patients into two categories: patients with baseline UV < 250 cc/day and PD patients with basal UV ≥ 1000 cc/day. presents the characteristics of these two subgroups of patients. Patients with UV ≥ 1000 cc/day were significantly more educated and married compared with patients with UV < 250 cc/day. More than 80% of PD patients with UV ≥ 1000 cc/day were candidate for CAPD based on positive selection criteria. Regarding the laboratory findings, mean of first serum creatinine was lower and mean of first serum albumin was higher in patients with UV ≥ 1000 cc/day compared with patients with UV < 250 cc/day.
Table 1. Demographic and clinical characteristics according to baseline UV.
When we divided the patients according to the records of UV over time, patients with stable UV had better survival compared with decreasing UV patients (p = 0.04). The peritonitis rate was not different between these two groups. Chronic glomerulonephritis as a cause of ESRD was more frequent in patients with declining UV (p = 0.007) and these patients had higher first serum creatinine (p = 0.03) and lower first hemoglobin levels (p = 0.00). shows the characteristics of patients with stable and decreasing UV.
Table 2. Demographic and clinical characteristics according to changes in UV over time.
Assessment of baseline UF in 467 patients showed no significant correlation with patient survival and no cutoff points in dichotomous categorization were observed.
In this study, we considered a new variable, net positive fluid removal, which defined as the combination of baseline UV and UF and then we looked at the association between net positive fluid removal (n = 257 patients) and patient survival. Multiple net positive fluid removal cutoffs were assessed, and we observed a significant correlation between net positive fluid removal ≥ 2000 cc/day and <500 cc/day with patient and technique survival.
Multiple Cox regression analysis revealed significant correlation between net positive fluid removal ≥2000 cc/day and higher patient survival [p = 0.01, hazard ratio (HR) = 13.2], higher first serum albumin (albumin ≥ 3.5 mg/dL, p = 0.01, HR = 0.02), lower negative selection (p = 0.0001, HR = 11.8). demonstrate the patient survival curve according to baseline UV, UV over time, and net positive fluid removal, respectively.
DISCUSSION
RRF has been found to be an important predictor of outcome in PD patients. The importance of RRF is probably due to the contribution of native kidneys function in better removal of middle- and large-molecular-weight toxins and organic acids.Citation1 Accurate measurement and the preservation of RRF in PD patients are still a big challenge.
Several studies have shown that patients on PD have a lower risk of RRF loss as compared with hemodialysis patients; however, RRF decreases over time in PD as well.Citation8,14,15,17,18 In fact, there are different factors which influence the rate of RRF decline and consequently the patient’s survival. In our study, we evaluated the different factors that presumably could affect the patient survival. We found that patients with baseline UV > 1000 cc/day had better survival, which is consistent with other studies.Citation1,4,9,19 Interestingly in patients with baseline UV > 1000 cc/day, first serum albumin was higher and first serum creatinine was lower. This may indicate that these patients were referred earlier for starting PD and had better RRF at initiation of dialysis.
This study demonstrated that chronic glomerulonephritis, as a cause of ESRD, higher serum creatinine, and lower hemoglobin levels, were more frequent in patients with declining UV over time. In this study, gender, history of DM, and the presence of comorbidity were not significantly associated with decreased UV.
A retrospective study by Moist et al. who used the Wave 2 database of the USRDS as a study population reported that predictors of RRF loss in PD patients were: time to follow-up, estimated glomerular filtration rate (eGFR) at ESRD onset, female gender, non-White race, DM, and prior history of congestive heart failure.Citation15
Liao et al. in a study showed that, on multivariable analysis, presence of DM, higher baseline residual glomerular filtration rate (rGFR), hypotensive events, use of diuretics, and episodes of peritonitis independently predicted faster decline of rGFR.Citation14
Singhal et al. in a prospective cohort study revealed that DM, larger body mass index, larger dialysate volume, higher rate of peritonitis, higher use of aminoglycoside were associated with more rapid decline of rGFR.Citation17 Johnson et al. in a prospective observational study showed that low baseline RRF, increased body surface area, high dietary protein intake, and DM independently predicted a shorter time to the development of anuria.Citation18 In line with these observations, our previous study, in a subgroup of PD patients with highest response rate and the most completed data from two major PD centers of Tehran, a significant association between diabetes, RRF, and patient survival was found.Citation19 Contrary to these studies, DM was not a risk factor for decreased RRF in this study. This inconsistency could be explained at least in part by low response rate in our national PD registry. The data regarding baseline UV were available only in 32% of the patients and the cause of ESRD was not definite for all the patients.
Our study showed that chronic glomerulonephritis as a cause of ESRD was significantly associated with declining UV. Chronic glomerulonephritis progresses more rapidly compared with other causes of ESRD and it could be considered as a risk factor for rapid loss of RRF in our study.
Patients with higher first serum creatinine demonstrated with a more rapid decline in urine volume. The majority of these patients also had lower baseline urine volume which may express the late referral of these patients for starting PD.
Patients with net positive fluid removal <500 cc/day at the initiation time of PD had more comorbid diseases and most of the patients were selected for CAPD based on negative selection criteria while they had cardiovascular diseases and vascular access problems. This finding emphasizes the importance of positive selection for choosing PD modality as a first modality of renal replacement therapy.
We have to mention that this study was performed on data from the first unpublished report of our national PD registry in 2006. In this regard, baseline UV had been recorded only in 32% of PD patients and the data regarding rGFR were missing. In late 2011, the second report of this registry became available (Najafi I, Alatab S, Atabak S, et al. Seventeen years experience of peritoneal dialysis in Iran; first official report of Iranian PD Registry. Submitted to Perit Dial Int) and the response rate through the CAPD centers from all over the country has increased. Our objective would be to assess this data in the near future and compare it with our previous report.
CONCLUSION
In conclusion, this study showed that higher baseline UV and the preservation of UV over time on PD were associated with better patient survival. We should wait for the second report of our registry and do study on greater sample size.
ACKNOWLEDGMENTS
The authors thank Dr. Abbas Shojaee for providing the Hakim software (Pegahsoft Co.) and also Mrs. Zhila Sarhangi and Zahra Masood Sinaki for their help in data collection.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Tam P. Peritoneal dialysis and preservation of residual renal function. Perit Dial Int. 2009;29(Suppl. 2):S108–S110.
- Li PK, Cheng YL. Therapeutic options for preservation of residual renal function in patients on peritoneal dialysis. Perit Dial Int. 2007;27(Suppl. 2):S158–S163.
- Radulescu D, Ferechide D, Davila C. The importance of residual renal function in chronic dialysed patients. J Med Life. 2009;2:199–206.
- Wang AYM. The heart of peritoneal dialysis: residual renal function. Perit Dial Int. 2007;27:116–124.
- Bargman JM, Thorpe KE, Churchill DN. CANUSA Peritoneal Dialysis Study Group. Relative contribution of residual renal function and peritoneal clearance to adequacy of dialysis: a reanalysis of the CANUSA study. J Am Soc Nephrol. 2001;12:2158–2162.
- Paniagua R, Amato D, Vonesh E, . Mexican Nephrology Collaborative Study Group. Effects of increased peritoneal clearances a mortality rates in peritoneal dialysis: ADEMEX, a prospective, randomized, controlled trial. J Am Soc Nephrol. 2002;13:1307–1320.
- Termorshuizen F, Korevaar JC, Dekker FW, Van Manen JG, Boeschoten EW, Krediet RT. NECOSAD Study Group. The relative importance of RRF compared with peritoneal clearance for patient survival and quality of life: an analysis of the Netherlands Cooperative Study on the Adequacy of Dialysis (NECOSAD)-2. Am J Kidney Dis. 2003;41:1293–1302.
- Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT. NECOSAD Study Group. Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int. 2002;62:1046–1053.
- Wang AYM, Woo J, Wang M, . Important differentiation of factors that predict outcome in peritoneal dialysis patients with different degrees of residual renal function. Nephrol Dial Tranplant. 2005;20:396–403.
- Szeto CC, Wong TYH, Chow KM, Leung CB, Li PKT. Are peritoneal dialysis patients with and without residual renal function equivalent for survival study? Insight from a retrospective review of the cause of death. Nephrol Dial Transplant. 2003;18:977–982.
- Shin SK, Noh H, Kang SW, . Risk factors influencing the decline of residual renal function in continuous ambulatory peritoneal dialysis patients. Perit Dial Int. 1999;19:138–142.
- Wang AYMW, Wang M, Woo J, . Inflammation, residual kidney function and cardiac hypertrophy are interrelated and combine adversely to enhance mortality and cardiovascular death risk of peritoneal dialysis patients. J Am Soc Nephrol. 2004;15:2186–2194.
- Wang AY, Wang M, Woo J, . A novel association between residual renal function and left ventricular hypertrophy in peritoneal dialysis patients. Kidney Int. 2002;62(2):639–647.
- Liao CT, Shiao CC, Huang JW, . Predictors of faster decline of residual renal function in Taiwanese peritoneal dialysis patients. Perit Dial Int. 2008;28(Suppl. 3):S191–S195.
- Moist LM, Port FK, Orzol SM, . Predictors of loss of residual renal function among new dialysis patients. J Am Soc Nephrol. 2000;11:556–564.
- Najafi I, Hakemi M, Safari S, . The story of continuous ambulatory peritoneal dialysis in Iran. Perit Dial Int. 2010;30:430–433.
- Singhal MK, Bhaskaran S, Vidgen E, Bargman M, Vas SI, Oreopoulos DG. Rate of decline of residual renal function in patients on continuous peritoneal dialysis and factors affecting it. Perit Dial Int. 2000;20:429–438.
- Johnson DW, Mudge DW, Sturtevant JM, . Predictors of decline of residual renal function in new peritoneal dialysis patients. Perit Dial Int. 2003;23:276–283.
- Hakemi MS, Golbabaei M, Nassiri A, . Predictors of patient survival in continuous ambulatory peritoneal dialysis 10-year experience in 2 major centers in Tehran. Iran J Kidney Dis. 2010;4:44–49.