Abstract
A 14-month-old girl was admitted to our clinic due to failure to thrive. Her weight and height were below the third percentile for age. Laboratory examination showed signs of alkalosis, hypokalemia, and hypochloremia. However, her urinalysis was consistent with renal tubular acidosis. Radiologic examination showed signs of active rickets. Based on clinical and laboratory findings, we focused on the probable diagnosis of cystinosis. Slit-lamp examination of the cornea confirmed our diagnosis. We should note that the presence of alkalosis does not exclude the possibility of diagnosis of cystinosis and we should be aware that if any slight doubt of cystinosis exists, patients should be carefully and completely evaluated for diagnosis.
INTRODUCTION
Cystinosis is an autosomal recessive metabolic disease characterized by disorder of lysosomal transport of cystine.Citation1 The estimated incidence for cystinosis is one in 100,000–200,000 live births.Citation1 There is a defective function of the lysosomal membrane protein, cystinosin. The responsible gene is CTNS. Three phenotypic forms of cystinosis (nephropathic, juvenile-onset, and benign adult forms) are well recognized. All three forms of the disease are caused by mutations of the CTNS gene and have phenotypic overlap.Citation2 Nephropathic (infantile) cystinosis is the most common and the most severe clinical expression of the disease.Citation3
Nephropathic cystinosis in an untreated child is characterized by renal tubular Fanconi syndrome, poor growth, hypophosphatemic rickets, impaired glomerular function, and accumulation of cystine crystals in almost all cells, leading to tissue destruction.Citation4 Cystinosis accounts for 5% of childhood renal failure.Citation5
In rare cases, biochemical findings compatible with Bartter syndrome can occur. In the literature, there are ten cases reported of cystinosis associated with Bartter syndrome.Citation6–13
Herein, we reported further one case presented with alkalosis but diagnosed as cystinosis.
CASE REPORT
A 14-month-old girl presented to our clinic with the complaint of failure to thrive. It was said that up to 6 months she was well, but after that she did not gain weight. She was born term and her mother’s pregnancy and delivery were uncomplicated. It was reported that in those days she had polydipsia. Lately, there were restlessness and vomiting. The parents were second-degree relatives and healthy. Her 3-year-old sister was healthy. There was no child death in the family.
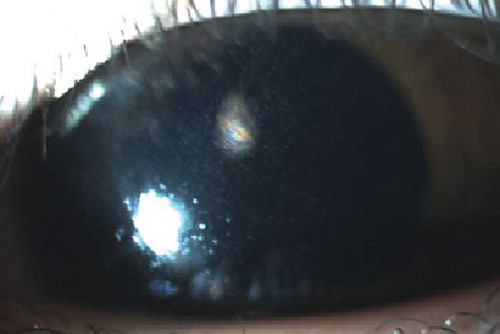
Upon physical examination, her weight was 6000 g (<third percentile) and height was 64 cm (<third percentile). Blood pressure was 85/50 mmHg, pulse rate was 110 beats/min, and temperature was 37°C. She was hypotonic. Her ankles and wrists were wide. Complete blood count revealed hemoglobin (Hb) 13.3 g/dL, hematocrit (Htc) 39.4%, white blood cell count (WBC) 24,300 per mm3 with normal platelets of 339,000 per mm3. Urinalysis revealed a specific gravity of 1.002 and pH of 8; glucose and protein were 1(+). In microscopic examination, there were abundant leukocyte and leukocyte clusters. Serum sodium level was 132 mEq/L, potassium 2.88 mEq/L, chloride 91.9 mEq/L, urea 12 mg/dL, creatinine 0.3 mg/dL, calcium 10.9 mg/dL, phosphorus 2 mg/dL, alkaline phosphatase 850 U/L, and glucose 71 mg/dL. From liver function tests, AST was 56 U/L and ALT was 16 U/L. Thyroid function tests were normal. The arterial blood gas analysis showed alkalosis (pH 7.51, PO2: 122 mmHg, PCO2: 17.6 mmHg, HCO3: 19 mmol/L). Radiologic examination of the wrists showed signs of active rickets (). Renal ultrasonographic examination revealed increased echodensity of renal parenchymas. The presenting clinical and laboratory findings mostly supported renal Fanconi syndrome, but there was an alkalosis. However, in the literature there were patients with similar findings initially diagnosed as Bartter syndrome but later diagnosed as cystinosis. Due to our patient’s high urine pH and low urine density, we suspected cystinosis from renal tubular acidosis. So we referred our patient for ophthalmologic examination. In her ophthalmologic examination, slit-lamp examination of the cornea showed cystine crystal deposition (). The patient was diagnosed with cystinosis and she was referred to pediatric endocrinology and nephrology for treatment and follow-up.
DISCUSSION
Cystinosis is a disease characterized by deposition of cystine crystals in various cells. Tissue damage accompanies the intracellular cystine accumulation, with the greatest effects seen in the kidney.Citation14 When compared with other lysosomal storage diseases, cystinosis cases are entirely normal at birth. Earliest manifestations involve complication of renal Fanconi syndrome and growth retardation. In childhood, it is the most common identifiable cause of renal Fanconi syndrome.Citation14 Cystinosis accounts for 5% of childhood renal failure.Citation5 Kidneys progressively lose function of their proximal tubular transporters; as a result, urinary loss of water, sodium, potassium, bicarbonate, calcium, magnesium, phosphate, amino acids, glucose, proteins, and many other solutes occurs.Citation2 Diagnostic criteria for cystinosis are renal Fanconi syndrome along with cystine crystals in cornea and/or high leukocyte cystine levels.Citation1
At the age of 6 months, full-blown Fanconi syndrome is usually present and causes clinical symptoms of polyuria, thirst, failure to thrive, growth retardation, vomiting, periods of dehydration, constipation, and rickets in some patients.Citation2
Biochemically, there are hypokalemia, hypophosphatemia, metabolic acidosis, low serum uric acid, low carnitine, and, sometimes, hyponatremia.Citation1 Occasionally, hypokalemia in combination with hypochloremic metabolic alkalosis and elevated plasma renin activity can mimic Bartter syndrome. In the literature, there were ten cases reported who presented with alkalosis.Citation6–13 However, most of them were diagnosed to have Bartter syndrome initially and cystinosis later.
In our patient, urinalysis showed the findings of Fanconi syndrome; high urinary pH and low urine density were consistent with renal tubular acidosis. She showed hypokalemia, hypophosphatemia, and alkalosis. In the radiologic examination of the wrists, there were signs of active rickets. Based on the clinical findings and information from the literature, we suspected the diagnosis of cystinosis. Also, the ophthalmologic examination confirmed our diagnosis. In patients with cystinosis, there are increased levels of cystine in leukocytes or fibroblasts.Citation5 However, in some patients, increased levels of cystine crystals are also found in tissues (e.g., cornea, bone marrow). In our patient, we reached the final diagnosis by showing cystine crystals in the cornea.
In conclusion, we know that the diagnosis of cystinosis is frequently delayed due to initial incomplete presentation. Therefore, in all infants with growth retardation we should exclude renal Fanconi syndrome. However, we should note that the presence of alkalosis does not exclude the diagnosis of cystinosis. We should be aware that cystinosis patients can present initially with laboratory findings of Bartter syndrome. In suspected cases, we should evaluate for corneal examination and/or leukocyte cystine levels.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Gahl WA, Thoene JG, Schneider JA. Cystinosis. N Engl J Med. 2002;347:111–121.
- Wilmer Martijn J, Schoeber JP, van den Heuvel LP, Levtchenko EN. Cystinosis: practical tools for diagnosis and treatment. Pediatr Nephrol. 2011;26:205–215.
- Kalatzis V, Antignac C. New aspects of the pathogenesis of cystinosis. Pediatr Nephrol. 2003;18:207–215.
- Nesterova G, Gahl WA. Cystinosis. In: Pagon RA, Bird TD, Dolan CR, eds. GeneReviewsTM [Internet]. Seattle, WA: University of Washington; 1993–2001.
- Middleton R, Bradbury M, Webb N, O’Donoghue D, Van’t Hoff W. Cystinosis. A clinicopathological conference. “From toddlers to twenties and beyond” Adult-Pediatric Nephrology Interface Meeting, Manchester 2001. Nephrol Dial Transplant. 2003;18:2492–2495.
- Berio A. Nephropathy caused by cystinosis with secondary Bartter’s syndrome. Personal experience in a case treated with prolonged diet therapy and acetylsalicylic acid therapy. Minerva Pediatr. 1978;30:1825–1831.
- O’Regan S, Mongeau JG, Robitaile P. A patient with cystinosis presenting with the features of Bartter syndrome. Acta Pediatr Belg. 1980;44:638–646.
- Lemire J, Kaplan BS. The various renal manifestations of the form of cystinosis. Am J Nephrol. 1984;4:81–85.
- Whyte MP, Shaheb S, Schanaper HW. Cystinosis presenting with features suggesting Bartter syndrome. Case report and literature review. Clin Pediatr (Phila). 1985;24:447–451.
- Pennesi M, Marchetti F, Crovella S, . A new mutation in two siblings with cystinosis presenting with Bartter syndrome. Pediatr Nephrol. 2005;20:217–219.
- Yildiz B, Durmus-Aydogdu S, Kural N, Bildirici K, Basmak H, Yarar C. A patient with cystinosis presenting transient features of Bartter syndrome. Turk J Pediatr. 2006;48:260–262.
- Çaltik A, Akyüz SG, Erdogan O, Bülbül M, Demircin G. Rare presentation of cystinosis mimicking Bartter’s syndrome: reports of two patients and review of the literature. Renal Failure. 2010;32:277–280.
- Özkan B, Çayır A, Koşan C, Alp H. Cystinosis presenting with findings of Bartter syndrome. J Clin Res Ped Endo. 2011;3(2):101–104.
- Gahl WA. Cystinosis. In: Avner ED, Harmon WE, Niaudet P, Yoshikawa N, eds. Pediatric Nephrology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2009:1019–1027.