Abstract
Acquired Bartter-like syndrome (BLS), characterized by hypokalemic metabolic alkalosis, hypomagnesemia, hypocalcemia, and normal kidney function, can be induced by diuretics or antibiotics. It is a very rare condition and only anecdotal cases mostly in adults were reported. Although tubulopathy associated with colistin was reported in adults, to the best of our knowledge, colistin-associated BLS neither in adults nor in children has been reported in the literature. We here report a-28-week, 740 g female preterm infant who developed BLS just after colistin treatment for Acinetobacter baumannii infection and recovered few days after the drug cessation, and discuss the possible association of colistin and tubulopathy. More research on colistin pharmacokinetics and pharmacodynamics in critically ill patients and preterm infants is needed to guide adequate colistin dosing at the least toxicity.
INTRODUCTION
Bartter syndrome (BS) is caused by defective salt reabsorption in the thick ascending limb of the loop of Henle, and is characterized by renal salt wasting, hypokalemia, metabolic alkalosis, hyperreninemic hyperaldosteronism with normal blood pressure, and hyperplasia of the juxtaglomerular apparatus.Citation1 It is a hereditary condition which is transmitted as autosomal recessive (Bartter types 1–4) or dominant traits (Bartter type 5).Citation2
Acquired Bartter-like syndrome (BLS), characterized by hypokalemic metabolic alkalosis, hypomagnesemia, hypocalcemia, and normal kidney function, can be induced by diuretics or antibiotics such as capreomycin, viomycin, amphotericin B, cyclosporine, cisplatin, and aminoglycosides. BLS is a very rare condition and only anecdotal cases generally in adults were reported.Citation3–5
Colistin use has been reported in treatment of neonatal multidrug resistant Acinetobacter baumannii infections.Citation6 Renal toxicity is the most common adverse effect of colistin treatment because the drug is excreted primarily by the kidneys, and elevated blood levels of colistin may further impair renal function.Citation7 Although tubulopathy associated with colistin was reported in adults, to the best of our knowledge, colistin-associated BLS neither in adults nor in children was reported in the literature. We here report a preterm infant who developed BLS just after colistin treatment and recovered few days after the drug cessation, and discuss the possible associations of tubulopathy and colistin use.
CASE REPORT
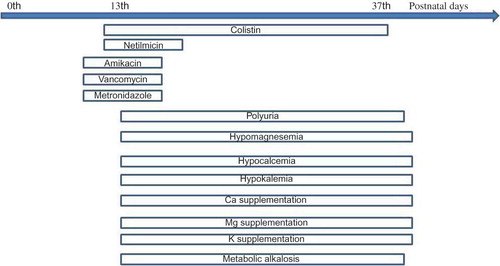
A 28 week, 740 g female preterm infant was born to a 28-year-old mother by cesarean section. The patient received surfactant followed by respiratory support as nasal continuous positive airway pressure and oxygen for 5 days. On postnatal 10th day, she had necrotizing enterocolitis and vancomycin at a dose of 20 mg/kg/day, amikacin at a dose of 10 mg/kg/day and metronidazole at a dose of 7.5 mg/kg/day as combined antibiotherapy was commenced. After the isolation of Acinetobacter baumannii in blood culture, therapy was changed to colistin at a dose of 5 mg/kg/day and netilmicin at a dose of 2.6 mg/kg/day which have been administered for 26 and 7 days, respectively, according to repeated blood culture results.
On the postnatal 13th day, the neonate had weight loss, polyuria (8 cc/kg/h) in the presence of normal blood pressure, and laboratory tests revealed hypokalemic metabolic alkalosis with hypocalcemia (5.5 mg/dL, N: 9–10.6 mg/dL) and hypomagnesemia (1.3 mg/dL, N: 1.6–2.6 mg/dL). Serum sodium and chloride concentrations were within the normal limits. Urine analysis revealed hypercalciuria (urine Ca/creatinine: 2.3, N: <0.8) and excessive renal potassium loss (13 mEq/L, N: <10 mEq/L) without natriuresis. Renal ultrasonography was normal. Serum renin (54 ng/mL/h, N: 0.5–1.9) and serum aldosterone (198 ng/dL, N: 3.4–27) levels were high. Clinical condition was mimicking Bartter type 5. Antibiotics and caffeine were thought to be the underlying cause of electrolyte imbalance due to acquired tubulopathy of the patient. Potassium, calcium, and magnesium levels could be kept within normal ranges with intravenous supplementation. However, she continued to lose weight due to excessive polyuria. On the seventh day of treatment, caffeine and Netilmicin were stopped, and the patient was fed full enterally with 180 mL/kg/day breast milk without intravenous fluids, but her polyuria was still present. Polyuria and her need for potassium, calcium, and magnesium discontinued after 2 and 7 days, respectively, following the cessation of colistin on the postnatal 37th day (). The patient was discharged with normal laboratory results and a body weight of 1580 g on the postnatal 61th day.
DISCUSSION
Drugs like furosemide, cisplatin, carbenicillin, cyclosporine, amphotericin, prolonged administration of gentamicin, capreomycin, and streptomycin have been known to cause possible defects in the thick ascending loop of Henle. However, neither BS nor BLS associated with colistin has been reported in the literature. To the best of our knowledge, this is the first report of a BLS who was associated with colistin in a newborn. Initiation and cessation of colistin therapy as seen in coincided BLS manifestations in our patient. Urine chloride, vitamin D, and prostaglandin E2 levels were not measured in our patient, which are the limitations of the presented case.
Only scant information is available on the mechanism of toxicity, but in vitro electrophysiological studies demonstrated that at long exposure times, colistin was directly toxic to mammalian urothelium by increasing transepithelial conduction.Citation7 It is possible that colistin, similar to aminoglycosides, may directly activate the calcium sensing receptor in the thick ascending loop of Henle and the distal tubule, resulting in hypokalemia, metabolic alkalosis, hypocalcemia, hypomagnesemia, and hypercalciuria.Citation7,8
Colistin has been reported to cause hypokalemia. It is known that numerous drugs can cause a shift of potassium from the extracellular to intracellular compartment, but the total body potassium content usually remains normal. Hypokalemia may sometimes be apparently minor, but should not be underestimated. Indeed, clinicians should be aware that the extent and consequences of hypokalemia may vary in clinical practice depending on factors such as co-morbidity, co-prescribed medications, drug dosage, or regimen.Citation4
A disparity between old and recent studies exists in the reported rates of nephrotoxicity associated with intravenous administration of colistin. The recent studies generally indicate a relatively lower incidence of renal toxicity. Moreover, the wide range of reported nephrotoxicity rates probably reflects more the varying definitions of renal failure than the actual effect of colistin. Colistin-induced nephrotoxicity is mostly mild and reversible. Renal replacement therapy is occasionally required and permanent kidney damage is rarely seen. Still, deteriorating renal function remains an independent factor predicting treatment failure and increased mortality. The observed association between duration of colistin treatment and BLS in our patient suggests that shortening the duration of treatment for specific infections could decrease the incidence of nephrotoxicity. It must be emphasized that dosage and frequency of colistin administration must be adjusted for tubulopathies beside serum creatinine levels and thus require close monitoring of renal function. Finally, the decision to stop colistin treatment on the basis of renal dysfunction must be weighed against the consequences of withholding a potentially life-saving antibiotic.Citation7
The paucity of pharmacologic information regarding colistin administration in the critically ill newborn impedes the creation of optimal dosing regimens that reconcile adequate antibacterial activity with minimal toxicity. Colistin pharmacokinetics are expected to be dramatically altered in critically ill patients, because they are frequently prone to large swings in distribution of volume, fluctuations in renal clearance, and variable protein binding.Citation7 We suggest that more research on colistin pharmacokinetics and pharmacodynamics in critically ill preterm infants is needed to guide adequate colistin dosing at the least toxicity.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Lee BH, Cho HY, Lee H, Genetic basis of Bartter syndrome in Korea. Nephrol Dial Transplant. 2012;27(4):1516–1521.
- Reinalter SC, Jeck N, Peters M, Seyberth HW. Pharmacotyping of hypokalaemic salt-losing tubular disorders. Acta Physiol Scand. 2004;181(4):513–521.
- Chen YS, Fang HC, Chou KJ, Gentamicin-induced Bartter-like syndrome. Am J Kidney Dis. 2009;54(6):1158–1161.
- Ben Salem C, Hmouda H, Bouraoui K. Drug-induced hypokalemia. Curr Drug Saf. 2009;4(1):55–61.
- Chrispal A, Boorugu H, Prabhakar AT, Moses V. Amikacin-induced type 5 Bartter-like syndrome with severe hypocalcemia. J Postgrad Med. 2009;55(3):208–210.
- Celik IH, Oguz SS, Demirel G, Erdeve O, Dilmen U. Outcome of ventilator-associated pneumonia due to multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa treated with aerosolized colistin in neonates: a retrospective chart review. Eur J Pediatr. 2012;171(2):311–316.
- Spapen H, Jacobs R, Van Gorp V, Troubleyn J, Honoré PM. Renal and neurological side effects of colistin in critically ill patients. Ann Intensive Care. 2011;1(1):14.
- Chou CL, Chen YH, Chau T, Lin SH. Acquired Bartter-like syndrome associated with gentamicin administration. Am J Med Sci. 2005;329(3):144–149.