Abstract
Renal involvement is an unusual but significant Behcet´s disease (BD) complication and AA amyloidosis appears to be the most common etiology. IL-6 is a pro-inflammatory cytokine with an important role in AA amyloidosis development. Tocilizumab (TCZ) is a humanized anti-IL-6 receptor antibody that has emerged as an effective and specific treatment in AA amyloidosis secondary to chronic inflammatory disorders. We report on a patient diagnosed with BD who developed nephrotic syndrome caused by renal AA amyloidosis with an excellent response to TCZ therapy.
INTRODUCTION
Behçet’s disease (BD) is a multisystemic vasculitis that causes mucocutaneous, ocular, gastrointestinal, neurological, respiratory, cardiovascular, and renal involvement.Citation1
Renal involvement in BD covers a wide clinical spectrum, from asymptomatic hematuria/proteinuria to end-stage chronic kidney disease. AA amyloidosis secondary to chronic systemic inflammation appears to be the most common form of renal disease in BD.Citation2
BD treatment is based on the affected organs, the extent of the disease, and symptom severity. The treatment goals in this disease are to alleviate the symptoms, decrease inflammation to prevent its progression, reduce flare-up frequency and severity, and prevent complications. Corticosteroids combined with immunosuppressive therapy have been used to reduce inflammation and control symptoms, albeit unsuccessfully in the most aggressive cases.Citation1
Recently, interleukin-receptor antagonists have become a more specific treatment for AA amyloidosis secondary to chronic inflammatory disorders.Citation3
We describe a patient diagnosed as having BD 16 years ago, developed nephrotic syndrome caused by renal AA amyloidosis. She showed an excellent response to humanized anti-IL-6 receptor antibody tocilizumab (TCZ) therapy.
CASE REPORT
A 51-year-old female patient was diagnosed with BD 16 years ago with genital and oral ulcerations and erythema nodosum. She was treated with low-dose corticosteroids. She suffered from iridocyclitis 9 years ago, with no new signs of disease activity since then.
The patient had mild renal failure and subnephrotic proteinuria for a year; rectal biopsy was negative. Proteinuria increased and she was admitted for a new evaluation.
Physical examination was normal, with no edema, mucocutaneous lesions, respiratory symptoms, or fever; blood pressure was 120/80 mmHg. An eye examination did not reveal any inflammatory findings.
Family history was unremarkable.
shows the most relevant laboratory data.
Table 1. Laboratory data.
Immune test, including C3-C4, ANCA, anti-GMB, ANA, anti-DNA, anti-cardiolipin antibodies, lupus anticoagulant antibodies, and cryoglobulins, was normal/negative. HLA B51 was positive. Viral serology tests (hepatitis B virus, hepatitis C virus, and HIV) were negative and CMV and EBV serology tests showed prior exposure. Quantiferon was positive and skin tuberculin test was negative. Chest X-ray and chest CT were normal.
Kidney ultrasound revealed normal-sized kidneys with good corticomedullary differentiation; echo Doppler scan: preserved flow in both renal veins and normal resistive index.
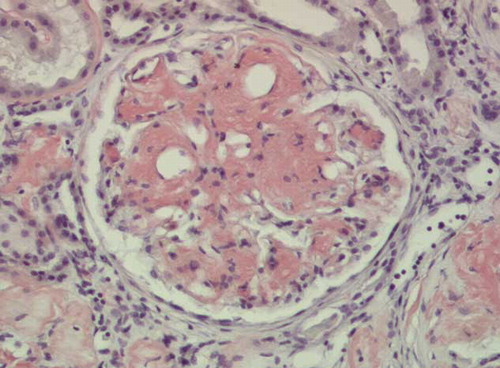
Percutaneous renal biopsy (35 glomeruli) showed five sclerotic glomeruli and amyloid deposit in the remaining 30%, 50% with global distribution, and the rest with a focal segmental pattern; amyloid was also seen in vascular walls, tubular basement membranes and interstitium. These deposits were confirmed as positive for AA amyloid by immunohistochemistry; immunofluorescence was negative ().
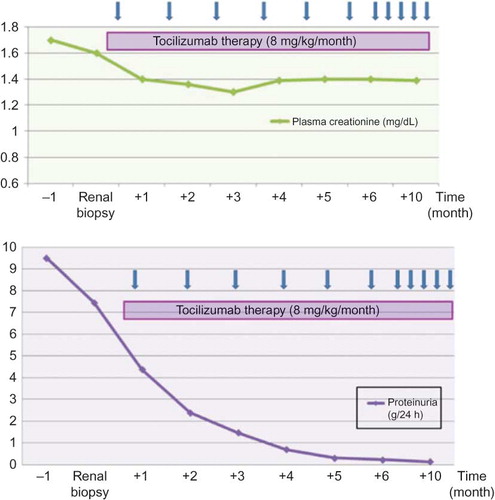
The patient was treated with colchicine (1 mg/day) and TCZ (8 mg/kg body weight/month) for a year; isoniazid was also administered prophylactically for latent tuberculosis for 6 months. After the second dose of TCZ, the proteinuria decreased from 9.5 g/24 h to 2.19 g/24 h and C-reactive protein (CRP) levels from 52.8 mg/dL to <5 mg/dL.
shows creatinine and proteinuria follow-up.
At the 1-year follow-up, laboratory test revealed the following: creatinine 1.4 mg/dL, albumin 4.4 g/dL, CRP < 5 mg/dL, total cholesterol 201 mg/dL (LDL-cholesterol 117 mg/dL), urine protein 165 mg/24 h, and normal sediment. There have been no adverse reactions to TCZ.
DISCUSSION
Clinically apparent renal involvement in BD is uncommon, although subclinical manifestations (microalbuminuria and increased beta-2 microglobulin excretion) are not as rare.Citation4 Renal disease in BD may be classified into 5 groups: (a) glomerulonephritis (diffuse proliferative, focal and segmental, IgA, membranous proliferative, and other); (b) amyloidosis; (c) renal vascular disorder; (d) interstitial nephritis; and (e) others, such as nephrotoxicity.Citation5
AA amyloidosis is an infrequent but significant BD complication. Although published data in the literature are limited, it appears to be the most common cause of renal disorder and renal failure in BD; its estimated prevalence is 0.04–3%.Citation6 BD-related amyloidosis is more common in Mediterranean countries, and in Turkey, it accounts for 3.6% of secondary amyloidosis, although some of these patients may have Familial Mediterranean fever mutations.Citation7
Akpolat et al.Citation8 have published one of the largest series, with 33 patients diagnosed with BD and renal involvement. Of these, 11 patients present AA amyloidosis and, unlike our case, almost 90% are males. These authors analyze 253 published cases, of which 108 include amyloidosis. The mean interval between BD and AA amyloidosis diagnosis is 11 years (range from 7-month to 30-year); this time is shorter in men than in women.Citation9 In our case, the interval between the onset of the first symptom of BD and the diagnosis of amyloidosis was 16 years and 9 years, respectively, with no BD clinical manifestations. In BD, amyloidosis usually occurs in patients with peripheral artery disease, lung disorders, and arthritis,Citation10 and it is not common to find cases such as this, with mucocutaneous and eye involvement alone.Citation6
BD pathogenesis is not clearly established; apparently, environmental factors act on a genetic predisposition, which leads to immune activation with an accompanying inflammatory response. There seems to be a complex interaction between T cells, neutrophils, and antigen-presenting cells, with cytokine release.Citation11
Hamzaoui et al. have analyzed the cytokine profile in BD patients and have noted that the blood levels of IL-4, IL-6, IL-10, IL-12, and IFN-γ cytokines were significantly higher in BD patients compared with the control subjects. IL-4, IL-10, and IL-12 levels were similar between the patients with active BD and BD in remission, whereas IL-6 and IFN-γ levels were higher in patients with active BD. Therefore, patients with active BD exhibit higher IL-6 levels, and these are correlated with the degree of disease activity.Citation12
IL-6 is a pro-inflammatory cytokine with an important role in immune response regulation and acute phase response; it stimulates serum amyloid A (SAA) synthesis in the liver and plays a key role in AA amyloidosis development.Citation13
TCZ has been approved as a biological therapy for several autoimmune and chronic inflammatory diseases. TCZ inhibits IL-6 pro-inflammatory activity, thus reducing SAA production, and also interferes with T-cell function.Citation14
This patient had an excellent response to TCZ therapy, with a fast decrease in proteinuria and improvement/stabilization of renal function. This response to TCZ suggests that IL-6 has a more direct effect on the glomerular filtration barrier.Citation3 Colchicine in BD is indicated for joint and mucocutaneous involvement, but does not appear to prevent or affect the course of the amyloidosisCitation10; therefore, we believe that the dramatic improvement in proteinuria was due to TCZ. To the best of our knowledge, this would be the first BD-related AA amyloidosis case treated with TCZ.
We conclude that TZC may be the treatment of choice for nephrotic syndrome secondary to renal AA amyloidosis in BD patients, and it could change the unfavorable outcome in amyloidosis.
Declararion of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Mendes D, Correia M, Barbedo M, . Behçet’s disease—a contemporary review. J Autoimmun. 2009;32:178–188.
- Belmouaz S, Sechet A, Fernandez B, . Tubulo-interstitial nephritis with Fanconi syndrome in Behçet disease. Nephrol Dial Transplant. 2007;22:2079–2083.
- Magro-Checa C, Navas-Parejo Casado A, Borrego-García E, . Successful use of tocilizumab in a patient with nephrotic syndrome due to a rapidly progressing AA amyloidosis secondary to latent tuberculosis. Amyloid. 2011;18:235–239.
- Sahin I, Noyan T, Karaman E, Yalçmkaya AS, Metin A, Akpolat T. Mild renal injury in Behçet´s Disease. Ren Fail. 2004;26:55–57.
- Nadir I, Gültekin F, Yönem O, Yildiz EA. Behçet case with renal amyloidosis. Ren Fail. 2003;25:323–326.
- Kutlay S, Civriz S, Ensari A, Nergizoglu G, Ates K, Karatan O. Development of amyloidosis in Behçet’s syndrome with isolated mucocutaneous involvement. Rheumatol Int. 2004;24:37–39.
- Kosemehmetoglu K, Baydar DE. Renal amyloidosis in Behçet´s disease: clinicopathologic features of 8 cases. Int Urol Nephrol. 2012; Sep 9. [Epub ahead of print].
- Akpolat T, Dilek M, Aksu K, . Renal Behçet’s disease: an update. Semin Arthritis Rheum. 2008;38:241–248.
- Skhiri H, Mahjoub S, Harzallah O, . Secondary amyloidosis, a fatal complication of Behçet´disease: three case reports. Saudi J Kidney Dis Transpl. 2004;15:57–60.
- Melikoglu M, Altiparmak MR, Fresko I, . A reappraisal of amyloidosis in Behçet´syndrome. Rheumatology. 2001;40:212–215.
- Pay S, Simşek I, Erdem H, Dinç A. Immunopathogenesis of Behçet’s disease with special emphasize on the possible role of antigen presenting cells. Rheumatol Int. 2007;27:417–424.
- Hamzaoui K, Hamzaoui A, Guemira F, Bessioud M, Hamza M, Ayed K. Cytokine profile in Behçet’s disease patients. Relationship with disease activity. Scand J Rheumatol. 2002;31:205–210.
- Evereklioglu C, Er H, Türköz Y, Cekmen M. Serum levels of TNF-alpha, sIL-2R, IL-6, and IL-8 are increased and associated with elevated lipid peroxidation in patients with Behçet’s disease. Mediators Inflamm. 2002;11:87–93.
- Hirano T, Ohguro N, Hohki S, . A case of Behçet’s disease treated with a humanized anti-interleukin-6 receptor antibody, tocilizumab. Mod Rheumatol. 2012;22:298–302.