Abstract
Purpose: To describe the epidemiologic features of acute renal failure related to pregnancy (PRARF) and to evaluate its prognostic impact. Methods: Retrospective study conducted in a Tunisian intensive care unit over a period of 17 years (1995–2011). Women were included if they were more than 20 weeks pregnant and were admitted to the ICU during pregnancy or immediately (<7 d) post partum. PRARF was defined by a serum creatinine level >0.8 mg/dL and was classified as mild (0.9 to 1.4 mg/dL), moderate (1.5 to 2.9 mg/dL) or severe (>3 mg/dL). Results: Five hundred and fifty patients were included. Mean age was 31 ± 6 years. Mean SOFA score was 4 ± 3. PRARF was diagnosed in 313 patients (56.9%). ARF was mild in 215 cases (39.1%), moderate in 65 cases (11.8%) and severe in 33 cases (6%). Main causes leading to this complication were preeclampsia (66.5%) and acute hemorrhage (27.8%). Only two patients (0.4%) developed chronic renal failure and needed long-term dialysis. Patients who developed this complication had higher SOFA score (4.7 ± 3.5 vs. 3.2 ± 2.1; p < 0.001). Thirty-three patients (6%) died in the ICU. The rate of ICU mortality was significantly higher in patients with PRARF (9.3 vs. 1.7%; p < 0.001). Conclusions: PRARF is associated with higher mortality. Thus, appropriate monitoring of pregnancies is needed in order to prevent its onset by an early and prompt management of the underlying risk factors.
Introduction
Acute renal failure (ARF) has become a rare complication of pregnancy in developed countries. In fact, since 1960, the incidence of this complication has been reduced significantly, and currently affects 1 per 15,000–20,000 pregnancies.Citation1,Citation2 Available data in the literature dealing with this topic are very heterogeneous as different definitions were proposed, ranging from serum creatinine levels of >0.8 mg/dL to daily dialysis requirement.Citation1 Moreover, epidemiologic data of pregnancy-related acute renal failure (PRARF) in developing countries are scanty and may differ from those of developed countries where the legislation of abortion have lead to the reduction in the number of septic abortion.Citation3,Citation4
The aim of our study is to describe the epidemiologic features of acute renal failure related to pregnancy and to evaluate its prognostic impact.
Materials and methods
Setting
The study was conducted in our 22-beds intensive care unit (ICU) of the “Habib Bourguiba University Hospital” – Sfax (Tunisia) over a period of 17 years (from 1995 to 2011). Patients admitted in our unit come from Sfax City (1.2 million inhabitants) and other cities of south Tunisia.
Patients
Women were included if they were more than 20 weeks pregnant and were admitted to the ICU during pregnancy or immediately (<7 d) post partum. Exclusion criteria were the following:
Gestational age <20 weeks.
Evidence of renal impairment prior to pregnancy or history of renal stone disease.
Elevated serum creatinine prior to gestation.
Small size of the kidneys on ultrasonography.
Data collection
All medical records of included patients were retrospectively reviewed. The clinical severity was evaluated by Simplified Acute Physiology Score II (SAPSII)Citation5 and the Sequential Organ Failure Assessment (SOFA) scoreCitation6 calculated within the first 24 h of intensive care unit stay. For each patient, the following data were recorded on admission:
Demographic parameters: age, gestational age and total number of pregnancies.
Cause of admission in ICU: Severe pre-eclampsia, eclampsia, hemorrhagic shock, sepsis (puerperal or not) and/or acute fatty liver of pregnancy (AFLP).Citation7–9
Intrapartum complications: HELLP syndrome, retroplacental hematoma, disseminated intravascular coagulation.Citation10,Citation11
Modalities of delivery (planned vaginal or urgent/planned cesarean delivery).
Clinical parameters on admission in ICU: body temperature, respiratory rate, systolic and diastolic blood pressure (SBP/DBP) and heart rate. Hypotension was defined as a systolic blood pressure <80 mmHg whereas severe arterial hypertension was defined by a SBP ≥160 mmHg and/or a DBP ≥110 mmHg.
Biological findings on admission: plasmatic sodium and potassium levels, hemoglobin levels, platelets count, prothrombin levels, serum aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels and plasmatic bilirubin levels.
Therapeutic measures on admission and during ICU stay: mechanical ventilation, anticonvulsants, antihypertensive medications, magnesium sulfate, transfusion, and vasopressors.
Evaluation of renal function
Renal function was assessed by blood urea nitrogen and serum creatinine levels on admission. Acute renal failure related to pregnancy was defined by a serum creatinine level >0.8 mg/dL. According to serum creatinine level on admission, the severity of acute renal failure (ARF) was classified as mild (0.9 to 1.4 mg/dL), moderate (1.5 to 2.9 mg/dL) or severe (>3 mg/dL).Citation12 For each patient suffering ARF, the underlying causes were recorded.
Follow-up and outcome
For each patient, we recorded the duration of mechanical ventilation, the length of ICU stay and issue in ICU (death or survival).
For patients with ARF, we also recorded if they needed further dialysis after ICU discharge.
Statistical analysis
Qualitative variables were expressed as percentages whereas quantitative variables were expressed as means ± standard deviation (SD). The normal distribution of quantitative variables was checked by using the Kolmogorov–Smirnov test. Two groups were compared: those with ARF (ARF (+) group) and those without ARF (ARF (−) group). Baseline characteristics of the two studied populations were compared by the chi-square test or Fisher exact test for qualitative variables and Student’s t-test or Mann–Whitney test for quantitative variables as appropriate. The one-way ANOVA test was used to evaluate the prognostic impact of ARF according to its severity (mild, moderate or severe) in terms of severity scores, duration of mechanical ventilation, length of ICU stay, and ICU mortality. The area under the receiver-operating-characteristics curve (ROC) was calculated to evaluate the prognostic significance of serum creatinine level. All tests were two-sided. The level of significance was set at p < 0.05.
Results
Demographic characteristics
During the study period, 726 pregnant women were admitted in our ICU. Only 550 patients were included in our study (7 had previous renal disease, 22 were in the first trimester of pregnancy (<20 weeks), 21 had severe hypertension prior to pregnancy and 126 were excluded because of lacking data about renal function). The mean age was 31 ± 6 years ranging from 17 to 45 years. Two hundred and sixty four patients (48%) were primigravid. Median number of total pregnancies was 2 ranging from one to 10 pregnancies. Main previous medical diseases were diabetes for 20 patients (3.6%), mitral or aortic diseases for 19 patients (3.5%), asthma for 5 patients (0.9%) and epilepsy for 6 patients (1.1%).
All our patients were admitted in our ICU just after delivery. Leading cause for ICU admission were preeclampsia for 354 patients (64.4%), eclampsia for 154 patients (28%), hemorrhagic shock for 144 patients (26.2%), HELLP syndrome for 96 patients (17.5%), severe sepsis for 23 patients (4.2%) and acute pregnancy fatty liver for 32 patients (5.8%). Several complications were diagnosed during labor or delivery: retro-placental hematoma in 88 patients (16%), immediate postpartum hemorrhage in 59 patients (10.7%) and uterine rupture in 18 patients (3.3%). Modalities of delivery were vaginal delivery in 129 cases (23.4%), planned cesarean in 30 cases (5.5%) and urgent cesarean in 391 cases (71.1%).
Clinical and biological findings on admission
Mean SAPSSII was 21.8 ± 10.3 whereas mean SOFA score was 4 ± 3. On admission, mean temperature was 37.5 ± 0.9°C. Mean systolic blood pressure was 136 ± 28 mmHg (ranging from 60 to 206 mmHg) whereas mean diastolic blood pressure was 52 ± 21 mmHg (ranging from 30 to 13 mmHg). Mean Heart rate was 108 ± 26 beats per minute. Eighty-five patients (15.5%) were hypotensive. Two hundred and seventy-four patients (49.8%) were under mechanical ventilation when admitted in our ICU. For patients with spontaneous breathing, mean respiratory rate was 22 ± 8 per minute.
Biological findings on admission are summarized in .
Table 1. Biological findings on admission in ICU.
Therapeutic measures during ICU stay
On admission, 176 patients (32%) needed vasopressors whereas 175 patients (31.8%) needed antihypertensive medication. Sedation and mechanical ventilation were required for 274 patients (49.8%). Mean duration of mechanical ventilation was 3.3 ± 4.4 d ranging from 1 to 29 d. Transfusion was required for 213 patients (38.7%). Anticonvulsants (benzodiazepine and/or phenobarbital) were given to 187 patients (34%) and 190 patients (34.5%) received magnesium sulfate.
Evaluation of renal function
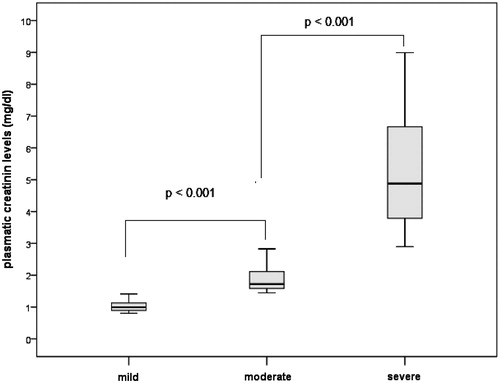
Even though the incidence of acute renal failure (defined by a serum creatinine level >0.8 mg/dL) overall decreased during the last decade, an important epidemiologic heterogeneity was observed. In fact, the highest incidence was recorded in 1995 (90.9%) whereas the lowest incidence was recorded in 2004 (26.7%) (). Among the included patients, 313 developed a PRARF (56.9%). Mean serum creatinine level was significantly higher in patients with acute renal failure (1.7 ± 1.5 mg/dL vs. 0.6 ± .01 mg/dL; p < 0.001). Similarly, mean serum level of blood urea nitrogen (BUN) was significantly higher in this group of patients (9 ± 6.9 mmol/L vs. 4.8 ± 3.7 mmol/L; p < 0.001). Acute renal failure was mild in 215 cases (39.1%), moderate in 65 cases (11.8%) and severe in 33 cases (6%). There was a significant difference of mean serum creatinine levels between these groups (). Main causes leading to this complication were preeclampsia and acute hemorrhage (). Nine patients (1.7%) required hemodialysis whereas 2 patients (0.4%) required plasma exchange because of thrombotic microangiopathies. Only two patients (0.4%) developed chronic renal failure and needed long-term dialysis.
Figure 1. Evolution of the incidence of acute renal failure during from 1995 to 2011 in our intensive care unit.
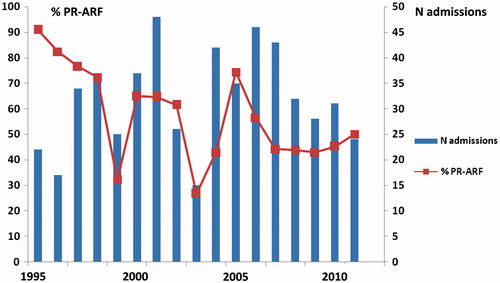
Table 2. Etiology of obstetric acute renal failure.
Baseline characteristics
When the two studied groups (PRARF (+) and PRARF (−)) were compared, there was no significant difference in terms of demographic characteristics (). However, patients who developed acute renal failure had higher SAPSII score (23.7 ± 11.5 vs. 19.4 ± 7.7; p < 0.001) and higher SOFA score (4.7 ± 3.5 vs. 3.2 ± 2.1; p < 0.001). The incidence of this complication was significantly higher in patients who were hypotensive on admission (72.9% vs. 54%; p = 0.001) and/or who required urgent transfusion during the first 24 h (65.7% vs. 51.3%; p = 0.001). Need of mechanical ventilation did not differ between PRARF (+) and PRARF (−) patients (respectively 47.9% and 52.1%; p = 0.223). Analysis of biological findings on admission in ICU showed that patients who developed this complication had significantly higher plasmatic potassium rates and a significantly more pronounced metabolic acidosis. This group of patient had also significantly higher levels of bilirubin and leucocytes ().
Table 3. Comparison of PRARF (+) and PRARF (−) according to demographic characteristics.
Table 4. Comparison of PRARF (+) and PRARF (−) according to biological findings on admission.
Prognosis impact of PRARF
In patients requiring ventilator support, mean duration of mechanical ventilation was significantly higher in the PRARF (+) group (3.9 ± 4.8 d vs. 2.4 ± 3.6 d; p = 0.013). The overall mean duration of length of stay in ICU was 2.8 ± 4.2 d, ranging from 1 to 30 d. This duration was also significantly higher in PRARF (+) group (3.5 ± 4.9 d vs. 2 ± 2.9 d; p < 0.001). Mean duration of mechanical ventilation, mean duration of length of ICU stay, as well as the severity score on admission significantly increased according to the severity of PRARF ().Thirty-three patients (6%) died in the ICU. The rate of ICU mortality was significantly higher in patients with PRARF (9.3 vs. 1.7%; p < 0.001). Mortality increased according to the severity of PRARF (5.6% in patients with mild PRARF, 10.8% in patients with moderate PRARF and 30.3% in patients with severe PRARF; p < 0.001). Moreover, a serum creatinine level higher than 1 mg/dL on admission predicted death with a sensitivity of 72% and a specificity of 66% ().
Figure 3. ROC curve showing the correlation between serum creatinine level and ICU mortality (area under curve = 0.761).
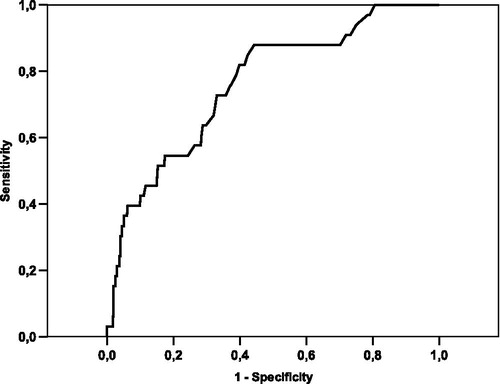
Table 5. Prognosis impact of PRARF.
Discussion
Obstetric acute renal failure can be defined as a sudden decrease in renal function during pregnancy or after delivery. While the occurrence of this challenging complication become rare in developed world, available epidemiological data in the literature about PRARF in developing countries are scarce.Citation1,Citation2 In our series, the incidence of PRARF was 56.9% of cases, which is too high compared to previous studies reporting an incidence ranging from 4.2 to 25%.Citation13–16 This may be explained by different adopted thresholds to define acute renal failure. In fact, Goplani et al.Citation14 defined PRARF by a serum creatinine level higher than 2 mg/dL or by a documented oliguria (urine output <400 mL per day) and they reported an incidence of 9.06%. According to this definition, the diagnosis of this complication in our study would be considered only in 111 of our patients (20.2%). Nevertheless, all these epidemiologic data confirm that the incidence of PRARF remains quietly higher in developing countries than developed countries where the incidence ranges from 1 to 2.8%.Citation15,Citation16 Thus, the discrepancy of epidemiological data can be related to different studied population (particularly different ethnics), different management procedures and different definitions. In 2004, the Acute Dialysis Quality Initiative (ADQI) group developed RIFLE criteria through a broad consensus of the expert.Citation17 However, the use of this classification, which focuses on the plasma creatinine percentage change and on the development of oliguria, is not consensual and further studies are needed to demonstrate its usefulness in pregnant women.Citation2
In our study, main causes responsible of PRARF were preeclampsia (66.5%) and acute bleeding (27.8%) while septic events were incriminated in only 4.2% of the cases. This may be explained by the fact that the Tunisian legislation allows abortion during the first three months of pregnancy since 1965. Bentata et al.Citation18 reported similar results as these two etiologies were responsible of 75% of PRARF. However, Goplani et al.Citation14 reported that puerperal sepsis was the most common etiological factor leading to ARF (61.5%). This may be explained by the difference between the studied populations in terms of gestational age. In fact, in the latter study, 20% of included patients presented in early pregnancy while all our patients were admitted just after delivery.
In our study, patients with PRARF had significantly higher severity scores with higher incidence of hypotension and higher need of transfusion. Moreover, this group of patients had significantly higher duration of mechanical ventilation and length of ICU stay. This finding highlights the importance of this complication as a prognosis marker during late pregnancy and postpartum period. Moreover, the onset of acute renal failure was significantly associated with several metabolic disturbances, particularly a decreased serum bicarbonate levels and increased serum potassium levels. Bentata et al.Citation19 reported that patients with PRARF had higher rate of hypotension, icterus, hyperuricemia, thrombocytopenia and hepatic cytolysis which can be explained by higher incidence of HELLP syndrome, DIC and abruption placenta as leading causes for ICU admission in this group of patients.
The overall ICU mortality in our study was 6%. However, PRARF onset was associated with significantly higher mortality (9.3 vs. 1.7%; p < 0.001). Moreover, mortality was correlated with the severity of the PRARF. A serum creatinine level higher than 1 mg/dL on admission predicted death with a sensitivity of 72% and a specificity of 66%. Our mortality is lower than that reported by Bentata et al.Citation19 and Goplani et al.Citation14 (respectively 28.3% and 18.6%). However, this may be related to the important proportion of patients with mild PRARF in our study. In fact, in patients with severe PRARF, we found a mortality as high as 30.3%).
Even though our study represents one of the rare studies reporting epidemiologic data about PRARF in African countries several limitations must be highlighted. First, we conducted a retrospective study during a seventeen years period with important changes in therapeutic management of acute kidney injury in critically ill patients, including pregnant women. Second, all included patients were admitted in our ICU just after delivery and all pregnant women who experienced PRARF during the early pregnancy were managed by nephrologists. Thus, the epidemiologic data describing incriminated causes of acute renal failure concern only this particular group of patients. However, the high ICU mortality in patients with moderate or severe PRARF indicates that there is substantial scope for improvement in maternity-care to prevent such complication.
Conclusion
Even though the incidence of pregnancy-related acute renal failure decreased in Tunisia during the last years, it still frequently complicates the course of pregnancy with different degrees of severity. This challenging complication is associated with longer ICU stay and higher mortality. Thus, appropriate monitoring of pregnancies is needed in order to prevent PRARF onset by an early and prompt management of the underlying risk factors. This can be reached with more accessible prenatal care, wide implementation of emergency obstetric care, safe abortion services and improvement of operative techniques.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Gammill HS, Jeyabalan A. Acute renal failure in pregnancy. Crit Care Med. 2005;33(10 Suppl):S372–S384
- Machado S, Figueiredo N, Borges A, et al. Acute kidney injury in pregnancy: a clinical challenge. J Nephrol. 2012;25(1):19–30
- Stratta P, Canavese C, Dogliani M, Todros T, Gagliardi L, Vercellone A. Pregnancy-related acute renal failure. Clin Nephrol. 1989;32(1):14–20
- Turney JH, Marshall DH, Brownjohn AM, Ellis CM, Parsons FM. The evolution of acute renal failure, 1956–1988. Q J Med. 1990;74(273):83–104
- Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–2963
- Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–1800
- Brown MA, Lindheimer MD, de Swiet M, Van Assche A, Moutquin JM. The classification and diagnosis of the hypertensive disorders of pregnancy: statement from the International Society for the Study of Hypertension in Pregnancy (ISSHP). Hypertens Pregnancy. 2001;20(1):IX–XIV
- Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2007;24(1):CD002252
- Devarbhavi H, Kremers WK, Dierkhising R, Padmanabhan L. Pregnancy-associated acute liver disease and acute viral hepatitis: differentiation, course and outcome. J Hepatol. 2008;49(6):930–935
- Martin JN Jr, Rose CH, Briery CM. Understanding and managing HELLP syndrome: the integral role of aggressive glucocorticoids for mother and child. Am J Obstet Gynecol. 2006;195(4):914–934
- Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M; Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Hemostasis (ISTH). Towards definition, clinical and laboratory criteria and a scoring system for disseminated intravascular coagulation. Thromb Hemost. 2001;86(5):1327–1330
- Galvagno SM Jr, Camann W. Sepsis and acute renal failure in pregnancy. Anesth Analg. 2009;108(2):572–575
- Selcuk NY, Tonbul HZ, San A, Odabas AR. Changes in frequency and etiology of acute renal failure in pregnancy (1980–1997). Ren Fail. 1998;20(3):513–517
- Goplani KR, Shah PR, Gera DN, et al. Pregnancy-related acute renal failure: a single-center experience. Indian J Nephrol. 2008;18(1):17–21
- Prakash J, Tripathi K, Pandey LK, Sahai S, Usha, Srivastava PK. Spectrum of renal cortical necrosis in acute renal failure in eastern India. Postgrad Med J. 1995;71:208–210
- Kumar KS, Krishna CR, Siva Kumar V. Pregnancy related acute renal failure. J Obstet Gynecol India. 2006;56:308–310
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute Dialysis Quality Initiative workgroup. Acute renal failure -- definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8(4):R204–R212
- Bentata Y, Housni B, Mimouni A, Abouqal R. Obstetric acute renal failure in an intensive care unit in Morocco. Int J Gynaecol Obstet. 2011;115(2):196–198
- Bentata Y, Housni B, Mimouni A, Azzouzi A, Abouqal R. Acute kidney injury related to pregnancy in developing countries: etiology and risk factors in an intensive care unit. J Nephrol. 2012;25(5):764–775