Abstract
Objective: To investigate the incidence and risk factors of contrast-induced nephropathy (CIN) in patients receiving coronary angiography (CAG) in a Chinese medical center. Methods: The medical records of the patients receiving CAG at Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiaotong University from January 2008 to July 2009 were collected to analyze the incidence of CIN under different conditions and the clinical difference between CIN group and non-CIN group. Results: There were 487 cases enrolled in this study and the total incidence of CIN was 10.5%. Through Mehran risk score stratification, incidence of CIN increased with risk scores and in an extremely high-risk group it was as high as 18.0%. Multi-factor regression analysis showed that preoperative hypotension, heart failure, anemia and low estimated glomerular filtration rate (≤30 mL/min) were risk factors of CIN after CAG. Conclusion: CIN post CAG is associated with preoperative hypotension, heart failure, anemia and renal function. Close attention should be paid to CIN in patients receiving CAG.
Introduction
In the 1970s, contrast-induced nephropathy (CIN) was considered a major complication after coronary angiography (CAG) with incidence as high as 50%.Citation1 In recent 30 years, medical safety has been highly valued, and hospital-acquired kidney injuries mainly include major postoperative, drug-induced renal diseases and CIN. With the rapid development of imaging and interventional treatment, contrast media are more and more extensively used. As a result, CIN has become the third largest cause for hospital-acquired acute kidney injury.Citation2
The incidence of CIN varies by the diagnostic criterion, about 3 to 14%, and can reach as high as 20% in high-risk patients.Citation3–5 In patients with CIN post-CAG, the risk of long-term mortality and heart attack of patients with CIN is increasing.Citation6–8 These days more and more works on CIN after CAG have been published, including the mechanism and prevention studies. But there is not so much clinical data about CIN post-CAG from China.
In this study a clinical survey on CIN was conducted in patients receiving CAG or percutaneous coronary intervention (PCI) in a Chinese medical center.
Subjects and methods
Subjects
The patients receiving CAG or PCI from 1 January 2008 to 31 July 2009 were enrolled in this study at Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiaotong University. Those patients receiving electrophysiological examination and left ventricular ablation were excluded. This study was approved by the ethical committee of Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiaotong University.
Diagnostic criteria
According to the diagnostic definition of CIN, if levels of serum creatine (SCr) rose more than 44.2 μmol/L (0.5 mg/dL) or 25% over the baseline level 48∼72 h after receiving contrast media, while other affecting factors were excluded, the case will be diagnosed with CIN.Citation9 Cardiac function was graded by the grading scheme of New York Heart Association (NYHA).
Estimated glomerular filtration rate (eGFR) was calculated according to simplified CG formula: CG-eGFR: Ccr =[(140 − age) × weight × (0.85 female)]/(72 × SCr).
Mehran risk scores for prediction of CIN after PCI were calculated according to the reference.Citation10 The CIN risk score variables included patient-related characteristics (i.e., age >75 years, diabetes mellitus, heart failure, or admission with acute pulmonary edema, hypotension, anemia, and chronic kidney disease) and procedure-related characteristics (i.e., the use of elective intraaortic bloon pump or increasing volumes of contrast media).Citation10
Grouping
Patients were divided into CIN group and non-CIN group according to whether they had CIN based on preoperative baseline SCr and at postoperative 48 h SCr.Citation10 After stratification according to Mehran risk scores, patients with risk score no less than 6 points or eGFR no more than 60 mL/min were divided into high-risk groups, otherwise will be divided into low-risk groups respectively. Patients with CIN were further defined as isotonic contrast media group, or hypotonic contrast group.
Contents and methodology of study
The clinical information of the enrolled patients, included gender, age, history of hypertension and diabetes, the value of preoperative hemoglobin (Hb), hematocrit (Hct), serum total cholesterol (TC) and triglyceride (TG), fasting glucose, 2-h postprandial blood sugar, preoperative SCr, blood urea nitrogen (BUN), serum uric (UA) acid and postoperative SCr within 72 h.
During and after CAG or interventional surgery, contrast media type, dosage, imaging results, type of PCI and the duration of CAG were recorded.
Statistical analysis
Data were processed by using software SPSS 13.0 (Chicago, IL). Each parameter was subject to single-factor analysis and Logistic regression analysis. p-Value <0.05 was considered as statistically significant.
Results
Basic data
A total of 487 patients were enrolled. Among them patients with hypertension accounted for 69.2% (7.6% for grade 1, 21.1% for grade 2, and 40.5% for grade 3, respectively). About 29.2% patients were found diabetes, 2.1% impaired glucose tolerance, 93.8% coronary atherosclerosis, 41.5% acute myocardial infarction (AMI), 2.9% sub-AMI, and 12.1% kidney disease.
Patients with history of cerebrovascular accidents accounted for 10.5%, and patients with heart failure or AMI KillipI-IV accounted for 34.3%. In this study, NYHA-IV and KillipI-IV were regarded as the same risk score. Patients with NYHA-I or Killip-I accounted for 21.4%, NYHA-II or Killip-II 5.7%, NYHA-III or Killip-III 5.3%, NYHA-IV or Killip-IV 1.8%.
Incidence of CIN in patients receiving CAG or PCI
In the 487 patients, 51 cases had SCr increased more than 25% of the baseline value, and the incidence of CIN was 10.5% (51/487). After stratification by risk score, the incidence increased significantly with increasing risk score. The incidences in high-risk and low-risk groups were 12.7 and 4.0%, respectively. Because the elevation of SCr may be resulted from postoperative heart failure attack, incidence of CIN should be recalculated by excluding cases with heart failure attack. The adjusted incidence was 7.5% (35/487), and among them incidences in high-risk and low-risk groups were 3.2 and 9.1%, respectively ().
Table 1. Comparison of incidences of CIN through risk score stratification.
Comparison of laboratory parameters between CIN group and non-CIN group
Hb, Hct, SCr, TC, LDL, serum phosphorus, calcium, eGFR, and left ventricular mass index (LVMI) in CIN group and non-CIN group were subject to independent t test respectively. The results showed significant in Hb and Hct (p < 0.05), while no significant difference in SCr, TC, eGFR, LVMI, phosphorus and calcium between the two groups (p > 0.05), as shown in .
Table 2. Comparison of clinical parameters between CIN group and non-CIN group.
Wilcoxon rank sum test showed that there was significant difference in hospital stay, heart failure, serum glycated albumin (GA), d-dimer (DD), brain natriuretic peptide (BNP), C-reactive protein (CRP), aspartate aminotransferase (AST), creatine phosphokinase (CPK), lactate dehydrogenase (LDH), creatine phosphokinase MB (CKMB), cardiac troponin I (cTnI) and ejection fraction (EF) between CIN group and non-CIN group (p < 0.05) ().
Risk factor analysis
Patients were grouped by the criteria shown in the table (conditions not less than 75 years of age, preoperative hypotension, intraaortic balloon pump (IABP), heart failure including AMI with varying degrees of pulmonary congestion, anemia, diabetes, and eGFR no more than 30 mL/min). Chi-square test results of the incidence of CIN in the two groups (group meeting the conditions and not meeting the conditions in the table) suggested that preoperative hypotension, heart failure, anemia and eGFR ≤ 30 mL/min were all risk factors of CIN after CAG, as shown in . GFR no more than 30 mL/min was also the risk factor of CIN with excluding patients with postoperative heart failure attack ().
Table 3. Chi-square test results of the incidence of CIN by risk factors.
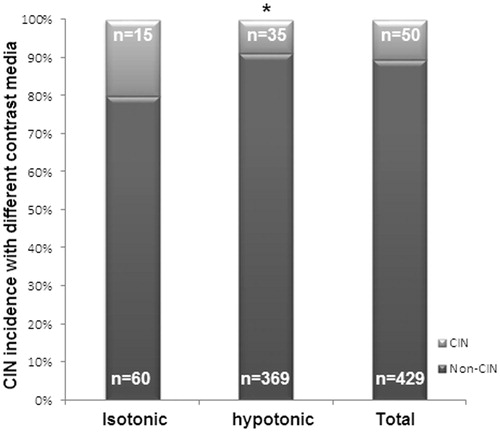
Comparison of the incidence of CIN caused by different contrast media
The results suggested that the risk of CIN in patients using isotonic contrast media (n = 15, 20%) was significantly higher than those using hypotonic contrast media (n = 35, 8.7%) (p < 0.05) as shown in .
Multi-factor analysis of CIN risk factors
Further Logistic regression analysis was performed to evaluate the clinic indexes shown in as risk factors including age, sex (male = 1, female = 0), weight, length of hospital stay, PCI times, cardiac function grading, Hb, Hct, urinary red blood cell count, urinary specific gravity, albumin (ALB), SCr, BUN, eGFR, the maximum dose of contrast media, the number of involved vessels, the number of implanted stents, and emergency PCI, stay in cardiac care unit (CCU), urine protein, preoperative hypotension, IABP, diabetes, diabetic nephropathy, angiotensin convert enzyme inhibitors (ACEI)/angiotensin II receptor I blockers (ARB) use, gout, isotonic contrast media, diuretics, AMI and hydration (value of the following variables: exposure, positive = 1, unexposed, negative = 0), all of which were covered as regression factors. The results suggested that male, emergency PCI, heart failure, ALB, BUN, diuretics and eGFR were risk factors of CIN after CAG, while weight and Hb were protective factors ().
Table 4. Logistic regression analysis of CIN incidence-related factors.
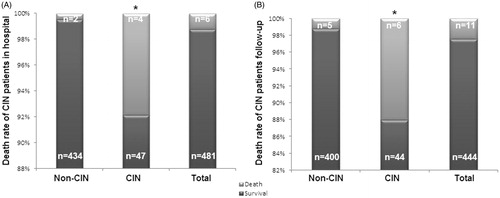
Prognosis
There were four patients (7.8%) with CIN and two (0.5%) patients without CIN died from sudden cardiac arrest, cardiac shock, hypovolemic shock, respiratory failure, heart or renal failure during their hospital stay (p < 0.05), as shown in . There was significant difference between the death rate during follow-up time in CIN group (n = 6, 12%) and non-CIN group (n = 5, 1.2%) (p < 0.05). There was one patient who received maintenance hemodialysis in CIN group while two patients received maintenance hemodialysis in non-CIN. There were 11 patients that died and three patients that received maintenance hemodialysis among the enrolled 458 cases with complete follow-up information up to 28 Feb 2010. The causes of the death included cardiac shock, heart failure, respiratory failure and renal failure.
Discussion
CIN is an important cause for hospital-acquired acute renal failure, whose total incidence is about 3 to 14%.Citation5 In high-risk patients with renal insufficiency, diabetes and other risk factors, the incidence of CIN is even high up to 20%.Citation5,Citation11 A single-center prospective study found that the incidence of CIN in patients with CAG and interventional treatment was 8.7%.Citation12
In this study the incidence of CIN in patients receiving CAG or PCI was 10.5%. Stratification by Mehran risk score suggested that the incidence of CIN increased with increasing risk score, and reached up to 18.0% in a very high-risk group, which was relatively low compared with the Mehran forecast (57%).Citation10 The incidence of CIN in the low-risk group was 4.0%, which indicated that the incidence of CIN in low-risk populations was very low.
In single-factor analysis, this study verified the eight major risk factors first proposed by Mehran, and suggested that preoperative hypotension, heart failure, anemia and GFR ≤ 30 mL/min were all risk factors for CIN.Citation10 The results revealed that the incidence in isotonic group was higher than that in the hypotonic group may be due to small number of cases and most of those patients who selected isotonic media were high-risk.Citation13–15
Our results indicated that CIN is closely associated with preoperative hypotension, heart failure, anemia, renal function, and some clinical indicators. Close attention should be paid and effective approaches should be taken to prevent the occurrence of CIN in the future.Citation16,Citation17 Prevention strategy of CIN post-CAG requires the identification of high-risk patients, elimination of those factors that could increase risk, intervention to minimize risk, careful follow-up and proper treatment to the kidney injury.Citation18
Declaration of interest
The authors report no conflicts of interest. This work was sponsored by the National Natural Science Foundation of China (81100528 and 81270824), Science and Technology Commission of Shanghai Municipality (114119a6100), the New 100-talent Plan of Shanghai Jiaotong University School of Medicine.
References
- Mehran R, Nikolsky E. Contrast-induced nephropathy: definition, epidemiology, and patients at risk. Kidney Int. 2006;100:S11–S15
- Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–936
- Bartholomew BA, Harjai KJ, Dukkipati S. Impact of nephropathy after percutaneous coronary intervention and a method for risk stratification. Am J Cardiol. 2004;93:1515–1519
- Abe M, Kimura T, Morimoto T. Incidence of and risk factors for contrast-induced nephropathy after cardiac catheterization in Japanese patients. Circ J. 2009;73:1518–1522
- Best PJ, Lennon R, Ting HH. The impact of renal insufficiency on clinical outcomes in patients undergoing percutaneous coronary interventions. J Am Coll Cardiol. 2002;39:1113–1119
- Lindsay J, Canos DA, Apple S. Causes of acute renal dysfunction after percutaneous coronary intervention and comparison of late mortality rates with postprocedure rise of creatine kinase-MB versus rise of serum creatinine. Am J Cardiol. 2004;94:786–789
- Solomon RJ, Mehran R, Natarajan MK, et al. Contrast-induced nephropathy and long-term adverse events: cause and effect? Clin J Am Soc Nephrol. 2009;4:1162–1169
- Kong DG, Hou YF, Ma LL, et al. Comparison of oral and intravenous hydration strategies for the prevention of contrast-induced nephropathy in patients undergoing coronary angiography or angioplasty: a randomized clinical trial. Acta Cardiol. 2012;67(5):565–569
- Morcos SK. Prevention of contrast media nephrotoxicity – the story so far. Clin Radiol. 2004;59:381–389
- Mehran R, Aymong ED, Nikolsky E, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44:1393–1399
- Rundback JH, Nahl D, Yoo V. Contrast-induced nephropathy. J Vasc Surg. 2011;54:575–579
- Wang L, Ni ZH, He B, et al. Urinary IL-18 and NGAL as early predictive biomarkers in contrast-induced nephropathy after coronary angiography. Nephron Clin Pract. 2008;108:c176–c181
- Liss P, Nygren A, Erikson U, et al. Injection of low and iso-osmolar contrast medium decreases oxygen tension in the renal medulla. Kidney Int. 1998;53:698–702
- Seeliger E, Flemming B, Wronski T, et al. Viscosity of contrast media perturbs renal hemodynamics. J Am Soc Nephrol. 2007;18:2912–2920
- Jost G, Pietsch H, Lengsfeld P, et al. The impact of the viscosity and osmolality of iodine contrast agents on renal elimination. Invest Radiol. 2010;45:255–261
- Mueller C, Buerkle G, Buettner HJ, et al. Prevention of contrast media-associated nephropathy: randomized comparison of 2 hydration regimens in 1620 patients undergoing coronary angioplasty. Arch Intern Med. 2002;162:329–336
- Shaw A. Models of preventable disease: contrast-induced nephropathy and cardiac surgery-associated acute kidney injury. Contrib Nephrol. 2011;174:156–162
- Solomon R, Dauerman HL. Contrast-induced acute kidney injury. Circulation. 2010;122:2451–2455