Abstract
Introduction: End-stage renal disease is the most debilitating condition for patients with renal diseases. Cardiovascular disease is the leading cause of death in these patients. It has been shown that nitric oxide (NO) increases in renal failure and hemodialysis patients and could be correlated with cardiovascular diseases in this population. Objectives: To investigate the relation between exhaled nitric oxide (eNO) and left ventricular performance in chronic hemodialysis patients. Methods: In this prospective study, eNO was measured in 20 chronic hemodialysis patients (13 males and 7 females with the mean age of 45.20 ± 14.99 years). Left ventricular findings were studied by conventional and Doppler echocardiography. eNO correlation with the echocardiographic parameters was evaluated. Results: The median eNO was 11.65 ppb (range: 1.9–29.9 ppb). eNO was positively correlated with left ventricular ejection fraction (ρ = 0.561, p = 0.01) and negatively correlated with left ventricular end systolic volume (ρ = −0.451, p = 0.046), isovolumic relaxation time (ρ = −0.448, p = 0.047) and myocardial performance index (ρ = −0.587, p = 0.007). Conclusion: There is a positive correlation between eNO and left ventricular performance in chronic hemodialysis patients. Therefore, eNO may play an important role in pathophysiology of cardiac involvement in these patients.
Introduction
End-stage renal disease (ESRD) is the most debilitating condition for patients with renal diseases. ESRD is defined as irreversible decline in kidney function, when renal replacement therapy is needed for survival. The total number of ESRD patients has been growing dramatically and cardiovascular disease (CVD) has become the leading cause of death in these patients.Citation1–5
There are two groups of cardiovascular risk factors including traditional risk factors-hypertension, diabetes, hyperlipidemia, and smoking and uremia-related risk factors. The latter alters by the uremic state, such as dyslipidemia, prothrombotic factors, hyperhomocysteinemia and characteristic factors of chronic uremia (e.g., hemodynamic overload, anemia and hypoalbuminemia).Citation6 However, the cardiovascular risks in dialysis patients may depend not only on emerging risk factors such as homocysteine or high sympathetic activity but also on a relative lack of vasculoprotective factors. Among these factors, nitric oxide (NO) is normally generated in the endothelium by the enzyme NO synthase (NOS), which transforms l-arginine into NO and citrulline.Citation7–10
NO acts as a signal in the blood vessels and different organs. It has effects on blood vessels, endothelial function and lungs.Citation8 Relation of decreased NO with heart failure and left ventricular hypertrophy (LVH) has also been investigated.Citation11,Citation12 Unopposed action of endothelin and other vasoconstrictor agents can contribute to hypertension and endothelial dysfunction in hemodialysis patients with decreased NO production.Citation8
Although there are clues of relation between NO and a few cardiovascular diseases, few studies have evaluated such association in ESRD patients. It has been shown that asymmetric dimethylarginine (ADMA), a NOS inhibitor, is associated with cardiovascular mortality in ESRD patients.Citation13 Small changes in NO levels may play a role in the progression of renal disease. Low NO production in patients with ESRD undergoing HD has been attributed to the increased ratio of plasma ADMA to arginine, hence higher blood pressure in these patients.Citation14 Excretion of NO in exhaled air of chronic renal failure and hemodialysis patients has been evidently illustratedCitation15–17; exhaled NO (eNO) has been found to be higher in hemodialysis patients with pulmonary hypertension.Citation16 Therefore, in this study we aimed investigating the relation between eNO and left ventricular performance in chronic hemodialysis patients.
Methods
In this prospective study, 20 chronic hemodialysis patients aged between 20 and 60 years were recruited. All patients were on dialysis 3 times a week for at least 2 years. Exclusion criteria were functional class III–IV heart failure, atrial fibrillation, moderate to severe heart valvular diseases, history of coronary artery diseases or previous myocardial infarction, severe pericardial effusion, asthma, chronic obstructive pulmonary diseases, allergic rhinitis, cigarette smoking, using nitrite-containing drugs, systemic or inhaled corticosteroid usage, systemic inflammatory disorders or inability to perform respiratory test.
Measurement of eNO
All patients fasted for at least 12 h before examination. Patients abstained from ingestion of nitrate or nitrate-containing foods (e.g., lettuce) or drinks (e.g., tea or coffee) prior to the eNO measurements. NO concentration in exhaled air (eNO) was determined at rest in a sitting position over 3 h. eNO measurements were performed by an ozone chemiluminescence analyzer (CLD 88sp FENO analyzer, ECOmedics, Duernten, Switzerland) between 8 a.m. and 1 p.m. Measurements were made according to ATS/ERS joint commission guidelines.Citation18 Measurements were performed during expiration following a full inspiration while the each subject exhaling against an oral pressure to ensure closure of uvula. At ordinary room temperature and using a nose-clip, the subjects underwent three repeated measurements of single-breath eNO at a target flow rate of 50 mL/s with intervals of at least 1 min. Measurements with coefficients of variations more than 10% were repeated. Measurements were obtained from 7 to 10 seconds of the plateau phase of expiration. Regular volume and NO calibration were performed according to the manufacturer’s recommendation. The unit of measurement was parts per billion (ppb). The mean value of the three measurements was calculated and used for analysis.
Echocardiographic evaluations
Conventional and pulse-wave tissue Doppler echocardiography was performed by Vivid 7, GE Vingmed, USA within 12 h of dialysis. Left ventricular mass index (LVMI), left ventricular end diastolic volume (LVEDV), left ventricular end systolic volume (LVESV) and left ventricular ejection fraction (LVEF) were measured by conventional echocardiography. Furthermore, isovolumic contraction time, isovolumic relaxation time, and myocardial performance index (MPI) were calculated by tissue Doppler echocardiography. Left ventricular diastolic filling, peak early (E) and late (A) diastolic mitral flow velocities, deceleration time of E wave (DT), systolic (Sm), early diastolic (Em) and late diastolic (Am) lateral mitral annular peak velocities, and the ratio of peak early diastolic mitral flow velocity-to-early diastolic septal mitral annular velocity (E/Em) were recorded.
Data analysis
All data were analyzed using SPSS statistical package version 16.0 (SPSS Inc, Chicago, IL). Data were presented as median and interquartile range (IQR) or mean ± standard deviation (SD). Spearman correlation coefficients were calculated to determine the possible relationships between the eNO and left ventricular function. A p value of 0.05 or less was considered statistically significant.
Results
Study population included 13 males and 7 females with the mean age of 45.20 ± 14.99 years. Underlying renal diseases were hypertension in 8 cases, diabetes mellitus in 4 cases, polycystic kidney disease in 2 cases and with unknown etiology in 6 cases. The mean duration of hemodialysis was 39.00 ± 13.13 months. The median (IQR) of measured eNO was 11.65 (12) ppb (range 1.9–29.9 ppb). eNO was not affected either by age (p = 0.56) or body surface area (p = 0.98).
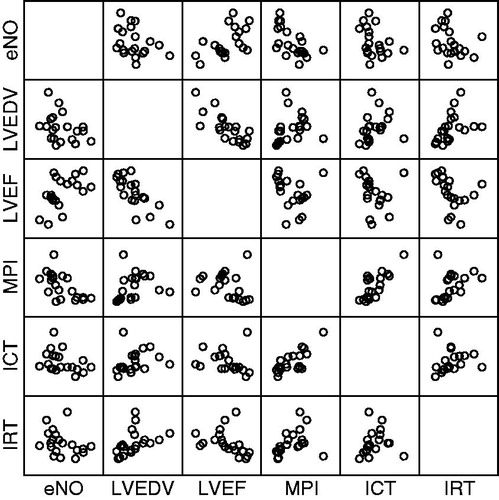
Patients’ echocardiographic or tissue Doppler findings are shown in . eNO had significantly positive correlation with LVEF (ρ = 0.561, p = 0.01) and inverse correlation with LVESV (ρ = −0.451, p = 0.046), isovolumic relaxation time (ρ = −0.448, p = 0.047) and MPI (ρ = −0.587, p = 0.007). There was also an inverse correlation between eNO and isovolumic contraction time which was not statistically significant (ρ = −434, p = 0.056) (). There was no correlation between eNO and other echocardiographic or tissue Doppler findings.
Table 1. Patients’ echocardiographic and tissue Doppler findings.
Discussion
The results of this study revealed that eNO was positively correlated with LVEF, as a surrogate for the cardiac function, in chronic hemodialysis patients. On the other hand, eNO was inversely correlated with MPI, LVESV and isovolumic relaxation time. Nonetheless, eNO tended to have a significant correlation with isovolumic contraction time. These findings might be due to the more sensitivity of MPI, rather than isovolumic relaxation/contraction time or ratio of each of these to ejection time, in detecting the global left ventricular dysfunction.
There are no available studies on the relationship between eNO and cardiac performance in chronic hemodialysis patients. Previous studies showed the significance of time intervals measurements by tissue Doppler study especially MPI for earlier detection of systolic or diastolic ventricular dysfunction in different settings.Citation19–23 Moreover, direct correlation between MPI and systolic and diastolic invasive measurements of ventricular function has been shown;Citation24,Citation25 MPI increases with increasing diastolic or systolic cardiac dysfunction.Citation26
This study illuminates some clues for better understanding of pathophysiological basis of increased cardiovascular diseases in hemodialysis patients. Previous studies investigated the relation between NO/eNO and cardiovascular diseases in chronic kidney disease and hemodialysis. Madore et al.Citation27 reported chronic increase in NO levels associated with maintenance hemodialysis. They also concluded that there was an inverse correlation between eNO and blood pressure in hemodialysis patients.Citation27 Interestingly, Raj and colleagues found elevated fractional eNO prior to the dialysis in patients with dialysis-induced hypotension.Citation28 In contrast, Sumino et al. failed to demonstrate a pivotal role for NO production in arterial blood pressure control in patients with chronic kidney disease.Citation29
Relation of decreased NO production with cardiovascular echocardiographic and clinical parameters has been investigated in conditions other than dialysis. In one study the rate of NO release, measured as eNO, was significantly lower in the patients with moderate-to-severe heart failure than in those with mild heart failure or in normal control subjects. The rate of release was positively correlated with the cardiac index and was negatively correlated with either the systemic or pulmonary vascular resistance.Citation11 Furthermore, positive correlation between cardiac index and NO levels has been shown in cirrhotic patients.Citation30 In experimental studies, correlation between eNO and diastolic dysfunction has been highlighted as well.Citation31
ADMA is an endogenous inhibitor of endothelial NOS which reduces NO availability. In another study among hemodialysis patients, it was observed that ADMA correlated with the mean and relative left ventricular wall thickness and the LVMI, but not the indices of systolic and diastolic function.Citation32 Moreover, positive correlation between ADMA and LVMI, and negative correlation between ADMA and early mitral inflow velocity, early/late mitral inflow velocity, and isovolumetric relaxation time was demonstrated.Citation33
All these studies are in consistent with the finding that NO has significant role in cardiac function. Therefore, increasing NO levels (for instance through l-arginine supplements) might improve the cardiovascular state in hemodialysis patients with low rate of eNO. Recently, the effects homoarginine levels on cardiovascular mortality have been assessed. Marz and coworkers concluded that homoarginine levels were independently associated with cardiovascular and all cause mortality in patients undergoing hemodialysis and in patients referred for coronary angiography.Citation34
Conclusion
This study revealed a positive correlation between eNO and left ventricular performance in chronic hemodialysis patients. Therefore, eNO may play an important role in pathophysiology of cardiac involvement in these patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Acknowledgments
This research was financially supported by Cardiovascular Research Center, Tabriz University of Medical Sciences, Iran. The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
- Murtagh FE, Eddington-Hall J, Higginson IJ. The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis. 2007;14:82–99
- Etemadi J, Zolfaghari H, Firoozi R, et al. Unexplained pulmonary hypertension in peritoneal dialysis and hemodialysis patients. Rev Port Pneumol. 2012;18(1):10–14
- Roberts MA, Polkinghorne KR, McDonald SP, Ierino FL. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am J Kidney Dis. 2011;58:64–72
- Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13:745–753
- Ardalan MR, Ghabili K, Pourabbas R, Shoja MM. A causative link between periodontal disease and glomerulonephritis: a preliminary study. Ther Clin Risk Manag. 2011;7:93–98
- Parfrey PS. Cardiac disease in dialysis patients: diagnosis, burden of disease, prognosis, risk factors and management. Nephrol Dial Transplant. 2000;15(Suppl 5):58–68
- Ardalan MR, Tarzamni MK, Shoja MM, et al. Black tea improves endothelial function in renal transplant recipients. Transplant Proc. 2007;39(4):1139–1142
- Sarkar SR, Kaitwatcharachai C, Levin NW. Nitric oxide and hemodialysis. Semin Dial. 2004;17:224–228
- Ghabili K, Agutter PS, Ghanei M, Ansarin K, Panahi Y, Shoja MM. Sulfur mustard toxicity: history, chemistry, pharmacokinetics, and pharmacodynamics. Crit Rev Toxicol. 2011;41(5):384–403
- Shoja MM, Agutter PS, Tubbs RS, Payner TD, Ghabili K, Cohen-Gadol AA. The role of the renin–angiotensin system in the pathogenesis of intracranial aneurysms. J Renin Angiotensin Aldosterone Syst. 2011;12(3):262–273
- Sumino H, Sato K, Sakamaki T, et al. Decreased basal production of nitric oxide in patients with heart disease. Chest. 1998;113:317–322
- Wenzel S, Rohde C, Wingerning S, Roth J, Kojda G, Schlüter KD. Lack of endothelial nitric oxide synthase-derived nitric oxide formation favors hypertrophy in adult ventricular cardiomyocytes. Hypertension. 2007;49(1):193–200
- Zoccali C, Bode-Böger S, Mallamaci F, et al. Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet. 2001;358(9299):2113–2117
- Schmidt RJ, Domico J, Samsell LS, et al. Indices of activity of the nitric oxide system in hemodialysis patients. Am J Kidney Dis. 1999;34(2):228–234
- Matsumoto A, Hirata Y, Kakoki M, et al. Increased excretion of nitric oxide in exhaled air of patients with chronic renal failure. Clin Sci (Lond). 1999;96(1):67–74
- Yu TM, Chen YH, Hsu JY, et al. Systemic inflammation is associated with pulmonary hypertension in patients undergoing hemodialysis. Nephrol Dial Transplant. 2009;24(6):1946–1951
- Rolla G, Bruno M, Bommarito L, et al. Breath analysis in patients with end-stage renal disease: effect of hemodialysis. Eur J Clin Invest. 2008;38(10):728–733
- American Thoracic Society; European Respiratory Society. ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide. Am J Resp Crit Care Med. 2005;171:912–930
- Chao G, Zheng C, Meng D, et al. Tei index: the earliest detectable cardiac structural and functional abnormality detected in Hb Bart's foetal edema. Int J Cardiol. 2009;134(3):e150–e154
- Kono M, Kisanuki A, Takasaki K, et al. Left ventricular systolic function is abnormal in diastolic heart failure; Reassessment of systolic function using cardiac time interval analysis. J Cardiol. 2009;53(3):437–446
- Greco S, Troisi F, Brunetti ND, Di Biase M. Tei index correlates with tissue Doppler parameters and reflects neurohormonal activation in patients with an abnormal transmitral flow pattern. Echocardiography. 2009;26(9):1012–1018
- Baykan M, Baykan EC, Turan S, et al. Assessment of left ventricular function and Tei index by tissue Doppler imaging in patients with slow coronary flow. Echocardiography. 2009;26(10):1167–1172
- Ajami G, Borzouee M, Amoozgeu H, et al. Evaluation of myocardial function using the Tei index in patients with Kawasaki disease. Cardiol Young. 2010;20(1):44–48
- Lacorte JC, Cabreriza SE, Rabkin DG, et al. Correlation of the Tei index with invasive measurements of ventricular function in a porcine model. J Am Soc Echocardiogr. 2003;16:442–447
- Tei C, Nishimura RA, Seward JB, Tajik AJ. Noninvasive Doppler-derived myocardial performance index: correlation with simultaneous measurement of cardiac catheterization measurements. J Am Soc Echocardiogr. 1997;10:169–178
- Tei C. New non-invasive index for combined systolic and diastolic ventricular function. J Cardiol. 1995;26:135–136
- Madore F, Prud'homme L, Austin JS, et al. Impact of nitric oxide on blood pressure in hemodialysis patients. Am J Kidney Dis. 1997;30(5):665–671
- Raj DS, Vincent B, Simpson K, et al. Hemodynamic changes during hemodialysis: role of nitric oxide and endothelin. Kidney Int. 2002;61(2):697–704
- Sumino H, Satö K, Sakamaki T, et al. Reduced production of nitric oxide during hemodialysis. J Hum Hypertens. 1999;13(7):437–442
- Matsumoto A, Ogura K, Hirata Y, et al. Increased nitric oxide in the exhaled air of patients with decompensated liver cirρsis. Ann Intern Med. 1995;123(2):110–113
- Joffe II, Travers KE, Perreault-Micale CL, et al. Abnormal cardiac function in the streptozotocin-induced non-insulin-dependent diabetic rat: noninvasive assessment with doppler echocardiography and contribution of the nitric oxide pathway. J Am Coll Cardiol. 1999;34(7):2111–2119
- Napora M, Graczykowska A, Próchniewska K, et al. Relationship between serum asymmetric dimethylarginine and left ventricular structure and function in patients with end-stage renal disease treated with hemodialysis. Pol Arch Med Wewn. 2012;122(5):226–234
- Ebinç FA, Erten Y, Ebinç H, et al. The relationship among asymmetric dimethylarginine (ADMA) levels, residual renal function, and left ventricular hypertrophy in continuous ambulatory peritoneal dialysis patients. Ren Fail. 2008;30:401–406
- Marz W, Meinitzer A, Drechsler C, et al. Homoarginine, cardiovascular risk, and mortality. Circulation. 2010;122(10):967–975