Abstract
Purpose: Our aim is to determine the biochemical and histologic changes induced in the kidneys, testis and prostate on possible ischemia and reperfusion (I/R) injury caused by pneumoperitoneum (PNP) in a rat model and to evaluate the ability of protective effects of caffeic acid phenethyl ester (CAPE). Methods: Twenty-eight adult male Wistar albino rats were randomly divided to one of three treatment groups, with seven animals in each group. Sham, laparoscopy (L), and laparoscopy plus CAPE (L + C) group were subjected to 60 min of PNP with 15 mmHg one hour before the desufflation period. Total oxidant status (TOS) and total antioxidant status (TAS) levels were determined in kidney, testis, and prostate. Kidney and testis tissues were removed to obtain a histologic score. Also, Johnsen scoring system was used for testicular tissue analysis. Results: L group had significantly higher TOS and lower TAS levels on kidney and testis compared to the other groups. In prostate biochemical analysis, there was not any difference between groups. No difference was found between groups according to kidney and testis tissues’ histologic evaluation. In evaluation of Johnsen scoring, L group showed significant lower score compared to the other two groups. Conclusions: Increased intraabdominal pressure (IAP) had an oxidative effect on kidney and testis but not on prostate in rats. Moreover, it could affect the testicular Johnsen score. All these adverse effects of IAP on both kidney and testis could be prevented by CAPE administration.
Introduction
Laparoscopy has gradually become the gold standard for the diagnosis and effective treatment of various diseases in both adults and children. At the same time, clinical investigation of intraabdominal pressure (IAP) became of interest since it was first described in the late 19th century.Citation1 Several studies have particularly focused on the effects of IAP on intraabdominal blood flow to hollow and solid organs. Most of the studies show that blood flow to intraabdominal organs is reduced by 10% to 80% during laparoscopy but normalizes after desufflation of the abdominal cavity.Citation1,Citation2 In terms of the hypoperfusion and subsequent reperfusion periods, both clinical and experimental studies reveal that the laparoscopic procedure provides a typical model of ischemia-reperfusion (I/R) injury in the organs.Citation1,Citation3
The adverse outcomes of IAP on the kidneys’ wall have been relatively well described.Citation1 Limited studies revealed that IAP could affect germ cell apoptosis and cause testicular hypoperfusion, free radical production, and subsequent testicular damage during laparoscopic procedures in animal models.Citation3,Citation4 In addition, acute I/R injury had an oxidative effect on prostate tissue.Citation5 However, the effect of increased IAP on the prostate has not been studied until now.
The caffeic acid phenethyl ester (CAPE), an active component of propolis from honeybee hives, is known to have antioxidant, immunomodulatory, anti-inflammatory and anticarcinogenic properties, and has been used as a folk medicine for many years. In literature, CAPE is used for protecting kidneys, testis, and prostate against several toxicities.Citation6 The physiological and pharmacological properties of CAPE were investigated both in vitro and in vivo assays. At a concentration of 10 µM, it completely blocks production of free radicals in human neutrophils and in the xanthine/xanthine oxidase system. The structure–activity relationship has been identified by comparing the potency of free radical scavenging.Citation7 The antioxidant activity of CAPE is to limit the anoxia-reoxygenation-induced mitochondria damage in vitro.Citation8 However, the physiological functions and the underlying protective mechanism of CAPE against increased IAP tissue injury remain totally unclear.
In this study, we aimed to determine the histologic and biochemical changes induced in the kidneys, testis, and prostate on possible tissue injury caused by increased IAP followed by abdominal deflation in a rat model and to evaluate the ability of protective effects of CAPE.
Materials and methods
Animals
This experimental study was conducted with 28 adult male Wistar albino rats of the same age, from the same colony weighing between 270 and 320 g, after approval of the Mustafa Kemal University, Faculty of Medicine, Animal Care and Ethics Committee was obtained before the onset of experiments. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. They were housed separately under specific pathogen-free conditions to avoid infections in macrolon cages, with a 12:12-hour light–dark cycle at 22 ± 0.5 °C room temperature and provided standard laboratory rat chow and tap water ad libitum.
The rats were randomly divided to one of three treatment groups, with seven animals in each group. The control group was subjected to a sham operation without pneumoperitoneum (PNP). The laparoscopy (L) group was subjected to 60 min of PNP with 15 mmHg IAP. The laparoscopy plus CAPE (L + C) group was subjected to 60 min of PNP with 15 mmHg and administered a single intraperitoneal injection of CAPE 10 μmol/kg one hour before the desufflation period.
Surgical procedure
The rats were anesthetized by intraperitoneal administration of ketamine hydrochloride (Ketalar, Pfizer, Turkey) 50 mg/kg and xylazine hydrochloride (Rompun, Bayer, Turkey) 3 mg/kg and then placed at a supine position on the operating table. During the procedure, additional doses were administered if necessary. The experiments were performed in a position allowing spontaneous breathing under sterile conditions. The body temperature was maintained at 37.0 °C with a heat pad to prevent the effects of hypothermia and to maintain the stability of hemodynamic parameters. After proper preparation of the surgical field, an 18 G Abbocath catheter was placed supraumbilically into the abdominal cavity and connected to an insufflator tube.Citation9 PNP was automatically established up to a 15 mmHg pressure for 60 min via the insufflation of CO2 by an abdominal CO2 insufflator (Karl Storz GmbH, Tutlingen, Germany), and followed by immediate desufflation.
Tested drugs
CAPE (Sigma, St. Louis, MO) was administered intraperitoneally to rats in doses of 10 μmol/kg, prior to use, CAPE was dissolves with 10 mL of 70% ethanol.Citation7
Biochemical analysis
Immediately following desufflation, first kidneys, testicles, and prostate were immediately removed, respectively. The excised left kidney, left testis, and prostate tissue were weighed, immediately stored at −80 °C. For biochemical analysis, tissues perfused with 1.15% ice-cold KCl, minced, then homogenized in five volumes (w/v) of the same solution. Assays were performed on the supernatant of the homogenate that was prepared at 14,000 rpm for 30 min at +4 °C. The protein concentration of the tissue was measured by the method of Lowry.Citation10
The levels of the total oxidant status (TOS) and total antioxidant status (TAS) were determined in the supernatants. TAS was determined using a novel automated colorimetric measurement method developed by Erel.Citation11 The TAS results were expressed as mmol Trolox equivalent/g protein for kidney, prostate, and testis tissue.
TOS were measured by Erel’s methods.Citation12 The TOS results were expressed as nmol H2O2 equivalent/mg protein for all tissues.
Histological evaluation
For light microscopic examination, right kidney and right testis tissues of each rat were removed and tissue pieces were fixed in 10% neutral buffered formalin solution, embedded in paraffin, sectioned at 5 µm, and then stained with hematoxylin and eosin (H&E). For statistical analysis, seven sections of kidney tissue and seven sections of testis tissue from each group were prepared. Totally, 48 sections of kidney and testis tissues were examined and photographed with DP 20 camera attached Olympus CX-41 photomicroscope (Olympus Corporation, Tokyo, Japan) for histopathological changes. The prostate tissues were not adequate for histological examination; therefore, only biochemical assessment was done.
To obtain a histologic score of kidney tissues, histopathological changes were graded according to cortical involvement and the severity of the lesions as shown in .Citation13
Table 1. Histologic kidney grading scale.
For testicular tissue analysis, Johnsen scoring systemCitation14 was used. Using 10X objective lens, 10 tubules were scored for each rat. Totally, 50 tubules were evaluated for each group at least. Each seminiferous tubule profile was given a score from 1 to 10 on the basis of the criterion according to Johnsen.
The testis was evaluated histologically with a 4-level grading scale, similar to that described by Erpek et al.Citation15 for the presence of hemorrhage, polymorphonuclear leukocyte infiltration, degeneration of seminiferous epithelium, tubular atrophy, and necrosis in 50 sections per group as shown in .
Table 2. Histologic testes grading scale.
Statistical analysis
The statistical analyses of results were performed using the SPSS (Statistical Package for Social Sciences, Chicago, IL) software version 16. One-way ANOVA was used for the statistical evaluation of TAS and TOS results. When an overall significance was observed, pairwise post-hoc tests were performed using Turkey’s test. Chi-square test was conducted to compare among groups for renal histologic score and testis histopathological findings. A p value less than 0.05 was accepted as statistically significant result.
Results
Biochemical results
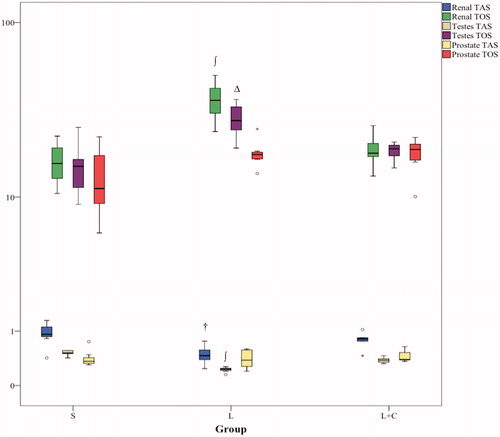
In kidney biochemical analysis, sham group had significantly higher TAS value than L group (p = 0.003, Turkey’s test). When L + C group was compared with L group, TAS value was higher (p = 0.048, Turkey’s test). Of TOS analysis, L group had higher oxidative value on kidney when compared with the other groups (p < 0.0001, Turkey’s test).
In testis, TAS level was significantly higher in sham group than the other groups (p < 0.0001, Turkey’s test), and L group had significantly diminished values than the other groups (p < 0.0001, Turkey’s test). Of TOS levels, sham group had significant lower values when compared with L group (p = 0.0001, Turkey’s test), and L group had significantly higher value when compared with L + C group (p = 0.004, Turkey’s test).
In prostate analysis, there was not any difference between groups according to biochemical TAS and TOS results. TAS and TOS findings were summarized in .
Histologic results
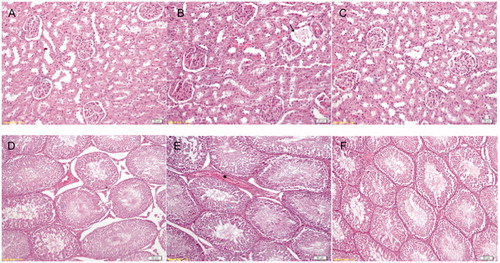
In histologic evaluation of kidney tissues, normal kidney tissue was observed in sham group (). Tubular degeneration and glomerular necrosis were observed in L group (). But these findings were not statistically significant compared to sham. CAPE administration reversed the unsignificant findings seen in L group (). According to kidney histologic score, no difference was found between three groups (p = 0.730).
Figure 2. Normal kidney histology in sham group (A). Glomerular necrosis (arrow) in laparoscopy group (B). Improved morphology in CAPE group (C). Normal germinal epithelium in sham group (D). Minimal disorganization and blood (*) in interstitial area in lap group (E). Improved epithelial structure in cape group (F).
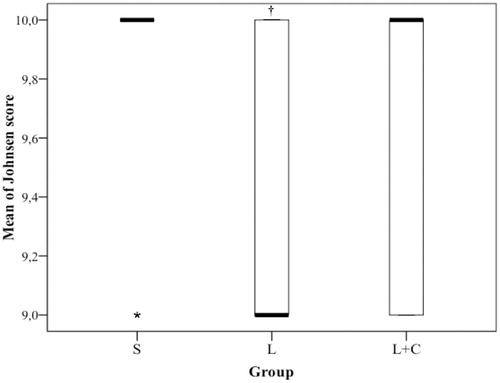
Based on Johnsen criteria, testicular tissue evaluation revealed normal spermatogenesis in S group (). According to statistical analysis of Johnsen scoring, S group showed significant difference compared to L group (p < 0.0001). There was a significant difference between L and L + C group (p = 0.046, ). There was not any difference between L + C and sham groups.
Figure 3. Testis Johnsen score results. †: p < 0.05 compared to S and L + C groups. S: Sham, L: Laparoscopy, L + C: Laparoscopy and CAPE.
In histologic evolution of testis tissue, minimal disorganization and blood in interstitial area were observed in L group (). CAPE administration improved tubular histology (). When a scoring system was used, no significant difference was recorded between groups.
Discussion
Laparoscopy is a recognized surgical approach that has great benefits for patients, significantly reduces operative time and morbidity, and results in a better postoperative recovery. However, a few physiologic complications are closely associated with gas insufflation under pressure in the abdominal cavity of mammals.Citation16 Sudden and erratic elevations of IAP can lead to various adverse events during laparoscopic abdominal surgical procedures such as subcutaneous emphysema, decreased venous return, impaired ventilation, risk of gas embolism, and even abdominal compartment syndrome,Citation17 especially in small mammals.Citation18,Citation19
Chiu et al.Citation19 performed a prospective controlled animal study on a pig model of PNP with 15 mmHg pressure. They found that superficial renal cortical blood flow reduction decreased by an average of 60% in the compressed kidney, and blood flow returned to the pre-insufflation level after the pressure was released. In animal studies, comparing CO2 to argon gas for PNP, no significant change in urine output was noted for IAPs less than 15 mmHg. For IAPs greater than or equal to 15 mmHg, a similar impairment in urine output and glomerular filtration rate was seen for both types of gas.Citation18 As a result, the major effect of IAP is I/R injury for kidneys.Citation1,Citation16,Citation18,Citation19 Our findings showed that 15 mmHg IAP generated an oxidative stress on kidney in terms of possible ischemia injury in a rat model as supported by the literature ().
Many studies have demonstrated that the major component of the adverse effects in I/R injury is not initiated by hypoxia, but rather by the return of the oxygenated blood to ischemic tissue.Citation20 Several endogenous substances, including free oxygen radicals, platelet activating factor, arachidonic acid metabolites, and bacterial endotoxins have been implicated in the pathogenesis of renal reperfusion injuries.Citation21 The amount of reactive oxygen species is under the control of antioxidant defense mechanisms.Citation22 In our study, similar to previous literature, we demonstrated that increased IAP caused oxidative stress to the kidney tissue in terms of TOS levels in L group compared to sham group. Also, sham group had higher TAS when compared with L group (). In addition, CAPE administration had protective effect for renal tissue against I/R injury induced by increased IAP.
In histological evaluation of kidney tissues, laparoscopy did not cause significant degeneration. Our histologic results were supported by Farias et al.,Citation23 Hazebroek et al.,Citation24,Citation25 and Lee et al.Citation26 who reported no significant histological changes in kidney tissue. In L group, we observed insignificant findings such as focal glomerular necrosis and signs of tubular degeneration like vacuolization, bleeding, and vascular congestion. Ozmen et al.Citation27 found similar findings of reversible hypoxic cell injury including cellular swelling, vascular congestion, and focal parenchymal bleeding. Those findings were reported to increase in 20 mmHg pressure. The significant degeneration in Ozmen’s study could be due to increased pressure.Citation27
Imamoglu et al.Citation3 initially investigated the effects of IAP on testicular blood flow (TBF) in a rat model. In their study, PNP caused a significant decrease in TBF at the 10th and 50th minutes of PNP in both 10 and 20 mmHg IAP groups. They also demonstrated that abdominal deflation after IAP of 10 and 20 mmHg for 60 minutes caused testicular free radical production. They concluded that the direct pressure effect of critically increased IAP on the testicular vessels reduced TBF, which might cause testicular hypoperfusion. IAP changes affecting the abdomen might also affect the testis due to I/R injury. Istanbulluoglu et al.Citation4 showed that IAP resulted in marked increases in inducible nitric oxide synthase (iNOS) and endothelial nitric oxide synthase (eNOS) in the testis in a pig model. However, there are limited studies which demonstrated the oxidative stress caused by IAP in testis. In our study, L group was found to have higher TOS and lower TAS levels than S group in testis tissue similar to literature (). Moreover, CAPE administration significantly inhibited oxidative stress due to increased IAP.
The effects of PNP on testicular histology were initially evaluated by Imamoglu et al.Citation3 and significant histologic degeneration was reported in 10 and 20 mmHg pressure groups for 1-hour insufflation period. Our results were partially supported by Istanbulluoglu et al.Citation4 who evaluated the effect of 20 mmHg PNP on testicular tissue in terms of apoptosis and spermatogenesis in 4 hours CO2 insufflation period. They reported marked germ cell apoptosis in study group and no significant difference in Johnsen’s score between groups. In addition, they found histologic evidences of testicular degeneration. However, they performed no quantification method for histologic degeneration. We evaluated testicular tissue according to both Johnsen criteria and a histologic quantification method. We found that laparoscopy did not make any significant changes in 1 hour with 15 mmHg CO2 insufflation with regard to histologic scoring system in contrast to Johnsen scoring system. The reason why Istanbulluoglu et al. reported marked apoptosis could be higher pressures for longer periods. In addition, S group had no significant difference compare with L + C group. It revealed that CAPE had a protective effect against toxic effect related to increased IAP on testis ().
Prostatic infarction has been reported to be significantly increased in patients with acute urinary retention.Citation28 Mentler et al.Citation29 retrospectively reviewed 111 inpatient records and found a 21.6% (n = 24) incidence of acute urinary retention after laparoscopic Nissen fundoplication. These reports suggested that blood flow and I/R played an important role in the normal functioning prostate. Saito et al.Citation5 investigated the expression of heat shock protein (HSP) 70 and its mRNAs during I/R in the rat prostate. In their study, the abdominal aorta was clamped just above its bifurcation using a small clip for 30 minute and reperfusion of the prostate was accomplished by removing the clip. They found that the expressions of HSP 70 proteins and their mRNAs were dramatically changed during I/R in the rat prostate. In our animal model, we suggested that IAP might affect the prostate vascular supply via compressing the large vessels such as abdominal aorta. Based on our findings, there was not any significant oxidative stress on prostate tissue in one hour with 15 mmHg IAP in rat model. In our opinion, higher pressures and longer periods are needed to figure out the effect of the PNP on prostate tissue. To our knowledge, this is the first study, which investigates the effect of the PNP on prostate tissue.
The limitation of our study was the lack of significant evidences in humans. There is significant difference in perfusion pressure of rat kidneys and other intraabdominal organs compared to large animals and humans. However, in patients, treated with laparoscopic partial nephrectomy, especially in an off-clamp setting, PNP was raised to 20 mmHg during excision time (usually 30–45 minutes or longer), the effect of increased IAP on kidney, testis, and the other organs remain unclear.Citation30
Conclusion
In rat model, increased IAP had an oxidative effect on kidney and testis but not on prostate. Moreover, it could affect the testicular Johnsen score. According to kidney and testis tissues’ histologic evaluation, no significant alteration was obtained in 15 mmHg pressure groups for 1-hour insufflation period. All these adverse effects of IAP on both kidney and testis could be prevented by CAPE administration. Further studies are needed to show oxidative effect of IAP against the tissues with more detailed morphological and biochemical analysis.
Declaration of interest
The authors report no conflicts of interest.
References
- Schafer M, Krahenbuhl L. Effect of laparoscopy on intra-abdominal blood flow. Surgery. 2001;129(4):385–389
- Polat C, Yilmaz S, Serteser M, Koken T, Kahraman A, Dilek ON. The effect of different intraabdominal pressures on lipid peroxidation and protein oxidation status during laparoscopic cholecystectomy. Surg Endosc. 2003;17(11):1719–1722
- Imamoglu M, Cay A, Unsal MA, et al. The effects of increased intraabdominal pressure on testicular blood flow, oxidative stress markers, and morphology. J Pediatr Surg. 2006;41(6):1118–1124
- Istanbulluoglu MO, Piskin M, Zor M, et al. The acute effects of increased intra-abdominal pressure on testicular tissue: an experimental study in pigs. Urology. 2011;77(2):510 e12–16
- Saito M, Tominaga L, Nanba E, Miyagawa I. Expression of heat shock protein 70 and its mRNAs during ischemia-reperfusion in the rat prostate. Eur J Pharmacol. 2004;487(1–3):199–203
- Ozturk G, Ginis Z, Akyol S, Erden G, Gurel A, Akyol O. The anticancer mechanism of caffeic acid phenethyl ester (CAPE): review of melanomas, lung and prostate cancers. Eur Rev Med Pharmacol Sci. 2012;16(15):2064–2068
- Parlakpinar H, Ozer MK, Ucar M, et al. Protective effects of caffeic acid phenethyl ester (CAPE) on amikacin-induced nephrotoxicity in rats. Cell Biochem Funct. 2006;24(4):363–367
- Gong P, Chen F, Liu X, Gong X, Wang J, Ma Y. Protective effect of caffeic acid phenethyl ester against cadmium-induced renal damage in mice. J Toxicol Sci. 2012;37(2):415–425
- Yilmaz S, Koken T, Tokyol C, et al. Can preconditioning reduce laparoscopy-induced tissue injury? Surg Endosc. 2003;17(5):819–824
- Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193(1):265–275
- Erel O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin Biochem. 2004;37(2):112–119
- Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 2005;38(12):1103–1111
- Tutanc M, Arica V, Yilmaz N, et al. Effects of erdosteine on cyclosporin-A-induced nephrotoxicity. Hum Exp Toxicol. 2012;31(6):565–573
- Johnsen SG. Testicular biopsy score count—a method for registration of spermatogenesis in human testis: normal values and results in 335 hypogonadal males. Hormones. 1970;1(1):2–25
- Erpek S, Bilgin MD, Dikicioglu E, Karul A. The effects of low frequency electric field in rat testis. Revue De Medecine Veterinaire. 2007;158(4):206–211
- de Barros RF, Miranda ML, de Mattos AC, et al. Kidney safety during surgical pneumoperitoneum: an experimental study in rats. Surg Endosc. 2012;26(11):3195–3200
- Bergstrom M, Swain P, Park PO. Measurements of intraperitoneal pressure and the development of a feedback control valve for regulating pressure during flexible transgastric surgery (NOTES). Gastrointest Endosc. 2007;66(1):174–178
- McDougall EM, Monk TG, Wolf JS Jr, et al. The effect of prolonged pneumoperitoneum on renal function in an animal model. J Am Coll Surg. 1996;182(4):317–328
- Chiu AW, Chang LS, Birkett DH, Babayan RK. The impact of pneumoperitoneum, pneumoretroperitoneum, and gasless laparoscopy on the systemic and renal hemodynamics. J Am Coll Surg. 1995;181(5):397–406
- Souza DG, Vieira AT, Pinho V, et al. NF-kappaB plays a major role during the systemic and local acute inflammatory response following intestinal reperfusion injury. Br J Pharmacol. 2005;145(2):246–254
- Di Paola R, Genovese T, Impellizzeri D, Ahmad A, Cuzzocrea S, Esposito E. The renal injury and inflammation caused by ischemia-reperfusion are reduced by genetic inhibition of TNF-alphaR1: a comparison with infliximab treatment. Eur J Pharmacol. 2013;700(1--3):134--146
- Nordberg J, Arner ES. Reactive oxygen species, antioxidants, and the mammalian thioredoxin system. Free Radic Biol Med. 2001;31(11):1287–1312
- Farias IE, Morais PH, Duraes Lde C, Carneiro FP, Oliveira PG, Sousa JB. Effects of carbon dioxide pneumoperitoneum on hepatic and renal morphology of rats after segmental colectomy and colonic anastomosis. Acta Cir Bras. 2011;26(4):279–284
- Hazebroek EJ, de Bruin RW, Bouvy ND, et al. Long-term impact of pneumoperitoneum used for laparoscopic donor nephrectomy on renal function and histomorphology in donor and recipient rats. Ann Surg. 2003;237(3):351–357
- Hazebroek EJ, Gommers D, Schreve MA, et al. Impact of intraoperative donor management on short-term renal function after laparoscopic donor nephrectomy. Ann Surg. 2002;236(1):127–132
- Lee BR, Cadeddu JA, Molnar-Nadasdy G, et al. Chronic effect of pneumoperitoneum on renal histology. J Endourol. 1999;13(4):279–282
- Ozmen MM, Zulfikaroglu B, Besler TH, Col C, Cinel L, Cinel I. The correlation between reactive oxygen species and histopathology of the liver, gut, and kidneys in animals with elevated intra-abdominal pressure. J Laparoendosc Adv Surg Tech A. 2009;19(3):339–343
- Strachan JR, Corbishley CM, Shearer RJ. Post-operative retention associated with acute prostatic infarction. Br J Urol. 1993;72(3):311–313
- Mentler E, Mann K, Earley A, Lucha P. High incidence of acute urinary retention associated with immediate catheter removal after laparoscopic Nissen fundoplication. Surg Endosc. 2011;25(5):1611–1616
- Bensalah K. Perioperative outcomes of off-clamp vs complete hilar control laparoscopic partial nephrectomy. BJU Int. 2013;111:E242 . doi: 10.1111/j.1464-410X.2012.11587.x