Abstract
Aim: Diabetes plays a major role in progression of renal failure. The risk-factor profile changes during the progression of chronic kidney disease (CKD) from mild/moderate to end-stage renal disease. The relationship between glycemic indices, blood pressure, body mass index (BMI) and age at diagnosis in Indians has been less investigated. We assessed association of these risk factors with CKD stages in Indian population. Methods: This study was carried out on patients (n = 162) who were diagnosed with CKD and normal control group (n = 155). For BMI, National Institutes for Health criteria were used to categorize the patients. Result: The mean age of CKD patients were significantly increased with the advancement of stage. BMI, systolic blood pressure (SBP), postprandial sugar level (PP), urea and creatinine were also significantly higher with elevated stages, whereas no differences were observed in diastolic blood pressure (DBP) and fasting blood sugar (FBS). The logistic regression study gave a significant result (p = 0.000) when we compared the group of CKD patients with established/prolonged postprandial blood sugar. It was independently associated with mild CKD [odds ratio (OR) = 5.213, 95% confidence interval (CI) = 2.06–13.21, p = 0.000], moderate CKD (OR = 7.724, 95% CI = 4.05–14.74, p = 0.000) and severe CKD (OR = 7.610, 95% CI = 4.03–14.36, p = 0.000). Conclusion: SBP and PP were the best predictors of prevalent nephropathy in this population, while DBP and FBS were found to be less effective. This may have implication for kidney disease risk stratification and protection.
Introduction
The worldwide prevalence of diabetes is expected to increase from 4% in 1995 to 5.4% by 2025.Citation1 Currently, the countries with the largest number of diabetic patients are India, China and USA. The acute and chronic complications of diabetes mellitus are major causes of hospital admissions. Asian patients have shown evidence of macro- and microvascular disease at the time of diagnosis of diabetes when compared to Europeans.Citation2 Diabetes is the most common cause of kidney failure, accounting for ∼44% of new cases.Citation3 Even when diabetes is controlled, the disease can lead to chronic kidney disease (CKD) and kidney failure. About 25 million people in the USA have diabetes and ∼180,000 people are suffering with kidney failure as a result of diabetes.Citation4 The occurrence of nephropathy in India was less (8.9% in Vellore, 5.5% in Chennai) when compared with the occurrence of 22.3% in Asian Indians in the UK.Citation5
The World Health Organization (WHO) has identified diabetes as a major health problem in Asia and, in this context, prevention of diabetes has become a high priority of health policies.Citation6,Citation7 The root of the problem is the current lifestyle causing visceral obesity; the long-term solution may be due to major changes in lifestyle.Citation8,Citation9 Besides causing premature mortality and morbidity and lowering the quality of life, it is a disease which imposes huge economic burden not only on the patients and their families but also in general on the health care system and society too.
The benefits of early diagnosis of the kidney disease extend beyond the kidney itself. Appropriate management of the co-morbid conditions reduces not only the overall and cardiovascular mortality but also improves the quality of life itself, reduces the economic burden and provides adequate time for the psychological, medical and economic preparation for renal replacement therapy.
Nevertheless, the dramatic increase of advanced diabetic nephropathy in type 2 diabetes requires additional measures targeted more specifically to the kidney. According to the recent recommendations of the American Diabetes Association and the National Kidney Foundation, two practically accessible parameters are critical for the detectionCitation10 and follow-upCitation11 of CKD in patients with diabetes: the albumin excretion rate (AER) and the glomerular filtration rate (GFR) as estimated (e-GFR) by the Cockcroft–Gault formula (CG) or the Modification of Diet in Renal Disease (MDRD) equation. Sedentary lifestyle leads toward obesity and high glucose level in blood. Obesity is indexed by body mass index (BMI), and the point of interest is in the adverse health effects of abdominal fat because of its direct relationship with visceral fat.Citation12
Elevated 2-h glucose concentration is not only an important risk factor for the development of type 2 diabetes, but also for cardiovascular disease (CVD).Citation13 Prolonged postprandial glucose (PP) excursions are risk markers of insulin resistance and dyslipidemia that collectively impact on CVD riskCitation14 that lead to CKD.
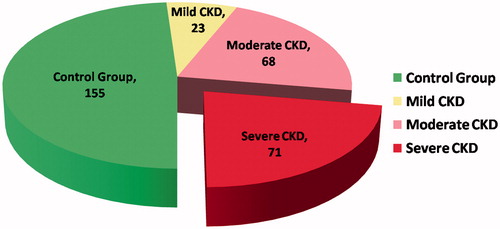
In this context, we hypothesized that higher established postprandial sugar, CVD and BMI may be increasing the severity of the kidney disease. Thus, the aim of this study was to examine the effect of the elevated postprandial glucose, CVD and BMI on the presentation and subsequent pathologic staging of kidney disease. In this study, n = 162 patients and n = 155 age-matched normal control groups were recruited, we determined isotopic GFR (i-GFR) by 51Cr-EDTA clearance (CG method) and classify the patients into three groups according to the degree of the severity.
Materials and methods
Study of population and clinical evaluation of patients
This consecutive cluster study included all patients who attended the outpatient department for kidney disease at the Department of Nephrology, Sir Sunderlal Hospital Banaras Hindu University, Varanasi, India, from January 2008. Exclusion criteria included patients <18 years of age, and patients who were mentally incapable of furnishing their own consent.
If the patient met the appropriate criteria, we visited the patient prior to treatment to explain the study and asked for patient’s participation. After receiving the formal consent from the patient, we conducted 30-min interview with the patient. Data involving presentation, diagnosis and staging were collected from the office and hospital charts, and face-to-face interview with the patient. The interview was based on pre-designed questionnaire that included questions about height and weight, age, health care and utilization, health habits, and physical activity level. This study was carried out on patients (n = 162) who were diagnosed with CKD and normal control group (n = 155) ().
Estimation of BMI
According to WHO (1998),Citation15 the BMI cutoff in Europeans for overweight (≥25 kg/m2) and obesity (≥30 kg/m2) are higher than Asian-pacific region. Steering committee (WHO Western Pacific Region, 2000;Citation16 the international association for the study of obesity and international obesity task force) recommended the cutoff for overweight (≥23 kg/m2) and obesity (≥25 kg/m2) for Asians. However, the exact classification criteria are shown in .Citation15,Citation16 BMI was measured at the time of hospital admission for treatment and the above criteria were used to categorize patients.
Table 1. Classification of BMI in adult Europids (WHO, 1998)Citation15 and Asians (WHO, 2000).Citation16
GFR estimations
Single serum creatinine measurements were performed the day before the isotopic measurement of i-GFR to calculate using CG formula.Citation17
As this equation was originally designed to estimate creatinine clearance expressed in milliliters per minute, the results were adjusted to body surface area calculated by the formula of Dubois and Dubois.Citation18
Kidney disease staging
The stages of CKD are mainly based on measured or e-GFR. There are five stages but kidney function is normal in Stage 1 and Stage 5 (end stage). In our study, we classify our patient in three groups: mild CKD (n = 60–89), moderate CKD (n = 30–59) and severe CKD (n = 15–29) on the basis of GFR [All GFR value normalized to an average surface area (size) of 1.73 m2].
Statistical analysis
Presentation and pathologic factors were compared among the CKD groups. Two-tailed tests were used at all times, and statistical significance was set a priori at p < 0.05. Statistical analyses were performed with SPSS for Windows 16.0 (Chicago, IL). All univariate analyses used Student’s t-test or χ2 tests, as appropriate. Multivariate analysis, by logistic regression, was performed to evaluate the postprandial sugar associated with the severity of CKD.
Results
The baseline characteristics of patients
The characteristics of the patients at baseline are shown in . The mean age of severe CKD (60.8 ± 9.1 years) patients was significantly higher (p < 0.000) than moderate CKD (56.7 ± 9.1 years), mild CKD (51.0 ± 10.9) and normal patients (55.2 ± 10.6). BMI, systolic blood pressure (SBP), postprandial sugar level (PP), urea and creatinine were significantly higher in severe CKD patients in comparison to other groups [(p < 0.05), whereas no differences were seen in diastolic blood pressure (DBP) and fasting blood sugar (FBS)].
Table 2. Characteristics of CKD patients at baseline and laboratory data during the follow-up period (mean with slandered deviation and 95% CI for mean).
Association of demographic and clinicopathologic presentation with disease stages
Association of demographic and clinicopathological presentation with disease stages are listed in . Patients at their latter half of life (>50 years) were significantly prone to severity in kidney disease (p < 0.01). On the basis of BMI, weight groups were found to be independently associated with disease stages. In severe CKD, 39.4% patients belong to Obese I and 12.7% with Obese II but in normal group only 29% individuals belong to Obese I and 5.2% belong to Obese II. When we compared fasting and postprandial blood sugar levels with disease stages, only postprandial blood sugar was found to be independently associated with the advancement of the disease stages (p < 0.000).
Table 3. Association between demographic presentation and pathologic factors with stages of CKD (χ2 test).
Established/prolonged postprandial blood sugar was found to be associated with advancement of the disease stage. The increased frequency of moderate and sever CKD presentation persisted on multinomial logistic regression analysis (), suggesting an independent association between mild CKD [odds ratio (OR) = 5.213, 95% confidence interval (CI) = 2.06–13.21, p = 0.000], moderate CKD (OR = 7.724, 95% CI = 4.05–14.74, p = 0.000) and severe CKD (OR = 7.610, 95% CI = 4.03–14.36, p = 0.000).
Table 4. Association of postprandial sugar with CKD stages (multinomial logistic regression analysis).
Discussion
In the 1980s, however, when past restrictions to accept type 2 diabetics for dialysis were relaxed, admission of type 2 diabetic patients for dialysis increased dramatically; we called this a “medical catastrophe of worldwide dimensions”.Citation19 In the 1990s and in the early years of the first decade after 2000, the rate of admission of type 2 diabetics for dialysis continued to increase. More recently, however, the admission rate has stabilized in the USA [United States Renal Data System (USRDS) Registry, www.usrds.org/adr.htm] as well as in Europe.Citation20
The present study investigated the risk factors associated with the development of subsequent pathological staging of kidney disease that had abnormal renal function. In this study involving 162 patients, 85.8% patients had an eGFR <59 mL/min/1.73 m2. However, in the MDRD study, as many as 19% of patients with GFR between 25 and 55 mL/min/1.73 m2 experienced improvement or stabilization of their renal function during the 2-year study period.Citation21 A community-based study of CKD among type 2 diabetic Chinese patients in Taiwan showed that the prevalence of CKD was 38%.Citation22 However, Lu et al.Citation23 reported the prevalence of CKD as high as 63.9% in downtown Shanghai, China. The marked variation in the prevalence of CKD might be due to the difference in study cohort characteristics.
Hypertension is a well-recognized risk factor for diabetic patients to develop advancement in CKD stages. However, in the present study, the association with SBP was stronger than those with other BP indices (DBP) based on likelihood ratio comparison. Globally, the risks of kidney diseases afforded by BP have been investigated for prevalent, incident kidney diseases, and for the progression of established disease. The focus has often been on people with non-optimal BPs. Risks have also been assessed across the persistence of BP measurements including in people with diabetes. Comparisons have often examined the issues of whether ambulatory, office, day or night time BPs were similar determinants of nephropathies.Citation24–27 Few studies have directly compared different BP variables from the same measurements for the prediction of nephropathy, including in people with diabetes. These studies have generally emphasized the importance of SBP over DBP in promoting the development and progression of diabetic nephropathy.Citation28 In the Ohasama Study,Citation24 SBP was a significant predictor of microalbuminuria while pulse pressure was not. In a cohort of London individuals with CKD at baseline, pulse pressure was stronger than systolic BP in predicting further decline in kidney function over a mean follow-up duration of 172 days.Citation29
In the present study higher age group, obesity and elevated postprandial glucose affected the patients, although these parameters were higher among subjects with advanced stage of CKD. First, higher postprandial glucose concentrations in the elderly age result from lower rates of glucose disappearance because postprandial suppression of endogenous glucose production and systemic appearance of ingested glucose do not differ between the groups. Postprandial hyperglycemia differs from fasting hyperglycemia in pathophysiology and the risk of adverse outcomes. Postprandial hyperglycemia results mainly from a moderate to severe decrease in muscle insulin sensitivity and late-phase insulin secretary response to oral glucose; whereas fasting hyperglycemia results mainly from a defect in hepatic insulin sensitivity and first-phase insulin response.Citation30 Levitan et al.Citation31 reveled through a meta-analysis of 38 prospective studies, which demonstrated that non-diabetic postprandial hyperglycemia significantly raises the likelihood of cardiovascular events or even death and that the relationship remains after cardiovascular risk factors have been adjusted for. The underlying pathobiologic changes linking elevated postprandial glucose and cardiovascular diseases consist mainly of elevated oxidative stress and endothelial dysfunction, leading to atherothrombotic propensities of elevated postprandial glucose, such as oxidation of LDL cholesterol, vasoconstriction and thrombogenicity.Citation32 Moreover, interventions targeting elevated postprandial glucose are of clinical significance for optimizing comprehensive glycemic control in individuals with diabetes and with impaired glucose regulation to lower the risk of adverse outcomes.Citation33,Citation34
Thus, this study with ample evidence to support the fact that SBP, obesity and postprandial hyperglycemia is linked to increased risk of CKD and poorer subsequent survival.
Conclusion
In conclusion, although both glycemic indices are significant predictors of prevalent CKD, the present study suggests that postprandial hyperglycemia is the more effective predictor, and combination of elevated SBP adds influence to the advancement of disease stages. These findings largely support applicability in this population of current recommendations for preventing the onset and slowing the progression of CKD. Once CKD is diagnosed, it is destined to progress to end-stage renal disease. Hence during early stages, aggressive BP control and decreasing postprandial glucose with the use of established drugs would be much effective in retarding progression to end-stage renal disease.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article. There is neither medical writing nor editorial assistance was used for the preparation of this article. The authors declare that all of them have made substantial contribution toward the writing of this article.
This study was supported by departmental contingency for research and research grant “Dr. D. S. Kothari Post Doctoral Fellowship” from University Grants Commission, India, availed through Banaras Hindu University [No. F.4/2006(BSR)/13-581/2012(BSR].
Acknowledgments
We thank all medical and nursing staffs of Nephrology and Diabetes Care for the design and conduct of the study and team members of Department of Nephrology and Centre for Genomic Disorder, Banaras Hindu University of India for the guidance and comments.
References
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995--2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–1431
- Chowdhury TA, Lasker SS. Complications and cardiovascular risk factors in South Asians and Europeans with early-onset type 2 diabetes. QJM. 2002;95:241–246
- United States Renal Data System. USRDS 2007 Annual Data Report. Bethesda, MD: National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, US Department of Health and Human Services; 2007
- National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics, 2007. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2008
- Ramachandran A. Epidemiology of diabetes in India—three decades of research. J Assoc Physicians India. 2005;53:34–38
- Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414:782–787
- Geneau R, Stuckler D, Stachenko S, et al. Raising the priority of preventing chronic diseases: a political process. Lancet. 2010;376:1689–1698
- Tuomilehto J, Lindström J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350
- Gong Q, Gregg EW, Wang J, et al. Long-term effects of a randomised trial of a 6-year lifestyle intervention in impaired glucose tolerance on diabetes-related microvascular complications: the China Da Qing Diabetes Prevention Outcome Study. Diabetologia. 2011;54:300–307
- Kramer H, Molitch ME. Screening for kidney disease in adults with diabetes. Diabetes Care. 2005;28:1813–1816
- Levey AS, Coresh J, Balk E, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification and stratification. Ann Intern Med. 2003;139:137–147
- Janssen I, Heymsfield SB, Allison DB, et al. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous and visceral fat. Am J Clin Nutr. 2002;75:683–688
- The DECODE Study Group, European Diabetes Epidemiology Group. Is the current definition for diabetes relevant to mortality risk from all causes and cardiovascular and non-cardiovascular diseases? Diabetes Care. 2003;26:688–696
- Tushuizen ME, Diamant M, Heine RJ. Postprandial dysmetabolism and cardiovascular disease in type 2 diabetes. Postgrad Med. 2005;81:1–6
- WHO/IASO/IOTF. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Health Communications Australia Pty Limited on behalf of the Steering Committee (WHO Western Pacific region), Australia: Melbourne; 2000
- Singh AK, Pandey A, Tewari M, et al. Obesity augmented breast cancer risk: a potential risk factor for Indian women. J Surg Oncol. 2011;103(3):217–222
- Cockcroft DW, Gault HM. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41
- DuBois D, DuBois EF. A formula to estimate the approximate surface area if height and weight are known. Ann Intern Med. 1916;17:863–871
- Ritz E, Rychlík I, Locatelli F, Halimi S. End-stage renal failure in type 2 diabetes: a medical catastrophe of worldwide dimensions. Am J Kidney Dis. 1999;34:795–808
- Stel VS, Tomson C, Ansell D, et al. Level of renal function in patients starting dialysis: an ERA-EDTA Registry Study. Nephrol Dial Transplant. 2010;25:3315–3325
- Hunsicker LG, Adler S, Caggiula A, et al. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int. 1997;51:1908–1919
- Lin CH, Yang WC, Tsai ST, Tung TH, Chou P. A community-based study of chronic kidney disease among type 2 diabetics in Kinmen, Taiwan. Diabetes Res Clin Pract. 2007;75:306–312
- Lu B, Song X, Dong X, et al. High prevalence of chronic kidney disease in population-based patients diagnosed with type 2 diabetes in downtown Shanghai. J Diabetes Complications. 2008;22:96–103
- Ishikawa T, Hashimoto J, Morito RH, et al. Association of microalbuminuria with brachial-ankle pulse wave velocity: the Ohasama Study. Am J Hypertens. 2008;21:413–418
- Palmas W, Pickering T, Teresi J, et al. Nocturnal blood pressure elevation predicts progression of albuminuria in elderly people with type 2 diabetes. J Clin Hypertens (Greenwich). 2008;10:12–20
- Palmas W, Moran A, Pickering T, et al. Ambulatory pulse pressure and progression of urinary albumin excretion in older patients with type 2 diabetes mellitus. Hypertension. 2006;48:301–308
- Tanaka M, Babazono T, Takeda M, Iwamoto Y. Pulse pressure and chronic kidney disease in patients with type 2 diabetes. Hypertens Res. 2006;29:345–352
- Knudsen ST, Andersen NH, Mogensen CE. Ambulatory pulse pressure and progression of albuminuria in type 2 diabetes: evidence provided, new questions emerge. Hypertension. 2006;48:207–208
- Arulkumaran N, Diwakar R, Tahir Z, Mohamed M, Kaski JC, Banerjee D. Pulse pressure and progression of chronic kidney disease. J Nephrol. 2010;23:189–193
- Nathan DM, Davidson MB, DeFronzo RA, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30:753–759
- Levitan EB, Song Y, Ford ES, Liu S. Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med. 2004;164:2147–2155
- Ceriello A. Impaired glucose tolerance and cardiovascular disease: the possible role of post-prandial hyperglycemia. Am Heart J. 2004;147:803–807
- Ceriello A, Colagiuri S. International Diabetes Federation guideline for management of postmeal glucose: a review of recommendations. Diabet Med. 2008;25:1151–1156
- Kebapci N, Uslu S, Ozcelik E. Metabolic syndrome is a risk factor for the development of chronic renal disease. Ren Fail. 2013;35(4):460–465