Abstract
Background: Left ventricular hypertrophy is the most common structural cardiac alteration in chronic dialysis patients. The aim of this study was to determine the possible association of endotelin-1 (ET-1) and nitric oxide (NO) with parameters of echocardiography in order to assess their participation in left ventricular (LV) remodeling in patients on peritoneal dialysis (PD). Methods: This prospective longitudinal study included 40 PD patients. Serum levels of ET-1 and NO baseline and after 12 months of PD treatment were measured and compared with echocardiography parameters done at the same time of PD treatment. Linear regression analysis was used to detect independent correlations of variables. Results: Mean ET-1 serum concentration decreased significantly after 12 months of PD treatment compared to baseline values (p < 0.01). NO serum concentration increased significantly 12 months after treatment compared to baseline values (p < 0.01). Left ventricular hypertrophy (LVH) was observed in 72.5% of patients at baseline with significant reduction in LV mass index after 12 months of PD treatment (p < 0.001). On linear regression analysis serum concentration of ET-1 was independent predictors of LV mass index, as well as NO at the end of observed period. Conclusions: According to our data ET-1 and NO are independently related to the process of left ventricular remodeling in PD patients
Introduction
Left ventricular hypertrophy (LVH) is a major cardiovascular risk factor in end stage renal disease (ESRD) with a prevalence of 75%, and also a predictor of cardiac death in peritoneal dialysis patients.Citation1 The morphological changes of the CV system occur mainly in response to long-lasting pressure and volume overload, as well as interaction between these mechanical stimuli, locally generated growth factors and vasoactive substances.Citation2
Endothelin (ET) is a potential vasoconstrictor occurring in three isoforms, although it dominantly occurs in serum in the form of ET-1.Citation3 In the conditions of endogenic homeostasis this vasoconstrictor has paracrine/autocrine action, whereas in several pathologic conditions it can be considered as circulating “hormone”.Citation4 It has been established that the level of endothelin in serum is increased in patients with acute myocardial infarction, atherosclerosis, congestive heart failure, liver cirrhosis and kidney disease.Citation5 Recent research show that endothelin acts as mitogenic stimulator of cardiac hypertrophy and proliferation of vascular smooth muscles.Citation4 The concentration of serum ET-1 is especially increased in dialysis patients. However, the mechanism and importance of this increase in patients on peritoneal dialysis (PD) is not completely clarified.Citation6 Research by Löwbeer et al.Citation7 suggests that in the state of heart failure in PD patients ET-1 is released from the damaged myocardium, which then contributes to calcium overload and the development of LVH. Because of its properties, strong vasoconstrictor action and influence on intracellular calcium, it is considered that ET-1 plays an important role in these patients in pathogenesis of hypertension, coronary vasospasm and heart failure.
Nitric oxide (NO) is produced by many cells in the body, but the production of NO in vascular endothelium is especially important for the regulation of blood circulation. The effects of NO on blood vessels include direct and indirect vasodilatation through inhibition of vasoconstrictor, antithrombotic, anti-inflammatory and antiproliferative effect in terms of inhibition of hyperplasia of smooth muscles.Citation6 Due to these important and multiple functions of NO, the reduction of its production or the reduction of its bioavailability may result in the occurrence of vasoconstriction.Citation8 NO has a protective role for the cardiovascular system because it not only modulates arterial compliance and peripheral vascular resistance, but also ensues decreased atherosclerosis.
There are many studies that have investigated the effect of NO in patients with ESRD, but only few in patients on peritoneal dialysis. According to Baylis et al.,Citation9 the measurement of NO level in ESRD patients treated with PD showed that the overall production of NO in these patients was low. It was established that in ESRD patients, one part of the produced NO is excreted in urine, whereas in PD patients’ urine elimination of NO was reduced. A question arises about the changes of concentration of serum ET-1 and NO in PD patients which appears during chronic treatment of PD and its relation towards cardiac system.
The aim of this study was to analyze the serum concentration of ET-1 and NO in PD patients at the time of start of dialysis treatment and after 12 months of treatment, and to evaluate the relation of these vasoactive substances with echocardiographic parameters of left ventricle during the treatment with PD.
Subjects and methods
This prospective longitudinal study included 40 ESRD patients who were observed for 1 year after the commencement of peritoneal dialysis treatment. The patients with the verified diagnosis of heart valve diseases and cerebral vascular diseases were excluded from the study, based on the criteria of the American Heart Association. All examined patients underwent four to five dialysis changes with 2 L of dialysis solution, with the weekly clearance Kt/V urea 1.9 ± 0.85. At the moment of commencement of observation, all observed patients were without clinical manifestation of heart failure. The baseline laboratory assessment included measurement of brain-natriuretic peptide (BNP) and total homocysteine (tHcy) as well as serum ET-1 and NO concentration.
In all patients echocardiographic parameters were evaluated at the very beginning of dialysis treatment and after 1 year. In all patients antihypertensive therapy, as well as therapy that can influence the values of monitored laboratory parameters were excluded 24 h before taking blood samples for determination of concentration of ET-1 and NO. The study was conducted 2 h after an early morning dialysis change. All records of patients were protected, whereas the study was conducted with the approval of local Ethics Committee and the respect for the rules of ethic principles in medical research. All patients were given their informative consent for the participation in the study.
Laboratory measurements
The measurement of serum concentration of ET-1 (pg/mL) was done by the ELISA method (Enzyme immunoassay for the quantitative determination of human endothelin (1–21) in serum, kit Biomedica Medizinprodukte GmbH & Co KG, Wien).
For the determination of concentration of NO in the serum, R&D System Total Nitric Oxide kit was utilized, while the concentration of NO was expressed in μmol/L. Blood samples for the determination of concentration of NO and ET-1 were analyzed at the Institute for Biochemistry of the Clinical Hospital Sestre milosrdnice in Zagreb, Croatia.
Echocardiographic assessment
Echocardiographic assessment was conducted by “Toshiba 270 SSA” device, equipped with the 3.75 MHz frequency sector sonde. All patients were examined with the method of conventional M-mode and two-dimensional echocardiography. The measurement performed by two cardiologists, who were not acquainted with the clinical status of the patients, according to the recommendations of the American Society of Echocardiography. The left ventricular mass was calculated according to the formula of Penn Convention,Citation10 while the left ventricular mass index (LVMI) was calculated with the division of the left ventricular mass with the body surface area. LVH is defined as the LVMI >131 g/m2 for males and >100 g/m2 for females. The systolic function of the left ventricle (LV) was assessed by the measurement of ejection fraction (EF). The systolic weakness of LV is defined as EF <50%. The diastolic function of LV is assessed by determination of the maximum velocity of the early (E) and late (A) phase of ventricular filling and the calculation of the E/A ratio. The diastolic dysfunction of LV is defined as E/A ≤1.
Statistical analysis
All statistical calculations were performed with the SPSS 16 software (version 16.0, SPSS Inc, Chicago, IL). Each value was expressed as the mean ± SD or as median and interquartile range where appropriate. Significant changes in the variables from baseline to 12 months after treatment were tested by paired t test for the variables that followed normal distribution or by the Wilcoxon signed-rank test for the variables that had skewed distribution. The difference between two groups was analyzed by the Mann–Whitney test. Univariate correlation coefficients were determined by the Pearson or Spearman analysis. A multiple regression analysis was applied to examine the relationship between left ventricular remodelling parameters and a set of clinical and laboratory parameters. Since ET-1, NO, CRP, BNP, tHcy and age were non-normally distributed in this study, we normalized these data by log transformation before entering a stepwise multiple regression. The significant independent variables were ordered according to their standardized effect, defined as regression coefficient/standard error of the regression (β). p Values <0.05 were considered statistically significant.
Results
In our study 70% of patients had elevated blood pressure before started with peritoneal dialysis treatment compared to 42.5% of CAPD patients after 12 months of dialysis treatment. Mean serum ET-1 concentration decreased significantly after 12 months on PD treatment (6.73 ± 7.95 pg/mL) compared to baseline (7.74 ± 8.43 pg/mL) values (p < 0.01) (). Serum NO concentration increased significantly 12 months after treatment (53.26 ± 30.56 µmol/L) compared to baseline values (46.02 ± 29.73 µmol/L) (p < 0.01).
Table 1. Characteristics of the PD patients at baseline and after 12 months.
Table 2. Cardiac parameters in PD patients at baseline and after 12 months.
Table 3. Correlation of cardiac parameters, ET-1 and NO in 1-year follow-up.
Discussion
In our study we monitored the concentration of serum endothelin-1 and NO, along with echosonographic changes on LV, over a period of 1 year on PD treatment, as well as its influence on left ventricular remodelling in PD population ( and ). Verified elevated values of ET-1 concentration in the serum of uremic patients before the commencement of dialysis treatment may be a consequence of reduced elimination of ET-1 from circulation due to ESRD and the damage of vascular endothelial cells. It is established that hyperproduction of ET-1 in dialysis patients, accompanied by the increased concentration of circulating ET-1, may lead to the development of endothelial dysfunction,Citation11 which increases the risk of cardiovascular morbidity and mortality in patients with chronic kidney disease.Citation12
Figure 1. ET-1 serum concentration in patients with and without LVH in 12-month follow-up. LVH, left ventricular hypertrophy; w/o LVH, without left ventricular hypertrophy. The solid horizontal lines denote the median value, the box represents the 25% and 75% interquartile ranges and the whiskers represent minimum and maximum values.
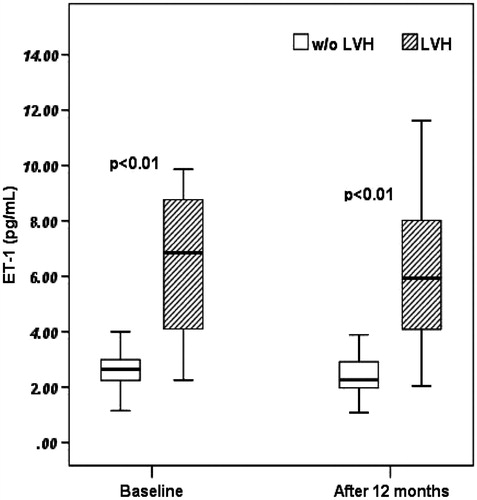
Figure 2. NO serum levels in patients with and without LVH in 12-month follow-up. LVH, left ventricular hypertrophy; w/o LVH, without left ventricular hypertrophy. The solid horizontal lines denote the median value, the box represents the 25% and 75% interquartile ranges and the whiskers represent minimum and maximum values.
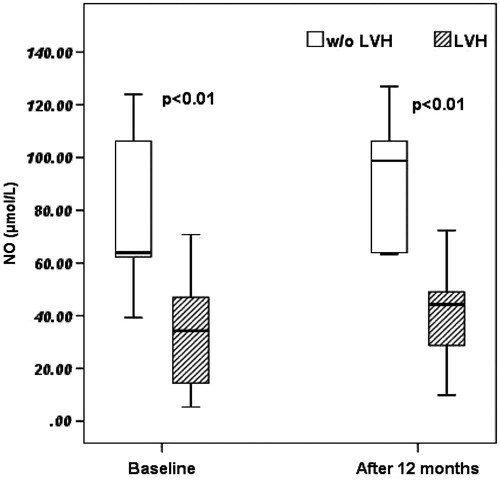
Figure 3. Scatter chart showing LV mass index (x-axis) versus ET-1 (y-axis). Linear line of best fit is shown. p < 0.001, r = 0.72.
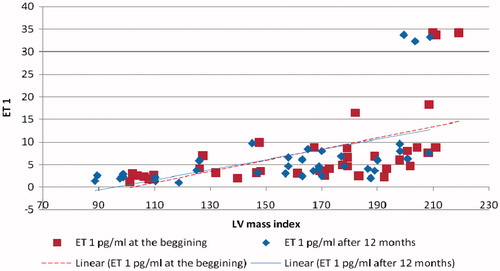
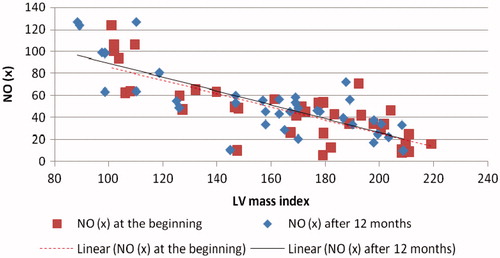
Figure 4. Scatter chart showing LV mass index (x-axis) versus NO (y-axis). Linear line of best fit is shown. p < 0.001, r = −0.82. On linear regression analysis independent predictors of baseline EF and E/A ratio were ET-1, DM type 2 and Hgb (R2 = 0.71 and R2 = 0.59, p < 0.01 respectively). ET-1, hypertension and DM type 2 were independently associated with LV mass index (R2 = 0.68; p < 0.01). After 12 months on PD treatment serum NO and DM type 2 were independently associated with LV mass index (R2 = 0.67) and E/A ratio (R2 = 0.30), while serum NO, BNP and Hgb were related with EF (R2 = 0.7, p < 0.001).
LVH was observed in 72.5% of patients at baseline with significant reduction in LV mass index and significant improvement of systolic and diastolic LV function after 12 months of treatment. LV mass and LV mass index are modifiable factors, and their reduction decreases cardiovascular risk, especially in dialysis population.Citation13 Zoccali et al.Citation14 confirmed that ∼40% of all mortality cases of patients on dialysis is caused by cardiovascular diseases. LVH, systolic and diastolic LV dysfunction is identified as independent predictors of cardiovascular morbidity and survival. Important indicators of LVMI changes are hemodynamic and non-hemodynamic factors. In PD patients the most prominent hemodynamic parameters are hypertension of high prevalence, volume overload and anaemia.Citation15
In linear regression analysis in our study independent predictors of LV mass index were ET-1, hypertension and DM type 2, while independent predictors of LV systolic and diastolic function were ET-1, DM type 2 and hemoglobin. Non-hemodynamic factors that could affect LVMI in PD patients include the retention of molecules in circulation, such as ET-1, angiotensin II and insulin-like growth factor.Citation16 The concentration of these trophic factors in circulation is increased in renal failure.Citation17
The results of our study suggest that at the very beginning of dialysis treatment patients have higher LVMI values compared to values observed after 1 year of dialysis treatment, along with the decrease in ET-1 serum concentration as a potent vasoconstrictor and the increase in NO level as vasodilatator. Such changes are accompanied by significantly positive correlation between ET-1 serum concentration and LVMI, and also by significantly negative correlation of LVMI with the NO serum concentration level. These results indicate that influence of these vasoactive substances in the process of LV remodelling in PD patients.
Demuth et al.Citation18 have demonstrated a significant positive correlation between elevated plasma ET concentration and an increased LV mass in ESRD patients. Zocalli et al. reported in a pioneer study that there was a significant correlation between serum asymmetric dimethyl arginine (ADMA) as an endogenous inhibitor of NO synthase enzyme and LV mass index in dialysis patients. That study was the first point to a possible role of reduced serum NO in the development of LVH in patients undergoing renal replacement therapy.Citation19
In conclusion, intensive monitoring of hemodynamic and non-hemodynamic risk factors of cardiovascular diseases such as ET-1 and NO in PD patients is necessary. Our study confirmed significance relationship between the remodelling of left ventricular hypertrophy and ET-1 and NO serum concentration level in PD patients during period of 12-month follow-up. Overall, these findings suggest a potential role of these biomarkers into development of LVH in uremic patients and possible regression of unwanted left ventricle changes in PD patients. Therefore, we would suggest a multicentric study with larger number of PD patients and a longer time of follow-up for the evaluation of the findings.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Mejía-Rodríguez O, Alvarez-Aguilar C, Vega-Gómez EH, Belio-Caro F, Vargas-Espinosa MJ, Paniagua-Sierra RJ. Bromocriptine induces regression of left ventricular hypertrophy in peritoneal dialysis patients. Proc West Pharmacol Soc. 2005;48:122–125
- Li H, Wang S. Organic nitrates favor regression of left ventricular hypertrophy in hypertensive patients on chronic peritoneal dialysis. Int J Mol Sci. 2013;14:1069–1079
- Quaschning T, Kocak S, Bauer C, Neumayer HH, Galle J, Hocher B. Increase in nitric oxide bioavailability improves endothelial function in endothelin-1 transgenic mice. Nephrol Dial Transplant. 2003;18:479–483
- Dhaun N, Goddard J, Webb JD. The endothelin system and its antagonism in chronic kidney disease. JASN. 2006;17(4):943–955
- Agapitov VA, Haynes GW. Role of endothelin in cardiovascular disease. Rev Bras Hipertens. 2003;10:87–105
- Rabelink TJ, de Boer HC, van Zonneveld J. Endothelial activation and circulating markers of endotelial activation in kidney disease. Nat Rev Nephrol. 2010;6(6):404–414
- Löwbeer C, Ottosson-Seeberger A, Gustafsson AS, Norrman R, Hulting J, Gutierrez A. Increased cardiac troponin T and endothelin-1 concentrations in dialysis patients may indicate heart disease. Nephrol Dial Transplant. 1999;14(8):1948–1955
- Jacobi J, Tsao SP. Asymmetrical dimethylarginine in renal disease: limits of variation or variation limits? Am J Nephrol. 2008;28(2):224–237
- Baylis C. Nitric oxide deficiency in chronic kidney disease. AJP-Renal Physiol. 2008;294(1):F1–F9
- Devereux R, Alonso D, Lutas E, Gottlieb G, Compo E, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–458
- Liu H, Peng Y, Liu F, et al. Correlation between endothelin-1 and atherosclerosis in chronic hemodialysis patinets. J Nephrol. 2010;23(5):593–602
- Ochodnicky P, Vettoretti S, Henning RH, Buikema H, Van Dokkum RP, de Zeeuw D. Endothelial dysfunction in chronic kidney disease: determinant of susceptibility to end-organ damage and therapeutic response. J Nephrol. 2006;19(3):246–258
- de Bie KM, Ajmone Marsan N, Gaasbeek A, et al. Left ventricular diastolic dysfunction in dialysis patients assessed by novel speckle tracking strain rate analysis: prevalence and determinants. Int J Nephrol. 2012;2012:963504
- Zoccali C, Benedetto FA, Mallamaci F, et al. Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventricular hypertrophy progression. Kidney Int. 2004;65(4):1492–1498
- London GM. Left ventricular alterations and end-stage renal disease. Nephrol Dial Transplant. 2002;17(1):29–36
- Glassock RJ, Pecoits-Filho R, Barberato SH. Left ventricular mass in chronic kidney disease and ESRD. Clin J Am Soc Nephrol. 2009;4(1):S79–S91
- Vanholder R, De Smet R, Glorieux G, et al. Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 2003;63(5):1934–1943
- Demuth K, Blacher J, Guerin AP, et al. Endothelin and cardiovascular remodelling in end stage renal disease. Nephrol Dial Transplant. 1998;13:375–383
- Zoccali C, Mallamaci F, Maas R, et al. Left ventricular hypertrophy, cardiac remodeling and asymmetric dimethylarginine (ADMA) in hemodialysis patients. Kidney Int. 2002;62:339–345
