Abstract
Acute myocardial infarction (AMI) in dialysis patients is associated with high mortality rate. Large randomized controlled trials documenting the benefits of revascularization in the general population have excluded chronic dialysis patients. Few observational data suggest that revascularization may provide a survival benefit compared with medical treatment alone also in these patients. We report a case of a dialysis patient who survived five documented AMIs, underwent five coronary angiographies in 11 years, had several episodes of angina pectoris and underwent percutaneous transluminal coronary angioplasty (PTCA) with stenting and heart surgery for coronary bypassing. It represents a highly unusual therapeutic approach and might contribute to support also in dialysis patients the use of revascularization to improve survival.
Introduction
Acute myocardial infarction (AMI) in dialysis patients is a catastrophic event associated with high mortality rate.Citation1–3 While the large randomized controlled trials (RCTs) that have documented the benefits of revascularization in the general population have generally excluded patients on maintenance dialysis, few observational data suggest that in these patients revascularization may provide a survival benefit compared with medical treatment alone.Citation4
We report a case of a dialysis patient who survived five documented AMI, underwent five coronary angiographies in 11 years, had several episodes of angina pectoris and underwent percutaneous transluminal coronary angioplasty (PTCA) with stenting and heart surgery for coronary bypassing. This case represents a highly unusual outcome and unusual therapeutic approach for such patients, which might contribute to support the use of revascularization procedure to improve survival also in dialysis patients.
Case report
A patient, immigrant from Bangladesh, with diabetic nephropathy on insulin treatment and diabetic foot, first came to our nephrology clinic in 2001 at the age of 56. He was a heavy smoker and had duodenal ulcer as comorbidities.
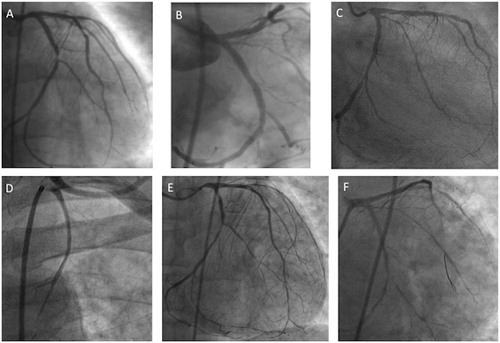
In 2001, he experienced a non-ST-elevation myocardial infarction (NSTEMI), coronary angiography showed a severe, sub-occlusive lesion of dominant left circumflex coronary artery (LCX), and a mild-to-moderate stenosis of left anterior descending artery (LAD) (, panel A). Systolic function of left ventricle was normal. A bare metal stent was successfully implanted on LCX (, panel B) and as medical treatment, ramipril 5 mg, metoprolol 100 mg, acetylsalicylic acid 100 mg, and simvastatin 40 mg were prescribed.
Figure 1. Panel A: coronary angiogram showing mild stenosis of mid-LAD and severe stenosis at proximal segment of dominant LCX; Panel B: angiographic image after bare metal stent implantation on proximal LCX; Panel C: coronary angiogram showing severe stenosis at the ostium of LM, multiple stenosis of middle LAD, first diagonal branches, and in-stent restenosis of LCX involving obtuse marginal branch. Panel D: angiogram showing occlusion of both by-pass grafts; Panel E: native coronary artery angiogram showing severe stenosis of ostial LM, moderate stenosis of mid-LAD, with diffuse disease of diagonal and septal branches; moderate in-stent restenosis on proximal LCX and severe; Panel F: angiographic image after bare metal stent implantation on LM. LAD, left anterior descending artery; LCX, left circumflex artery; LM, left main; NSTEMI, non-ST elevation myocardial infarction; PL, posterolateral branch.
In 2003, the patient started three times a week chronic 210–240 min, low-flux bicarbonate dialysis, with ultrapure dialysate, using a polysulphone dialyzer 1.8 m2.
In 2008, after a new NSTEMI of anterolateral myocardial wall, coronary angiography showed significant progression of coronary artery disease: tight lesion at the ostium of left main artery determining 90% stenosis, multiple significant stenosis (>70%) at middle segment of LAD and first diagonal branch as well as tight stenosis of proximal LCX (in-stent restenosis) and obtuse marginal (OM) branch (, panel C). Due to the presence of diffuse coronary disease, the patient underwent coronary artery by-pass, with implantation of left internal mammary artery on LAD, and saphenous vein graft for the postero-lateral branch of LCX. In the same year due to an episode of acute heart failure with atrial fibrillation, the patient was treated by non-invasive respiratory support, diuretics, anti-arrhythmic drugs, and warfarin, which was discontinued after 3 months when he regained sinus rhythm and double antiplatelet treatment with acetylsalicylic acid and clopidogrel, was prescribed.
On November 2011 during a hemodialysis session, he had another NSTEMI. Coronary angiogram showed the occlusion of both grafts (, panel D), severe stenosis (80%) of ostial left main (LM), moderate stenosis of mid-LAD, with diffuse disease of diagonal and septal branches, moderate stenosis of Ramus, moderate in-stent restenosis on proximal LCX, and severe stenosis of distal LCX at bifurcation with PL branch (, panel E). Bare metal stent (Vision 4.0 × 8 mm, Abbott Vascular) was then successfully implanted on LM (, panel F).
On September 2012, notwithstanding the full antiplatelet, antiatherosclerotic, and CV protective medical treatment, the patient experienced a new NSTEMI of lateral myocardial wall and coronary angiography documented focal in-stent restenosis of LM, a moderate stenosis of mid LAD, diffuse disease of diagonal branches, tight stenosis of ostial LCX, and a long lesion in distal LCX beyond the distal edge of the previous implanted stent (, panel A). Direct bare metal stents of proximal (ML Vision 2.5 × 12 mm) and distal (ML Vision 2.5 × 28 mm) LCX were successfully implanted as well as in-stent re-PTCA of LM (, panel B). Left ventricular angiography showed mild dysfunction of left ventricle with akinesis of antero-lateral and diaphragmatic wall.
Figure 2. Panel A: coronary angiogram showing focal in-stent restenosis of LM, tight stenosis of ostial LCX, and a long lesion in distal LCX beyond the distal edge of the previous implanted stent. Panel B: angiographic image after multiple bare metal stent implantations on proximal and distal LCX, and in-stent re-PTCA of LM. Panel C: coronary angiogram showing severe and diffuse in-stent restenosis of LCX involving the ostium of OM branch; Panel D: angiographic image after re-PTCA of LCX.
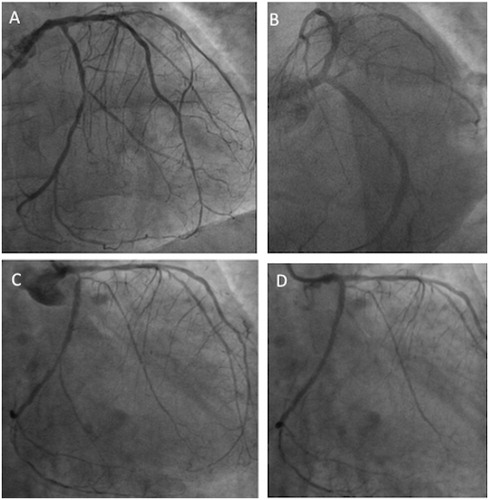
On December 2012, the patient experienced angina and during paroxysmal atrial fibrillation with chest pain and ST-segment shift on anterolateral leads a NSTEMI was documented. Two months later he was admitted in the cardiac emergency unit due to episodes of recurrent ischemia and coronary angiography showed severe and diffuse in-stent restenosis of LCX involving the ostium of OM side branches (, panel C); in-stent re-PTCA was successfully performed (, panel D).
Currently, after almost a year since the last episode of angina, the patient did not experience any other chest pain episode or coronary complications and continues his chronic dialysis.
Discussion
AMI in dialysis patients is a catastrophic event associated with very poor medium-long-term survival.Citation1–4 One year death rate of 59% and 2 years death rate of 73% were reported in US dialysis patients hospitalized for AMI from 1977 through 1995.Citation3 The 2 years death rate reported for dialysis patients initiating renal replacement therapy from 1995 through 1999 who subsequently experienced AMI in the modern era of reperfusion therapy was still 73%.Citation3
The case we presented reports survival to five AMIs, really unusual for patients on chronic dialysis while instead may be the case for the general population. At the present, it remains unsolved whether intervention, either by percutaneous or by coronary artery bypass grafting (CABG), improves outcome in dialysis patients with proven CAD. The large RCTs that have documented the benefits of revascularization in the general population, generally excluded patients with renal disease, particularly those on maintenance dialysis and their conclusions cannot be extrapolated to the dialysis population. Few observational data, however, suggest that revascularization may provide a benefit in terms of survival as compared with medical treatment alone. One-year survival rates in dialysis patients experiencing an AMI treated with medical therapy alone, PTCA, or CABG were 45%, 54%, and 69%, respectively.Citation4 Patients on dialysis may not tolerate aggressive medical therapy for CAD due to the hemodynamic effects of beta-blockers, nitrates, and calcium channel blockers, which may hamper the achievement of target dry weight in these patients, thus the optimal medical therapy for CAD in the general population may not be for dialysis patients.Citation5,Citation6
Our patient seems to be a living example of what a medical textbook reports regarding all the coronary morbidities and cardiac comorbidities for a CKD/dialysis patient. He had the best therapeutic options both medical and interventional to be a quite unique reference of the victory of a dialysis patient over a long-lasting fight against his coronaries and his case may contribute to support the use of revascularization procedures to improve survival also in dialysis patients.
Declaration of interest
The authors report no conflicts of interest.
References
- Luke RG. Chronic renal failure -- a vasculopathic state. N Engl J Med. 1998;339:841–843
- Williams BA, Dvorak DL, Miller WL, Murphy JG, Kopecky SL, Jaffe AS. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002;137:563–570
- Herzog CA, Littrell K, Arko C, et al. Clinical characteristics of dialysis patients with acute myocardial infarction in the United States: a collaborative project of the United States Renal Data System and the National Registry of Myocardial Infarction. Circulation. 2007;116:1465–1472
- Chertow GM, Normand SL, Silva LR, et al. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35:1044–1051
- Agarwal R, Sinha AD. Cardiovascular protection with antihypertensive drugs in dialysis patients: systematic review and meta-analysis. Hypertension. 2009;53:860–866
- Kaisar MO, Isbel NM, Johnson DW. Recent clinical trials of pharmacologic cardiovascular interventions in patients with chronic kidney disease. Rev Recent Clin Trials. 2008;3:79–88
