Abstract
Although the epidemiology and the impact of Acute Kidney Injury on outcomes are well-known in the Western literature, good data is lacking from India. Most studies published from India have not evaluated epidemiology of Acute Kidney Injury in the Intensive Care Unit setting and/or have not used validated criteria. In our observational study of 250 patients, admitted to a tertiary level ICU, we have explored the epidemiology of Acute Kidney Injury using both RIFLE and AKIN criteria and have validated them. We have also demonstrated that the severity of AKI is an independent predictor of mortality in critically ill patients. Our results are very much comparable to other studies and we feel that this study will remain as an epidemiological reference point for Indian clinicians dealing with AKI.
Introduction
Acute kidney injury (AKI) is common in intensive care unit (ICU) and is associated with increased mortality and cost of hospitalization.Citation1–3 AKI is an independent risk factor for mortality in critically ill patients. Epidemiology of AKI is diverse and varies with geography, race and socio-economic status. In addition, epidemiology of AKI differs between patients admitted to ICU and others. A study of epidemiologic pattern of AKI gives an insight in to the disease burden, disease pattern and thereby helps to prevent AKI as well as its deleterious consequences.
The epidemiology and outcomes of AKI in the ICU have been studied extensively in the western world.Citation4–9 In addition, Risk, Injury, Failure, Loss and End-stage Kidney (RIFLE) and AKI Network (AKIN) have been validated in several patient populations around the globe.Citation10–14 However, the epidemiology, outcomes of AKI and the validity of RIFLE and AKIN criteria in the Indian setting are largely unknown. Very few studies have attempted to explore the epidemiology of AKI in India.Citation15–20 However, these studies have either evaluated specific patient population or included patients outside the ICU, pediatric patients or have not used RIFLE or AKIN criteria to define, stratify or prognosticate AKI. Hence, in this study we aim to explore the epidemiology of AKI using both the RIFLE and AKIN criteria and to determine the prognostic validity of these criteria in an Indian ICU.
Patients and methods
Study population and data collection
We performed a prospective observational study, in a 75 bed tertiary hospital ICU on adult patients admitted during the period between 1 January 2009 to 31 July 2009 (7-month study duration), after obtaining institutional research ethics committee approval. Patients admitted to coronary care unit, patients re-admitted to ICU within a single hospital admission and patients with any known pre-existing renal disease (defined as baseline serum creatinine >1.3 mg/dL in men and >1.2 mg/dL in women when available) were excluded from the study. When baseline creatinine was not available, presence of pre-existing renal disease was made by the consulting nephrologist based on clinical grounds after incorporating presence or absence of proteinuria, patient co-morbidities and ultrasonography findings. Data including demographics, APACHE III score, presence of sepsis,Citation21 need for mechanical ventilation, need for dialysis, dialysis modality, ICU length of stay, ICU and 28-day hospital mortality were all collected. Both RIFLE and AKIN criteria were used to detect the presence and classify the severity of AKI when present. The individual patient’s worst RIFLE (RIFLEmax) and AKIN (AKINmax) class during the ICU stay was recorded and used for analysis.
RIFLE criteria
We classified patients according to their maximum RIFLE class (class R, class I or class F) during their hospital stay.Citation22,Citation23 Determination of the RIFLE class was done based on the worst of either glomerular filtration rate criteria or urine output criteria. We calculated a serum creatinine level using the modified diet in renal disease – MDRD equation (CrMDRD) as recommended by the Acute Dialysis Quality Initiative,Citation24 by solving the MDRD equation for serum creatinine assuming a glomerular filtration rate of 75 mL/minute/1.73 m2. We then used the lowest creatinine value among the hospital admission creatinine, the ICU admission creatinine or the MDRD creatinine as the baseline value. We used the change in this baseline serum creatinine level and urine output to classify patients according to the RIFLE criteria. Patients who met any of the criteria of the RIFLE classification were classified as acute kidney injury patients. We did not evaluate the outcome classes of RIFLE (loss and end-stage kidney disease criteria) in this study.
AKI Network criteria
We classified patients according to the maximum AKIN class (stage 1, stage 2 or stage 3) reached during their hospital stay.Citation25 AKIN class was determined similar to the RIFLE criteria, using worst of either glomerular filtration rate criteria or urine output criteria. Baseline creatinine value was calculated similar to that used for RIFLE classification.
Statistical analysis
Student t-test for quantitative variables and x2 test for qualitative variables were used for comparison. Kruskal–Wallis one-way analysis of variance (ANOVA) was used to compare mortality rates between groups. Survival analysis was performed using Kaplan–Meier curves. Logistic regression was performed to determine the factors associated with ICU mortality. The variables which have been known to affect the mortality in AKI and those with a p-value of <0.1 on univariate analysis were included in the multivariate regression analysis to predict mortality. Receiver operative characteristic curves (ROC) were plotted and area under the curve (AUC) was calculated for AKINmax and RIFLEmax to test their validity in predicting mortality. p < 0.05 was selected as the level of significance. Statistical analysis was done using the Statistical Package for Social Science (SPSS) version 17.0 (SPSS Inc., Chicago, IL).
Results
A total of 250 patients were included in our study (). Eight patients were discharged at their request and hence were not included in the analysis. Mean age of our study patients was 52.8 ± 17 and 61.6% were males. Mean APACHE III score of our patients was 48.19 ± 24.11. Sepsis was present in 59.5% (144/242) of study patients during their ICU stay. Mean ICU length of stay (LOS) was 7.35 ± 4.92 days. Overall mortality of the study population was 12.4% (30/242).
Table 1. Baseline characteristics of study patients (n = 242).
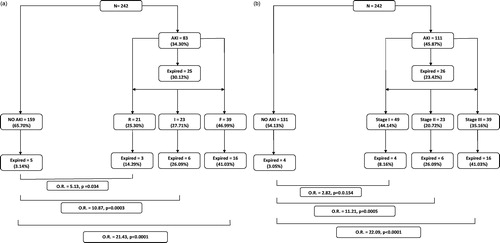
AKI – incidence and outcomes (RIFLE criteria)
AKI occurred in 34.3% (83/242) when RIFLE criteria were used to define AKI (). Among patients who had AKI during their ICU stay, Class R AKI was present in 25.3% patients, class I in 27.7% and class F was seen in 46.9% patients (). Renal replacement therapy (RRT) was initiated in 19.3% (16/83) patients, with continuous renal replacement therapy (CRRT) being the commonest mode (75%, 12/16 patients). Slow efficiency dialysis was initiated in 25% (4/16) patients. The need for RRT was 34.9% in RIFLE F group (15/39 patients). One patient who did not have AKI received dialysis for barbiturate overdose. There was no significant difference in the mean ICU LOS of patients with AKI compared to that of patients without AKI (8.1 ± 5.6 days vs. 7.0 ± 4.5; p = 0.10). Patients with AKI had a significantly higher 28-day mortality compared to patients without AKI (30.1% vs. 3.1%; p < 0.001). The mortality of class R, class I and class F AKI were 14.29%, 26.09% and 41.03% respectively ( and ). When compared to patients without AKI, the odds of death in Class R AKI was 5.13 (p = 0.034), in Class I AKI was 10.87 (p = 0.0003) and in Class F AKI was 21.43 (p < 0.0001) (Figure 1a).
Figure 2. (a) Survival of patients with and without AKI (RIFLE criteria). (b) Survival of patients with and without AKI (AKIN criteria).
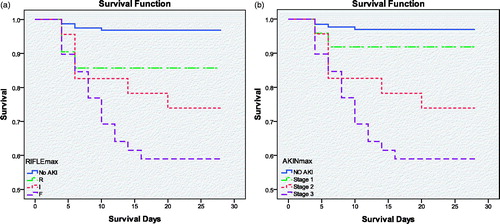
Table 2. Characteristics of patients with and without AKI (RIFLE Criteria).
AKI – incidence and outcomes (AKIN criteria)
When the AKIN criteria were applied, AKI was seen in 45.9% (111/242) patients (). Among patients who had AKI during their ICU stay, Stage 1 AKI was present in 44.1%, stage 2 in 20.7% and stage 3 was seen in 35.2% patients. Renal replacement therapy was necessary in 13.5% (15/111) patients with continuous renal replacement therapy being the commonest mode (80%, 12/15 patients). Slow efficiency dialysis was initiated in 20% (4/15) patients. The need for RRT was 34.9% in patients with stage III AKI (15/39 patients). The mean ICU LOS of patients with AKI was not significantly different than that of patients without AKI (7.8 ± 5.1 vs. 7.0 ± 4.7; p = 0.19). Mortality at 28 days was significantly higher in the AKI group compared to patients without AKI (23.4% vs. 3.1% p < 0.001). Stages 1, 2 and 3 of AKI had a mortality of 8.2%, 26.1% and 41.1% respectively ( and ). When compared to patients without AKI, the odds of death in stage I AKI was 2.82 (p = 0.15), in stage II AKI was 11.21 (p = 0.0005) and in stage III AKI was 22.09 (p < 0.0001) (Figure 1b).
Table 3. Characteristics of patients with and without AKI (AKIN Criteria).
Table 4. Predictors of mortality.
Predictors of ICU mortality
Logistic regression was done with age, sex, APACHE III, presence of sepsis, need for dialysis and severity of AKI (AKINmax) in the model with 28-day mortality as the outcome variable. We found that APACHE III score (Odds ratio 1.04; 95% CI 1.01–1.06; p < 0.002) and presence of AKI (Odds ratio 5.96; 95% CI 1.9–18.6; p < 0.002) were associated with higher mortality (). The results were similar when AKINmax was substituted in the model by RIFLEmax.
Table 5. Comparison of patients having AKI based on RIFLE and AKIN.
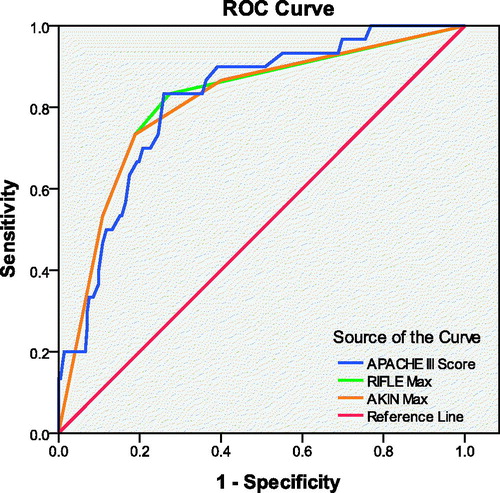
RIFLE criteria versus AKIN criteria ()
To compare the predictive abilities of RIFLE and AKIN criteria in predicting mortality of AKI, we analyzed area under the curve (AUC) of receiver operating characteristic curve (ROC) (). APACHE III score, RIFLEmax and AKINmax all showed good discrimination and were equally reliable in predicting mortality. AUC of ROC for APACHE III score was 0.82, while the AUC of ROC was 0.81 for both RIFLEmax and AKINmax (p < 0.001).
Discussion
In our single center study, AKI was diagnosed in 34.3% of patients based on RIFLE criteria and 45.9% of patients based on AKIN criteria. Our study results are very much similar to other studies from western countries that report an incidence of AKI of 20–50% depending on the criteria used and the patient population studied.Citation9,Citation12,Citation14,Citation26–28 In our study, incidence of AKI was higher when AKIN criteria was used compared to RIFLE criteria. This is very much expected since AKIN criteria uses a much smaller change in creatinine (>0.3 mg/dL from baseline) to define AKI. Similar findings have been reported in many previous studies.Citation29,Citation30
Although several studies from India have reported the epidemiology of AKI, very few studies have systematically explored the epidemiology of AKI in the critically ill population or have used validated criteria, such as RIFLE or AKIN. Most studies report an incidence of AKI of 10–40%, which is very similar to that of our results.Citation15,Citation16,Citation19,Citation31,Citation32 However, the slightly lower incidence of AKI noted in other studies is likely because of inclusion of patients outside the intensive care unit. In a small prospective observational studyCitation32 of 100 critically ill patients from North India, Paudel et al. reported 33% incidence of AKI based on AKIN criteria and very high mortality rate in patients with AKI (93.3%) as well as non-AKI patients (53.7%). The patients included in that study had a significantly higher severity of illness compared to our study likely explaining the higher mortality reported in their study.
Our results are in concordance with several other studies that have demonstrated increasing mortality with increasing severity of AKI.Citation33–35 In our study, patients even with early AKI (i.e., RIFLE – R and Stage I) AKI had a higher odds of death compared to no AKI. Other larger studies have shown similar results.Citation30,Citation33,Citation34 The relative risk of death was significantly higher in RIFLE R compared to no AKI, where as the difference was not significant between Stage 1 of AKIN and no AKI. This could be explained by the fact that AKIN is a more sensitive criteria and hence picks up patients with very minimal derangements in serum creatinine. It is plausible that when baseline serum creatinine is very low, minor increments of serum creatinine ≥0.3 mg/dL not amounting to more than 1.5-times of the baseline serum creatinine may indicate transient azotemia and may not have clinical relevance in terms of predicting mortality. This observation is in contrary to the results of a study by Chertow et al., who reported in a large cohort of patients a significant increase in mortality even with a small increment in serum creatinine of more than 0.3 mg/dL over the baseline value. However the baseline over which this increment occurred was not specified and not all patients in analysis had normal baseline serum creatinine. Our results do not support the notion that minor increment of serum creatinine not amounting to more than 1.5-times the baseline is associated with significant increase in the risk of mortality. Our study was a single-center, smaller study and could have been underpowered to show an increase in mortality with small changes in creatinine. It is also likely that good proportion of patients with stage I AKI, in our study had pre-renal azotemia from intravascular dehydration. Pre-renal azotemia is easily reversible and may not have an impact on mortality thereby diluting the effect of stage I AKI on mortality. The 28-day mortality of patients in our study, stratified by RIFLE and AKIN are comparable to that reported in other studies.Citation30,Citation33,Citation34 Our study results are also in agreement with other western studies that have reported good discriminatory ability of both RIFLE and AKIN criteria in predicting mortality.Citation30,Citation36
The need for RRT in our study was 19.3% when RIFLE criteria was used and only 13.5% when AKIN criteria was used. This difference in RRT rates seen between AKIN and RIFLE groups can be accounted for by the increased diagnosis of early AKI (i.e., more stage I AKI than class R) which does not require RRT. Rates of RRT in our study are much lower than that seen in several other western studiesCitation7,Citation14. However, another study from India has also reported similar lower rates of dialysis in AKI.Citation15 We speculate that several factors could contribute to the lower rate of RRT seen in our study. First, exclusion of patients with any pre-existing renal disease would have likely excluded a patient population at high risk for needing RRT. Second, it is likely that in third-world tropical countries, volume depletion is likely to be the major contributor to AKI. Hence higher rates of reversal of oliguria and AKI with lower rates of RRT requirement may be seen with aggressive fluid resuscitation. Third, there may be a conservative approach in initiating RRT in our population compared to the more liberal approach generally practiced in the western countries. Though there is general agreement on the absolute clinical indications to initiate RRT, no such consensus exist on the level of azotemia, severity or duration of AKI that warrants RRT. This lack of consensus regarding timing of initiation of RRT may account for wide variation in the initiation pattern of RRT in ICU worldwide. Lastly, it is likely that some of the patients who needed RRT died prior to initiation of RRT. This is plausible since health care is predominantly self-sponsored in the Indian setting and decisions regarding expensive supportive therapy such as RRT (especially continuous RRT) are more likely to be delayed compared to the west.
Previous studies have shown that general prognostic scores such as APACHE poorly discriminate between survivors and non-survivors in subgroups of patients with AKI.Citation37,Citation38 We however, applied APACHE III score to all patients admitted to our ICU rather than subgroup of patients with AKI. Hence in our study, APACHE III score and the presence of AKI seem to predict mortality.
Our study has several strengths. First, this is the largest prospective study exploring in detail the epidemiology and outcome of AKI in the Indian critical care unit setting. Second, our patient population is representative of most tertiary care mixed medical-surgical ICUs. Third, ours is the only study that has used and validated both RIFLE and AKIN criteria to evaluate epidemiology of AKI in heterogeneous population in ICU. We have used well validated methodology and applied robust statistics. However, our study has some limitations. First, our study reports data from a single tertiary centre and may not be representative of all Indian ICUs. Second, we used the MDRD criteria for calculating the baseline creatinine value. Although the MDRD equation was developed and validated on a large number of patients, conflicting results have been published regarding the validation of this equation in different patient populationsCitation39,Citation40. Hence using MDRD creatinine as the baseline creatinine could have led to a falsely high or low incidence of AKI.
Conclusion
Using the definitions of RIFLE and AKIN criteria, AKI is common in patients admitted to the Indian ICU and significantly increases 28-day mortality. APACHE III score and the severity of AKI are strongly associated with increased 28-day mortality. Both RIFLE and AKIN criteria seem to reliably predict outcomes.
Declaration of interest
The authors declare no conflicts of interests. The authors alone are responsible for the content and writing of this article.
References
- Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294:813–818
- Barrantes F, Tian J, Vazquez R, et al. Acute kidney injury criteria predict outcomes of critically ill patients. Crit Care Med. 2008;36:1397–1403
- Chertow GM, Burdick E, Honour M, et al. Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol. 2005;16:3365–3370
- Case J, Khan S, Khalid R, et al. Epidemiology of acute kidney injury in the intensive care unit. Crit Care Res Pract. 2013;2013:479–730
- Cole L, Bellomo R, Silvester W, et al. A prospective, multicenter study of the epidemiology, management, and outcome of severe acute renal failure in a “closed” ICU system. Am J Respir Crit Care Med. 2000;162:191–196
- Liano F, Junco E, Pascual J, et al. The spectrum of acute renal failure in the intensive care unit compared with that seen in other settings. The Madrid Acute Renal Failure Study Group. Kidney Int Suppl. 1998;66:S16–S24
- Mehta RL, Pascual MT, Soroko S, et al. Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int. 2004;66:1613–1621
- Odutayo A, Adhikari NK, Barton J, et al. Epidemiology of acute kidney injury in Canadian critical care units: a prospective cohort study. Can J Anaesth. 2012;59:934–942
- Piccinni P, Cruz DN, Gramaticopolo S, et al. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol. 2011;77:1072–1083
- Arnaoutakis GJ, George TJ, Robinson CW, et al. Severe acute kidney injury according to the RIFLE (risk, injury, failure, loss, end stage) criteria affects mortality in lung transplantation. J Heart Lung Transplant. 2011;30:1161–1168
- Chung KK, Stewart IJ, Gisler C, et al. The Acute Kidney Injury Network (AKIN) criteria applied in burns. J Burn Care Res. 2012;33:483–490
- Hoste EA, Clermont G, Kersten A, et al. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Crit Care. 2006;10:R73
- Jiang F, Chen YH, Liang XL, et al. The sensitivity and accuracy of RIFLE and AKIN criteria for acute kidney injury diagnosis in intensive care unit patients. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2011;23:759–762
- Ostermann M, Chang RW. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med. 2007;35:1837–1843
- Basu G, Chrispal A, Boorugu H, et al. Acute kidney injury in tropical acute febrile illness in a tertiary care centre – RIFLE criteria validation. Nephrol Dial Transplant. 2011;26:524–531
- Jha V, Malhotra HS, Sakhuja V, et al. Spectrum of hospital-acquired acute renal failure in the developing countries – Chandigarh study. Q J Med. 1992;83:497–505
- Kohli HS, Bhat A, Jairam A, et al. Predictors of mortality in acute renal failure in a developing country: a prospective study. Ren Fail. 2007;29:463–469
- Kohli HS, Bhat A, Aravindan AN, et al. Predictors of mortality in elderly patients with acute renal failure in a developing country. Int Urol Nephrol. 2007;39:339–344
- Krishnamurthy S, Mondal N, Narayanan P, et al. Incidence and etiology of acute kidney injury in southern India. Indian J Pediatr. 2013;80:183–189
- Singh TB, Rathore SS, Choudhury TA, et al. Hospital-acquired acute kidney injury in medical, surgical, and intensive care unit: a comparative study. Indian J Nephrol. 2013;23:24–29
- Dellinger RP, Carlet JM, Masur H, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858–873
- Bellomo R, Kellum JA, Ronco C. Defining and classifying acute renal failure: from advocacy to consensus and validation of the RIFLE criteria. Intensive Care Med. 2007;33:409–413
- Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004;8:R204–R212
- Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med. 1999;130:461–470
- Mehta RL, Kellum JA, Shah SV, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31
- Joannidis M, Metnitz B, Bauer P, et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 2009;35:1692–1702
- Mandelbaum T, Scott DJ, Lee J, et al. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med. 2011;39:2659–2664
- Thakar CV, Christianson A, Freyberg R, et al. Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study. Crit Care Med. 2009;37:2552–2558
- Bagshaw SM, George C, Bellomo R. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1569–1574
- Ratanarat R, Skulratanasak P, Tangkawattanakul N, et al. Clinical accuracy of RIFLE and Acute Kidney Injury Network (AKIN) criteria for predicting hospital mortality in critically ill patients with multi-organ dysfunction syndrome. J Med Assoc Thai. 2013;96:S224–S231
- Attur RP, Kuppasamy S, Bairy M, et al. Acute kidney injury in scrub typhus. Clin Exp Nephrol. 2013;17:725–729
- Paudel MS, Wig N, Mahajan S, et al. A study of incidence of AKI in critically ill patients. Ren Fail. 2013;34:1217–1222
- Thakar CV, Christianson A, Freyberg R, et al. Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study. Crit Care Med. 2009;37:2552–2558
- Bagshaw SM, George C, Dinu I, et al. A multi-centre evaluation of the RIFLE criteria for early acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1203–1210
- Ricci Z, Cruz D, Ronco C. The RIFLE criteria and mortality in acute kidney injury: a systematic review. Kidney Int. 2008;73:538–546
- Roy AK, Mc GC, Treacy C, et al. A comparison of traditional and novel definitions (RIFLE, AKIN, and KDIGO) of acute kidney injury for the prediction of outcomes in acute decompensated heart failure. Cardiorenal Med. 2013;3:26–37
- Fiaccadori E, Maggiore U, Lombardi M, et al. Predicting patient outcome from acute renal failure comparing three general severity of illness scoring systems. Kidney Int. 2000;58:283–292
- Mehta RL, Pascual MT, Gruta CG, et al. Refining predictive models in critically ill patients with acute renal failure. J Am Soc Nephrol. 2002;13:1350–1357
- Vervoort G, Willems HL, Wetzels JF. Assessment of glomerular filtration rate in healthy subjects and normoalbuminuric diabetic patients: validity of a new (MDRD) prediction equation. Nephrol Dial Transplant. 2002;17:1909–1913
- Botev R, Mallie JP, Wetzels JF, et al. The clinician and estimation of glomerular filtration rate by creatinine-based formulas: current limitations and quo vadis. Clin J Am Soc Nephrol. 2011;6:937–950