Abstract
A 68-year-old diabetic chronic kidney disease patient on continuous ambulatory peritoneal dialysis for two years developed Candida haemulonii peritonitis without any predisposing factors. There is no effective treatment for this fungus. A peritoneal biopsy showed morphological changes of acute inflammation and chronicity.
Introduction
In the last two and a half decades, a steady improvement in the survival of diabetics with ESRD has been observed and continuous ambulatory peritoneal dialysis (CAPD) has been the treatment of choice for an ever increasing number of uremic diabetics in developing countries. Uncontrolled diabetic state with comorbidities predisposes diabetic patients to cardiovascular and infective complications.Citation1,Citation2 Microbiological diagnosis using different tools and peritoneal biopsy had been previously reported as supplementary investigation in the proper diagnosis of fungal peritonitis.Citation3
Case report
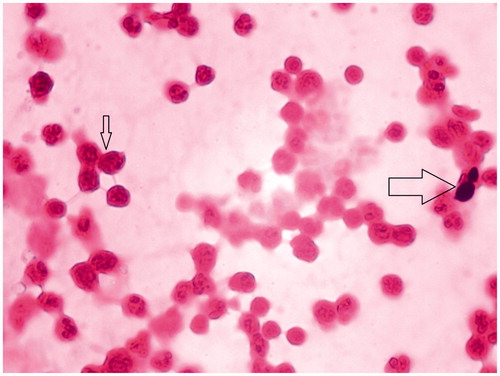
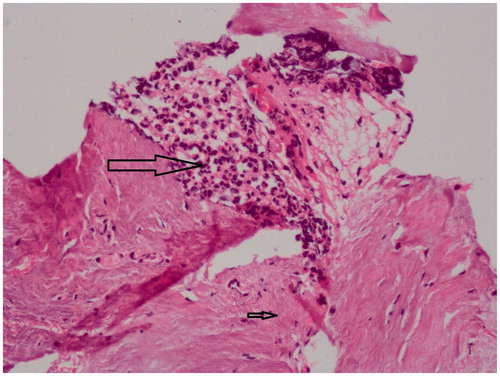
A 68 years old lady with diabetic chronic kidney disease (CKD) stage 5 was on CAPD using swan neck double cuff Tenckhoff catheter for 2 years. She was doing three exchanges of Dianeal round the clock with 2 L × 2 bags of 2.5% and 2 L × 1 bag of 1.5%, with an ultrafiltration volume which varied from 1.2 to 1.4 L/day. She had suboptimal diabetic control with HBA1c of 9.7%. She came with abdominal pain since 1 day. Dialysate effluent showed leucocyte count 5.9 × 109/L with neutrophils 0.98, lymphocytes 0.02. Hemoglobin (Hb) was 98 g/L, BUN was 11.78 mmol/L, creatinine 362.4 mmol/L, serum albumin 26 g/L and electrolytes were normal except K+ 3.2 mmol/L. She was initiated on standard ISPD guideline peritonitis treatment. Dialysate effluent sent for microbiology showed fungal elements on KOH, and hence PD catheter was removed after 24 hours. A two D ECHO done pre-operatively showed normal LV function. While removing the catheter as a part of our protocol, a peritoneal biopsy was done. The catheter tip and dialysate effluent grew Candida haemulonii () identified with Vitek II compact (bioMerieux, SA, France). She was dialyzed through an internal jugular catheter. However her abdominal pain continued and she was initiated on voriconazole 200MG BID IV. She succumbed to a cardiac arrest on the third day and could not be resuscitated. The peritoneal biopsy showed fibrosis with neutrophilic exudates (). She had no recent prior exposure to oral/intravenous antibiotics and had no vaginal discharge.
Discussion
Fungal peritonitis accounts for about 4–6% of the episodes although Candida is by far the most common organism. In an Indian study, fungal peritonitis accounted for 23.88% of all peritonitis episodes.Citation4 Three factors appeared to predict mortality: the presence of non-Candida species, the catheter being left in situ and a serum albumin level <3 g/dL.Citation4
As peritoneal biopsy is rarely done in clinical practice unless it is a protocol procedure, a significant proportion of information on morphology is unavailable to the treating physician to predict the outcome. The peritoneal biopsy showed areas of fibrosis with neutrophilic infiltration. Although an EM was not done, the presence of fibrosis in peritoneum in our patient showed discordance with ultrafiltration capacity as her ultrafiltration was good prior to the development of peritonitis. This could probably due to diabetic changes in the peritoneum, continuous exposure to GDP using dialysis fluid based on glucose and sampling. Biopsy also showed neutrophilic phenotype as lymphocyte predominance is commonly reported with fungal peritonitis. This could be attributed to recent onset of infection before the biopsy.
Candida haemulonii, one of the non-albicans Candida species, is an emerging yeast pathogen that is known to be resistant to amphotericin B and other antifungal agents such as azoles. These anti-fungal agents have often been associated with clinical treatment failure. An echinocandin such as caspofungin may be an empirical choice of antifungal agent for an invasive C. haemulonii infection. So far no successful treatment regimen has been clearly established for treatment of C. haemulonii fungal peritonitis. A literature search revealed no previous reports of C. haemulonii fungal peritonitis in patients on CAPD. Noteworthy is the susceptibility profile of this yeast that shows high minimal inhibitory concentrations (MIC) for amphotericin B (AMB) and fluconazole (FLC) (range 0.5–32; mg/L and 4–>64; mg/L, respectively), which can hinder the management of patients with deep infections caused by this yeast.Citation5
Candida haemulonii is one of the rare yeast species that can be isolated from 49 human clinical sources. The first isolation of this yeast from humans was reported from the blood of a patient with renal failure. Since then, several cases of infections due to this yeast have been described in the literature, varying from superficial to deep infections, other than peritonitis. The species has also been isolated from toe nails of diabetic patients.Citation5
In another Indian study, the incidence of fungal peritonitis was 16.2% with mortality in 20%.Citation6 This patient did not have risk factors for fungal peritonitis and had no exit site infection. However, in this lady, despite catheter removal within 24 hours and switch over to hemodialysis which she could not tolerate and suffered a sudden cardiac death which is not unusual in a diabetic CKD patient. This case highlights the importance of diagnosing rare fungal infections in diabetic patients and the value of peritoneal biopsy in predicting long-term morphological changes.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Abraham G, Zlotnik M, Ayiomamitis A, Oreopoulus DG. Dropout of diabetic patients from CAPD. Adv CAPD. 1987;7:199–203
- Abraham G, Kumar V, Nayak KS, et al. Predictors of long-term survival on peritoneal dialysis in South India: A multicenter study. Perit Dial Int. 2010;30(1):29–34
- Pavithra M, Lakshmi R, Gautam G, et al. Three patients on CAPD for ten years – Once a life time scheme. Indian J Perit Dial. 2012;22:32–36
- Ram R, Swarnalatha G, Neela P, Dakshina Murty KV. Fungal peritonitis in patients on continuous ambulatory peritoneal dialysis: A single centre experience in India. Nephron Clin Pract. 2008;110:c207–c212
- Cendejas-Bueno E, Kolecka A, Alastruey-Izquierdo A, et al. Reclassification of the Candida haemulonii complex; C. duobushemulonii sp. nov. (C. haemulonii group II) and C. haemulonii var. vulnera var. nov.: Three multiresistant human pathogenic yeasts. J Clin Microbiol. 2012;50(11):3641–3651
- Indhumathi E, Chandrasekaran V, Jagadeswaran D, Varadarajan M, Abraham G, Soundararajan P. The risk factors and outcome of fungal peritonitis in continuous ambulatory peritoneal dialysis patients. Indian J Med Microbiol. 2009;27:59–61