Abstract
Background: Intra-abdominal free air is found frequently in patients undergoing peritoneal dialysis (PD). Some studies have investigated an association between intra-abdominal free air and peritonitis in PD patients. However, most used chest X-rays, which are of limited sensitivity, and the association was not made clear. We conducted a retrospective study of the association between peritonitis and intra-abdominal free air using computed tomography. Methods: The presence and volume of free air, and its relationship with other variables, were assessed on review of routine examinations in 108 patients. Correlations between the presence of free air and age, duration of PD, continuous ambulatory versus automated PD, presence or absence of a person who assisted in bag changes, exit-site infection, tunnel infection and peritonitis were assessed. Results: Free air was detected in 29 patients (27.1%). The prevalence of peritonitis was higher in the free air (+) group than in the free air (−) group: 1/40.2 patient-months for free air (+) versus 1/96.9 patient-months for free air (−). The risk ratio of free air for peritonitis was 2.41 (95% confidence interval: 2.28–2.55) and was similar when corrected for age, gender, albumin, diabetes mellitus and body mass index. Conclusion: Free air is an independent risk factor for peritonitis in PD patients. This suggests that bag change procedures should be re-evaluated, and patients re-educated, when necessary.
Introduction
In the general population, intra-abdominal free air is known to be a sign of a perforated viscus in an intact abdomen.Citation1 In asymptomatic peritoneal dialysis (PD) patients, free air is a common occurrence on chest X-ray (10.7–33.7%).Citation2–5 In PD patients with abdominal pain, free air is rarely associated with viscus perforation.Citation6
Infections are a major concern in the PD population.Citation7 The overall rate of PD-associated infection is 0.24–1.66 episodes per patient-year on dialysis.Citation8–17 Some studies investigating peritonitis in PD patients have found a certain proportion of patients to have intra-abdominal free air.Citation2,Citation6
It is not clear whether peritonitis in PD patients with free air is caused by contaminated outside air entering the abdominal cavity or by touch contamination of the PD system. Currently, many patients use a bag-exchange device based on a “Y” set and ultraviolet light sterilization. With this system, any air entering the abdominal cavity is sterile.Citation18,Citation19 This suggests the cause of the association between peritonitis and intra-abdominal free air may be touch contamination of the PD system.
In our institution, all patients undergo annual routine abdominal computed tomography (CT), which is more sensitive for free air than chest X-ray.Citation20–23 All patients use a bag-exchange device sterilized by ultraviolet light. In order to clarify whether intra-abdominal free air is a risk factor for peritonitis caused by touch contamination, we conducted a retrospective study to detect any association between peritonitis and intra-abdominal free air on CT.
Subjects and methods
The study was conducted at a single center under a retrospective design. We included PD patients who had undergone a check-up including abdominal CT at Oji Hospital between April 2009 and March 2010. We excluded patients whose PD catheter insertion occurred less than one month previously, those whose connection tube was changed less than one month previously and those undergoing automated PD in a cold region (to avoid cases of dissolved air being released with warming). All patients used a PD system (Dianeal-N®, Extraneal®; Baxter Healthcare™, Tokyo, Japan) and a bag-exchange device based on an ultraviolet light irradiation joint system (UV FLASH AUTO®, Medi-Tech, Inc.™, Tokyo, Japan).
Free air was assessed on CT (Activion16®, Toshiba™ Medical Systems, Tokyo, Japan). To detect free air, CT images were viewed with adjusted settings (window = 500, level = 40) to differentiate air from fat. Isolated collections not continuous with the gastrointestinal tract were judged to be free air.
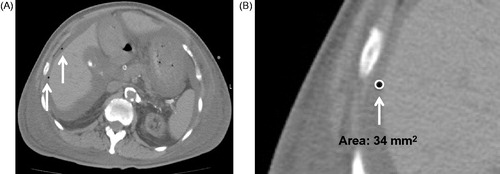
Free air was measured using on-board software in the CT system. The volume of free air was calculated from the largest cross-sectional area assuming a spheroid morphology (free air volume [mm3] = 4 × area [mm2]/3 × radius) ().
Figure 1. The volume of free air was estimated on the assumption that it was spherical by calculating its cross-sectional area in the plane with a maximum diameter using application software.
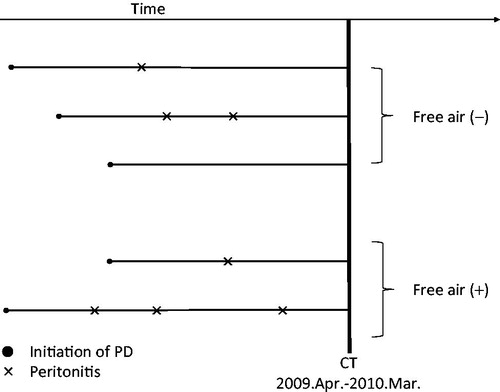
If multiple pockets of free air were detected, they were summed to give a total volume. The diagnosis of PD-associated peritonitis was based on the medical records (). Diagnosis was according to the guidelines proposed by the International Society of Peritoneal Dialysis (ISPD).Citation24,Citation25 In accordance with these guidelines, the infecting organisms in all peritonitis patients who had had peritonitis were recorded. We calculated the prevalence of PD-related peritonitis in terms of the length of time on PD. We calculated the risk ratio and 95% confidence interval (CI) to compare the prevalence of PD-related infections between patients with free air and those without. We recorded age, gender, dialysis history, body mass index (BMI), serum albumin, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides and the presence or absence of diabetes mellitus (DM). We treated continuous data, including age, BMI and serum albumin, as categorical data. We set cut-off values for categorical data as per a previous study.Citation26,Citation27
Figure 2. Free air was measured on routine computed tomography (CT) examinations from April 2009 to March 2010. Episodes of peritonitis were measured retrospectively from PD introduction to the CT measurement point.
This study was approved by the Oji Hospital Institutional Review Board and Ethics Committee (Approval no. 15), and all participating patients gave written informed consent.
All statistical analyses were performed using commercial software (Stata® version 11.2 Stata Corp.™, College Station, TX) with two-sided significance set at 0.05. Data are expressed as the mean ± standard deviation or the median (interquartile range) for normal and non-normal continuous variables, respectively. Univariate analyses were performed using Student’s t-test, the Mann–Whitney U test and the chi-squared test. A direct standardization method was used to estimate risk ratios and 95% CIs adjusted for age and sex.Citation28 Stratified analysis was done using BMI, serum albumin and DM as prognosticators with adjustment for age.
Results
We examined 108 PD patients [66 males and 42 females (median age: 61 years; interquartile range: 55–75 years)] with a median PD duration of 29.5 months (interquartile range: 11–61.5 months). Free air was detected in 29 patients (27.1%) on CT.
The relationships between free air and various factors were evaluated (). First, comparisons were made between the 29 patients who had free air on CT and the 79 patients who had no free air. No significant difference was noted in the presence of intra-abdominal free air or its volume based on differences in treatments [automated peritoneal dialysis or continuous ambulatory peritoneal dialysis (CAPD), length of time on PD, or presence or absence of exit-site/tunnel infection]. The prevalence of peritonitis was 1 per 39.6 patient-months and 0.29 per patient-year in those with intra-abdominal free air, and 1 per 97.0 patient-months and 0.12 per patient-year () in those without intra-abdominal free air. Thirty-eight of 108 patients had previously had peritonitis. In these 38 patients, 17 were in the free air (+) group and 21 were in the free air (−) group. In other words, 17 of 29 patients (58.6%) in the free air (+) group and 21 of 79 patients (26.8%) in the free air (−) group had previously had peritonitis (p = 0.002). The risk ratio of free air for peritonitis was adjusted according to possible prognostic factors (age, gender, albumin, DM and BMI), and free air was identified as an independent risk factor for peritonitis. The risk ratio of free air for peritonitis was 2.41 (). We investigated the relationship between the volume of free air and prevalence of peritonitis in the free air (+) group. There was no significant correlation between the median free air volume in the 15 patients who had previously had peritonitis (202.7 mm3, interquartile range: 30.2–444.4) and the 11 patients who had not had peritonitis (143.0 mm3, interquartile range: 67.6–838.2; p = 0.42). No difference was noted in the causative microorganisms of peritonitis between the free air (−) and free air (+) groups ().
Table 1. Characteristics of the study population.
Table 2. Incidence of peritoneal dialysis-related infections.
Table 3. Risk ratio of free air for peritonitis.
Table 4. Bacterial species causing peritonitis.
Discussion
In this retrospective study of the association between peritonitis and intra-abdominal free air using CT, we found that the prevalence of peritonitis was significantly higher in patients with free air than in patients without free air. No correlation was detected between the volume of free air and history of peritonitis. We therefore concluded that the presence of intra-abdominal free air on CT is an independent risk factor for peritonitis in PD patients and may identify patients in need of interventions to improve suboptimal PD technique and reduce touch contamination.
Free air on CT in PD patients may be related to poor PD technique from inadequate patient training and may carry an increased risk of peritonitis. The volume of air that may escape from the bag or tube using dialysis bags (Dianeal-N®, Extraneal®; Baxter Healthcare™) is approximately 11 mL without priming. That is, a maximum of 44 mL of air may enter the abdominal cavity when CAPD is performed using four bags per day. The mean decrease in volume of free air through absorption is 13.5 mL per day.Citation29 We calculated the intra-abdominal free air as the difference between the inflow and the absorption of air. Inadequate procedures during PD bag exchange could introduce free air. However, all patients use a bag-exchange device based on an ultraviolet light irradiation joint system. Air in the dialysis solution bag is sterile, so that inflow of air from the bag into the abdominal cavity is harmless. For these reasons, free air may be a surrogate marker for other inadequate procedures in exchanging PD bags, namely, inadequate sterile technique.
No correlation was detected between the volume of free air and prevalence of peritonitis, only the presence or absence of free air. The awareness that the presence of free air may be a sign of imperfect sterile technique may help to reduce risk of peritonitis among PD patients. PD patients with free air could be targeted to receive advanced nursing and patient training in dialysis bag exchange to lower the risk of technical failure of bag exchange and touch contamination.Citation30–33 These interventions may reduce the prevalence of peritonitis among PD patients. In this study, we showed that PD patients who have intra-abdominal free air have a higher risk of peritonitis.
There are several limitations to this study. First, the study was conducted under a retrospective design based on chart review. We specifically searched back for the number of peritonitis episodes since the initiation of PD in patients undergoing CT. Second, free air was measured with CT only once. Third, only 108 patients were evaluated. Although sufficient to evaluate CIs in univariate analysis, this sample was not large enough to evaluate CIs in multivariate analyses, which included multiple confounders at the same time. However, these limitations may not have affected our conclusion. Patients who did not undergo CT until a transfer or death were excluded. Unmeasured confounders might also have been present, which may have limited the validity of the results. These limitations need to be resolved in future prospective studies.
Conclusion
Intra-abdominal free air on CT in PD patients is related to the prevalence of peritonitis. This result might be based on poor PD technique and touch contamination. The presence of free air on CT may identify patients in need of intervention to improve suboptimal PD technique and reduce touch contamination. Intra-abdominal free air on CT in PD patients suggests that bag change procedures should be re-evaluated, and patients re-educated, when necessary.
Declaration of interest
All authors declare no competing interest.
References
- Winek TG, Mosely HS, Grout G, Luallin D. Pneumoperitoneum and its association with ruptured abdominal viscus. Arch Surg. 1988;123:709–712
- Kiefer T, Schenk U, Weber J, Hubel E, Kuhlmann U. Incidence and significance of pneumoperitoneum in continuous ambulatory peritoneal dialysis. Am J Kidney Dis. 1993;22:30–35
- Lee FT Jr, Leahy-Gross KM, Hammond TG, Wakeen MJ, Zimmerman SW. Pneumoperitoneum in peritoneal dialysis patients: Significance of diagnosis by CT. J Comput Assist Tomo. 1994;18:439–442
- Daly BD, Guthrie JA, Couse NF. Pneumoperitoneum without peritonitis. Postgrad Med J. 1991;67:999–1003
- Lampainen E, Khanna R, Schaefer R, Twardowski ZJ, Nolph KD. Is air under the diaphragm a significant finding in CAPD patients? ASAIO Trans. 1986;32:581–582
- Ergun T, Lakadamyal H. The CT frequencies of various non-traumatic acute abdominal emergencies in hemodialysis, peritoneal dialysis patients and the general population. Eur J Radiol. 2012;81:13–20
- Friedrich AK, Cahan M. Intraabdominal infections in the intensive care unit. J Intensive Care Med. 2013. [Epub ahead of print]. doi: 10.1177/0885066613476465
- Han SH, Lee SC, Ahn SV, et al. Improving outcome of CAPD: Twenty-five years’ experience in a single Korean center. Perit Dial Int. 2007;27:432–440
- Li PK, Law MC, Chow KM, et al. Comparison of clinical outcome and ease of handling in two double-bag systems in continuous ambulatory peritoneal dialysis: A prospective, randomized, controlled, multicenter study. Am J Kidney Dis. 2002;40:373–380
- Nessim SJ, Bargman JM, Jassal SV. Relationship between double-cuff versus single-cuff peritoneal dialysis catheters and risk of peritonitis. Nephrol Dial Transplant. 2010;25:2310–2314
- Goffin E, Herbiet L, Pouthier D, et al. Vancomycin and ciprofloxacin: Systemic antibiotic administration for peritoneal dialysis-associated peritonitis. Perit Dial Int. 2004;24:433–439
- Boehm M, Vecsei A, Aufricht C, Mueller T, Csaicsich D, Arbeiter K. Risk factors for peritonitis in pediatric peritoneal dialysis: A single-center study. Pediatr Nephrol. 2005;20:1478–1483
- Prasad N, Gupta A, Sharma RK, Prasad KN, Gulati S, Sharma AP. Outcome of gram-positive and gram-negative peritonitis in patients on continuous ambulatory peritoneal dialysis: A single-center experience. Perit Dial Int. 2003;23(Suppl 2):S144–S147
- Edey M, Hawley CM, McDonald SP, et al. Enterococcal peritonitis in Australian peritoneal dialysis patients: Predictors, treatment and outcomes in 116 cases. Nephrol Dial Transplant. 2010;25:1272–1278
- Freitas C, Rodrigues A, Carvalho MJ, Cabrita A. Exit site infections: Systematic microbiologic and quality control are needed. Adv Perit Dial. 2009;25:26–31
- Lobo JV, Villar KR, de Andrade Junior MP, Bastos Kde A. Predictor factors of peritoneal dialysis-related peritonitis. J Bras Nefrol. 2010;32:156–164
- Renaud CJ, Subramanian S, Tambyah PA, Lee EJ. The clinical course of rapidly growing nontuberculous mycobacterial peritoneal dialysis infections in Asians: A case series and literature review. Nephrology. 2011;16:174–179
- Buoncristiani U, Buoncristiani E, Bianchi P. Use of sodium hypochlorite in peritoneal dialysis: The genesis of the ‘Y’ set and beyond. Contrib Nephrol. 2007;154:103–116
- Stegmayr B. Various clinical approaches to minimise complications in peritoneal dialysis. Int J Artif Organs. 2002;25:365–372
- Braccini G, Lamacchia M, Boraschi P, et al. Ultrasound versus plain film in the detection of pneumoperitoneum. Abdom Imaging. 1996;21:404–412
- Chen SC, Yen ZS, Wang HP, Lin FY, Hsu CY, Chen WJ. Ultrasonography is superior to plain radiography in the diagnosis of pneumoperitoneum. Br J Surg. 2002;89:351–354
- Chen CH, Huang HS, Yang CC, Yeh YH. The features of perforated peptic ulcers in conventional computed tomography. Hepatogastroenterology. 2001;48:1393–1396
- Oguro S, Funabiki T, Hosoda K, et al. 64-Slice multidetector computed tomography evaluation of gastrointestinal tract perforation site: Detectability of direct findings in upper and lower GI tract. Eur Rad. 2010;20:1396–1403
- Li PK, Szeto CC, Piraino B, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int. 2010;30:393–423
- Piraino B, Bailie GR, Bernardini J, et al. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005;25:107–131
- Hsieh YP, Chang CC, Wen YK, Chiu PF, Yang Y. Predictors of peritonitis and the impact of peritonitis on clinical outcomes of continuous ambulatory peritoneal dialysis patients in Taiwan—10 years’ experience in a single center. Perit Dial Int. 2014;34:85–94
- Fouque D, Kalantar-Zadeh K, Kopple J, et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008;73:391–398
- Curtin L, Klein R. Direct standardization (age-adjusted death rates) Healthy People 2000 Stat Notes. 1995. Available at: http://www.cdc.gov/nchs/data/statnt/statnt06rv.pdf. Accessed March 15, 2014
- Stanley IR, Laurence AS, Hill JC. Disappearance of intraperitoneal gas following gynaecological laparoscopy. Anaesthesia. 2002;57:57–61
- Yang Z, Xu R, Zhuo M, Dong J. Advanced nursing experience is beneficial for lowering the peritonitis rate in patients on peritoneal dialysis. Perit Dial Int. 2012;32:60–66
- Holloway M, Mujais S, Kandert M, Warady BA. Pediatric peritoneal dialysis training: Characteristics and impact on peritonitis rates. Perit Dial Int. 2001;21:401–404
- Bernardini J, Price V, Figueiredo A. Peritoneal dialysis patient training, 2006. Perit Dial Int. 2006;26:625–632
- Hall G, Bogan A, Dreis S, et al. New directions in peritoneal dialysis patient training. Nephrol Nurs J. 2004;31:149–154, 159–163

