Abstract
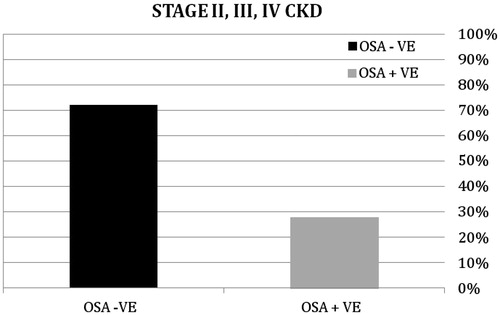
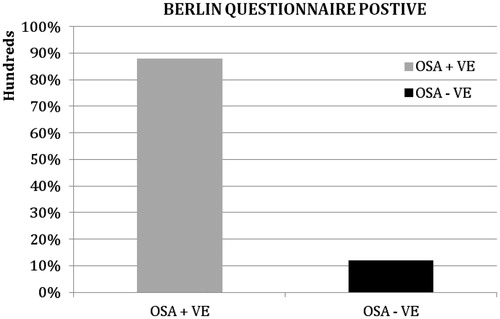
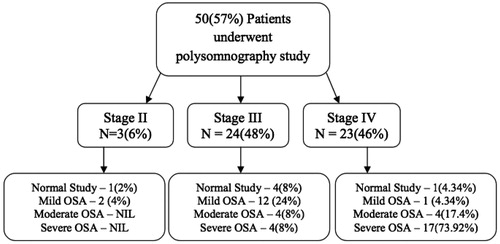
There is an enormous increase in the burden of chronic kidney disease both in developing and developed countries. There is a paucity of data on obstructive sleep apnea (OSA) in chronic kidney disease (CKD) patients in India. We used a cross-sectional prospective observational study to determine the prevalence of OSA in non-dialysis CKD patients. Of the 647 CKD patients 302 patients were in stage II, III and IV. The study population was screened using the Berlin questionnaire and 87 patients were positive for OSA (28%). Among the 87, 37 patients were excluded based on the exclusion criteria. Fifty patients underwent a split night sleep study. Stage II, III CKD patients were clubbed as early CKD or group one and stage IV CKD patients were clubbed as late CKD or group two. The spilt night study revealed an 88% incidence of OSA of varying severity. A sub group analysis was done to assess the severity of OSA. A statistical significance (p < 0.05) between early and late CKD group was observed with respect to AHI and ODI. An improvement in the late CKD is observed and the Z values for AHI and ODI are 4.273 and 2.307, respectively. The prevalence and incidence of OSA was found to be 28% and 88% in non-dialysis CKD patients, respectively and the risk and severity of OSA increased with the progression of CKD stages and thus necessitating the need for screening the non-dialysis CKD population.
Introduction
Chronic kidney disease (CKD) encompasses a spectrum of different pathophysiologic processes associated with abnormal kidney function and a progressive decline in glomerular filtration rate (GFR).Citation1 Prevalence is estimated to be 8–16% worldwide.Citation2 The Indian CKD registry and previous studies done in Indian population revealed an approximate prevalence of 17.2% with preponderance of male sex.Citation3,Citation4 Obstructive sleep apnea (OSA) happens to be the most common form of sleep disordered breathing (SDB) and was recognized more than 30 years ago and presents as complete or partial blockage of the upper airway during sleep.Citation5 Population-based studies in the developed countries have shown that up to 6% of adults are likely to have undiagnosed OSA.Citation6,Citation7 Studies conducted on general population to assess the prevalence of OSA in India reveals a prevalence ranging from 7 to 20%.Citation8,Citation9 Several studies in developed countries on CKD patients have shown a higher prevalence of SDB ranging from 18 to 80% with prevalence in maintenance of hemodialysis patients to be 50–80%.Citation10–13 Studies have shown that OSA in CKD patients are present with non-specific symptoms like tiredness, headache, decreased sleep during night, increased day time somnolence, and snoring.Citation14–16 These risks increase twofold when the two disorders CKD and OSA coexist.Citation9–11,Citation15 OSA carries increased morbidity due to hypertension, coronary artery disease, cardiac arrhythmias and stroke.Citation16
The increased prevalence of OSA in CKD patients can be attributed to reduction in upper airway dimensions in patients with renal failure.Citation1,Citation14,Citation17–20 Beecroft et al. reported that the pharyngeal cross-sectional area measured by pharyngometry in ESRD patients was 12% less than that in the normal renal function control group matched for BMI.Citation21 Such pharyngeal narrowing was considered to occur because of upper airway edema due to systemic fluid overload and upper airway dilator muscle dysfunction due to neuropathy or myopathy associated with chronic uremia. Ventilation control is known to be unstable in CKD patients. Chemoreflex responsiveness has been reported to be augmented in patients with CKD V, possibly because of the accumulation of uremic molecules or metabolic acidosis, explained by a high “loop gain” theory, which contributes to the pathogenesis of OSA in CKD.Citation21 Upper airway dilator muscle dysfunction secondary to neuropathy or myopathy associated with either chronic uratemia or the underlying cause of CKD, such as diabetes mellitus can attribute to OSA.Citation22
There is a paucity of data in the Indian population. Hence, this prospective study was undertaken to assess the prevalence of OSA in CKD patients not on dialysis.
Methods
Study design
We performed a cross-sectional, prospective observational study in a tertiary care center in South India, enrolling patients between January 2012 and July 2013. All CKD patients attending the outpatient department of general medicine and nephrology were assessed with Cockroft – Gault equation to stage the CKD. Patients in Stage II, III and IV of CKD were enrolled in the study. This population was screened for OSA with Berlin questionnaire.Citation23 The patients who were at high risk in accordance to Berlin questionnaire were enrolled for the study. Patients were not included on the basis of exclusion criteria such as obesity (BMI > 27 kg/m2) in accordance to the Indian guidelines.Citation24 Other exclusion were hemoglobin <12 g/dL, abnormal thyroid function tests, CNS depressant drug usage or alcohol abuse within the last one week and clinical conditions like COPD and bronchial asthma. The study population was divided into two groups; group 1 comprising of Stage II– III (early CKD) and the group 2 Stage IV (late CKD) patients. After getting the institutional ethics committee approval and a written consent from the patient about the polysomnography study, patients in both the groups underwent a diagnostic split night sleep study. The first phase of the study that is, first three hours of the study was for diagnosis of OSA and if the patient was OSA positive, a titration of continuous positive airway pressure (CPAP) was done during the second phase of the study. The diagnosis of OSA was made based on the apnea hypopnea index (AHI) and oxygen de-saturation index (ODI), which is the number of apneas and hypopneas per hour of sleep.Citation16 An apnea is defined as the complete cessation of airflow for at least 10 s and a hypopnea is defined as a reduction in airflow (30–50%) that is followed by an arousal from sleep or a decrease in oxy-hemoglobin saturation (3–4%).Citation22,Citation25–27 AHI of 5–15 is considered as mild OSA, 16–30 as moderate OSA and AHI of 30 or more as severe OSA.Citation22 After the sleep study the OSA patients were informed about the disorder and the treatment options including CPAP therapy were emphasized.
Statistical analysis
The study was to assess the prevalence of OSA and hence descriptive statistics was used. All the results were calculated using IBM SPSS version 22.0 software (Armonk, NY). Continuous variables were presented as median values or interquartile ranges, and categorical variables were presented as frequency (number) and proportions.
The Mann–Whitney U-test statistic was applied between the two groups due to the limited population in the two groups and a Z test was applied in the aspect to the AHI and ODI. A subgroup analysis was done to assess the incidence and severity of OSA in each stage of CKD.
Results
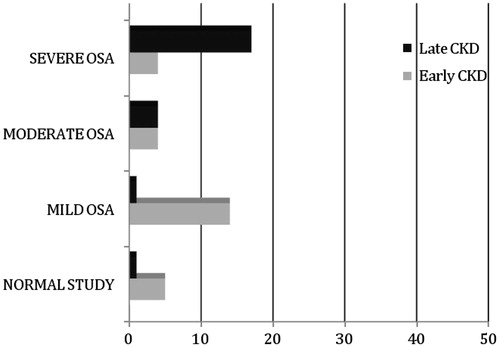
The baseline characteristics of the study population are summarized in . A total of 647 CKD patients were screened and 302 (46.67%) patients were in stage II, III and IV of CKD. Among the 302 patients 87 (28.81%) were in stage II, 104 (34.44%) in stage III and 111 (36.75%) in stage IV of CKD. Eighty-seven (28%) among the 302 patients were at high risk for OSA in Berlin questionnaire (). Thirty-seven (42.5%) among the 87 patients were excluded based on the exclusion criteria. Fifty patients were divided into group 1 and group 2 who underwent split night sleep study for polysomnography testing (). The prevalence of OSA was found to be 28% after screening the population with Berlin questionnaire. The incidence of OSA was found to be 88% in the Berlin questionnaire positive group after polysomnography (). A sub-group analysis was done to assess the severity of OSA which revealed 5 (18.51%) had normal study with AHI less than 5, 14 (51.85%) had mild sleep apnea with AHI ranging between 5 and 15, 4 had moderate OSA with AHI ranging between 16 and 30 and 4 had severe OSA with AHI more than 30 in the early CKD group. In the late CKD group 1 (4.34%) had normal study with AHI less than 5, 1 (4.34%) had mild OSA with ranging between 5 and 15, 4 (17.4%) had moderate OSA with AHI ranging between 16 and 30 and 17 (73.92%) had severe OSA with AHI more than 30 (). The prevalence of OSA in various stages of CKD was assessed. There was 6% incidence in the stage II with mild and moderate forms of OSA. The incidence of OSA in stage III was 48% with majority of the patients having mild and moderate OSA. The incidence of OSA in stage IV CKD was 46% with the majority of the patients having severe OSA than mild to moderate form of the disease (). The Mann–Whitney U-test statistics was applied and a statistical significance (p < 0.05) between early and late CKD with respect to AHI and ODI was observed (). An improvement in the late CKD is observed and the Z values for AHI and ODI were 4.273 and 2.307, respectively ().
Table 1. Baseline characteristics.
Table 2. Groups 1 and 2.
Table 3. AHI between the early CKD and the late CKD groups.
Table 4. AHI and ODI between the two groups.
The pattern of cardiac rhythms that were observed in the ECG during the study was sinus rhythm, premature ventricular complexes, and sinus tachycardia. Of the 27 patients in early CKD group 2 (7%) had sinus tachycardia, 3 (12%) had premature ventricular complexes and 22 (81%) had sinus rhythm. In the late CKD group 2 (9%) had sinus tachycardia, 1 (4%) had premature ventricular complexes and 20 (87%) had sinus rhythm. The number of arousals was determined by arousal index which was determined by EEG. The transition from delta or theta wave to alpha or beta wave was considered an arousal. In the early CKD group 13 (48%) had an arousal and 14 (52%) had no arousal. In the late CKD group 14 (61%) had arousal and 9 (39%) patients had no arousal. One patient in the late CKD group had periodic leg movement syndrome which was determined by periodic leg movement index.
Discussion
Our study revealed the prevalence and incidence of OSA in non-dialysis CKD patients to be 28% and 88%, respectively. This shows a high incidence of OSA in non-dialysis CKD which had not been looked at in Indian CKD population. This study has limitations because it is a cross-sectional analysis. We found that there is an increased risk of OSA associated with a decline of kidney functions in CKD patients.
To our knowledge this is the first study in South Indian population to assess the prevalence of OSA in non-dialysis CKD patients. Previous studies conducted in India on maintenance hemodialysis showed a prevalence of 24.6%, however, the true incidence was not assessed.Citation9,Citation17 A study by Sakaguchi et al. conducted in non-dialysis CKD population in Japan revealed a high prevalence of 65%, though an initial screening test was not employed as we have done and confounding factors like anemia, thyroid disorders and COPD were not excluded.Citation19 Another study by Markou et al., showed a prevalence of OSA at 54.3% in 35 non-dialysis CKD patients.Citation20
A study by Roumelioti et al., with a median age of 58.1 years in stage IV to V CKD patients demonstrated a high incidence of OSA.Citation18 The increase in age has been attributed as an independent risk factor for OSA in various studies.Citation28,Citation29 The median age of our study population was 56.5 years which was low when compared to other studies done in non-dialysis patient.Citation19,Citation20,Citation28 The study population was screened using Berlin questionnaire to assess the prevalence of OSA and was found to be 28%. The incidence of OSA after sleep study in screened population was 88%. Ramachandran et al. and Sharma et al. concluded that Berlin questionnaire has better sensitivity and specificity than Epworth sleepiness scale and hence Berlin questionnaire was used as a screening tool to identify the prevalence of OSA which is being concurred by this study.Citation23,Citation30
We stratified our study population into two groups with male preponderance of 68%. Bixler et al. observed that OSA is more prevalent in male population as in our study.Citation31,Citation32 The mean BMI in our study group was 25.244 kg/m2 which was over weight as per Indian standards and was not suggestive of obesity as in other studies, thus excluding obesity as an individual risk factor for OSA.Citation24,Citation33,Citation34 Anemia was not a confounder as per CKD stage.Citation35 The mean SBP and DBP in the group 1 was 151.560 ± 13.328 mmHg and 90.520 ± 9.242 mmHg. Hypoalbuminemia was not a confounding factor as the mean value was 3.626 ± 0.2212 g/dL and 3.130 ± 0.1845 g/dL in the two groups. The mean SBP and DBP in group 2 was 155.040 ± 11.101 mmHg and 87.650 ± 7.228 mm Hg, respectively, and had not influenced the results of the study.Citation36
As reported in other studies we observed an increased risk of OSA with progression of CKD stage which was statistically significant (p < 0.05) This is consistent with the previous studies conducted by Sakaguchi et al., Morkou et al., Roumelioti et al., which shows similar results.Citation18–20
Conclusion
This study of OSA in non-dialysis CKD patients is unique, which revealed the high incidence and prevalence of OSA. OSA increases with progressive stage of CKD. However, further prospective longitudinal study with large sample sizes are needed with intervention in controlling progression of CKD, fluid electrolyte balance anemia, cardio vascular disease and targeted therapy with CPAP.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Fauci SA, Braunwald E, Kasper LD, et al. Harrison’s Principle of Internal Medicine. 18th ed. Chapter 280. McGraw Hill; 2308–2321
- Jha V, Garcia-Garcia G, Iseki K, et al. Chronic kidney disease: Global dimension and perspectives. Lancet. 2013;382(9888):260–272
- Ilangovan V, Abraham G. API Textbook of Medicine Section. Vol. 17. Jaypee Brothers Medical Publishers; 593–597
- Singh AK, Farag MKY, Mittal BV, et al. Epidemiology and risk factors of chronic kidney disease in India – Results from the SEEK (Screening and Early Evaluation of Kidney Disease) study. BMC Nephrol. 2013;14:114
- Guilleminault C, Tilkian A, Dement WC. The sleep apnea syndromes. Annu Rev Med. 976;27:465–484
- Octavian C, Loachimesu, Nancy A. Collop: Sleep disordered breathing. Neurologic Clinics 2012;30(4):1095–1136
- Young T. Peppard PE. Epidemiology of obstructive sleep apnea: A population health. WMJ. 2009;108(5):246–249
- Udwadia AF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep-disordered breathing and sleep apnea in middle-aged urban Indian men. Am J Respir Crit Care Med. 2004;169:168–73
- Sharma SK, Kumpawat S, Banga A, Goel A. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest. 2006;130:149–156
- Kuhlmann U, Becker HF, Birkhahn M, et al. Sleep-apnea in patients with end-stage renal disease and objective results. Clin Nephrol. 2000;53:460–466
- Jurado-Gamez B, Martin-Malo A, Alvarez-Lara MA, Munoz L, Cosano A, Aljama P. Sleep disorders are underdiagnosed in patients on maintenance hemodialysis. Nephron Clin Pract. 2007;105:c35–c42
- Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328:1230–1235
- Kimmel PL, Miller G, Mendelson WB. Sleep apnea syndrome in chronic renal disease. Am J Med. 1989;86:308–314
- Unruh M, Hartunian M, Chapman M, Jaber BL. Sleep quality and clinical correlates in patients on maintenance hemodialysis. Clin Nephrol. 2003;59(4):280–288
- Sharma SK, Ahluwalia G. Epidemiology of adult obstructive sleep apnea syndrome in India. Indian J Med Res. 2010;131:171–175
- Fletcher E. Obstructive sleep apnea and the kidney. J Am Soc Nephrol. 1993;4:1111–1121
- Rai M, Rustagi T, Rustagi S, Kholi R. Depression, insomnia and sleep apnea in patients on maintenance hemodialysis. Indian J Nephrol. 2011;21(4):223–229
- Roumelioti ME, Buysse DJ, Sanders MH, Strollo P, Newman AB, Unruh ML. Sleep-disordered breathing and excessive daytime sleepiness in chronic kidney disease and hemodialysis. Clin J Am Soc Nephrol. 2011;6:986–994
- Sakaguchi Y, Shoji T, Kawabata H. High prevalence of obstructive sleep apnea and its association with renal function among nondialysis chronic kidney disease patients in Japan: A cross-sectional study. Clin J Am Soc Nephrol. 2011;6:995–1000
- Markou N, Kanakaki M, Myrianthefs P, et al. Sleep-disordered breathing in nondialyzed patients with chronic renal failure. Lung. 2006;184:43–49
- Beecroft J, Duffin J, Pierratos A, Chan CT, McFarlane P, Hanly PJ. Enhanced chemo-responsiveness in patients with sleep apnea end end-stage renal disease. Eur Respir J. 2006;28:151–158
- Mavanur M, Sanders M, Unruh M. Sleep disordered breathing in patients with chronic kidney disease. Indian J Med Res. 2010;131:277–284
- Ramachandran SK, Josephs LA. A meta-analysis of clinical screening tests for obstructive sleep apnea. Anesthesiology. 2009;110(4):928–939
- Grunstien R, Wilcox I, Yang TS, et al. Snoring and sleep apnea in men: Associated with central obesity and hypertension. Int J Obes Realt Metab Disord. 1993;17(9):533–534
- Lam JCM, Sharma SK, Lam B. Obstructive sleep apnea: Definitions, epidemiology & natural history. Indian J Med Res. 2010;131:165–170
- The Report of an American Academy of Sleep Medicine Task Force. Sleep-related breathing disorders in adults: Recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;21:667–689
- Kushida CA, Littner MR, Morgenthaler T, et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep. 2005;28:499–521
- Ip MS, Lam B, Lauder IJ, et al. A community study of sleep disordered breathing in middle-aged Chinese men in Hong Kong. Chest. 2001;119:62–69
- Sharma SK, Kumpawat S, Banga A, Goel A. Prevalence and risk factors of obstructive sleep apnea syndrome in a population of Delhi, India. Chest. 2006;130(1):149–156
- Sharma SK, Vasudev C, Sinha S. Validation of the modified Berlin questionnaire to identify patients at risk for the obstructive sleep apnea syndrome. Indian J Med Res. 2006;124:281–290
- Bixler EO, Vgontas An, Ten HT, et al. Effects of age on sleep apnea in men: I prevalance and severity. AM J Respir Crit Care Med. 1998;157(1):144–148
- Bixler EO, Vgontas AN, Lin HM, et al. Prevalance of sleep disordered breathing in woemen: effects of gender. AM J Respir Crit Care Med. 2001;163(3 Pt 1):608–613
- Frey WC, Pilcher J. Obstructive sleep related breathing disorders in patients evaluated for bariatric surgery. Obes Surg. 2003;13(5):676–683
- Stradling JR, Crosby JH. Predictors and prevalence of obstructive sleep apnea and snoring in 1001 middle aged men. Thorax. 1991;46:85–90
- Jhamb M, Unruh ML. Volume overload as a mechanism for obstructive sleep apnea in CKD? Nephrol Dial Transplant. 2012;27:1291–1293
- Khaled AK, Sheena D, Nirav S, et al. Resistant hypertension and obstructive sleep apnea in the setting of kidney disease. J Hypertens. 2012;30(5):960–966