Abstract
The imbalance between organ demand and supply causes the increasing use of suboptimal donors. The aim of this study is to investigate the survival and allograft function of kidney transplantation from standard (SLD) and elderly living (ELD), standard criteria (SCDD) and expanded criteria deceased (ECDD) donors. All patients transplanted from 1997 to 2005 were investigated according to the donor characteristics. Data were collected retrospectively during the 83.4 ± 43.1 months of follow-up period. ELD was defined as donor age ≥60 years. ECDD was defined as UNOS criteria. A total of 458 patients were divided into four groups: SLD (n:191), ELD (n:67), SCDD (n:154), and ECDD (n:46). Seven-year death-censored graft survival in SLD, ELD, SCDD, and ECDD were 81.6%, 64.8%, 84.7%, and 68.3%, respectively (p = 0.003). The death-censored graft survival in ELD group was lower than in SLD (p = 0.007) and SCDD (p = 0.007) groups, while in ECDD group it was lower than in SCDD group (p = 0.026). Patient survival was similar. In ECDD group, 83% of total deaths occurred within the first 3 years, mainly due to infections (66.6%) (p < 0.05). Estimated glomerular filtration rate (eGFR) was lower in ELD (compared with SLD and SCDD); and ECDD (compared with SCDD) at last visit. In multivariate analysis, ELD, experience of an acute rejection episode and presence of delayed graft function were the independent predictors for death censored graft loss. Transplantation of a suboptimal kidney provides inferior graft survival and function. A higher number of deaths due to infection in the early post-transplant period in the ECDD group are noteworthy.
Introduction
Many end-stage renal failure patients want to have kidney transplants, in the hope of improving their quality of life. Transplant patients’ life satisfaction, physical and emotional well-being, and the rate of their ability to return to work improve after transplant. According to the data from USRDS, the life expectancy of an individual in the general population is 35.8 years. However, if these people are suffering from end stage renal failure, their life expectancy reduces to 9.7 years. Transplant patients fare better, with expected remaining lifetimes 75–80% (26.4 years) as long as those in the general population.Citation1 In addition, transplant can correct complications of uremia that cannot be reversed by dialysis, including anemia, peripheral neuropathy, autonomic neuropathy, and sexual dysfunction. In addition, compared to hemodialysis the long-term benefits of transplantation are more prominent.Citation2–4
Due to the increasing number of patients with end-stage renal failure, ideal donors cannot be found for every patient. Moreover, due to increasing demand for organs the uses of donors formerly called expanded criteria donors or suboptimal donors are becoming a necessity.Citation5 Transplants from expanded criteria or suboptimal donors have been shown to have better survival than the waiting list; however, survival is not as ideal as a transplant from an optimal donor.Citation6,Citation7 In this study we aimed to investigate the patient and graft outcome of kidney transplantation from the standard living donor (SLD), standard criteria deceased donors (SCDD), elderly living donor (ELD), and expanded criteria deceased donor (ECDD).
Materials and methods
Our study started with 465 patients who underwent organ transplantation at our center between 1997 and 2005. Seven patients were excluded from the study due to insufficient data. The clinical and demographic data (age, gender, primary kidney disease, number of transplants, cold ischemia time, haplotype match or mismatch count, pre-transplant blood transfusion rate, dialysis type and duration, whether it was a preemptive transplant or not, pre-transplant HBV and HCV status, whether the living donors were relatives, presence of delayed graft function) of the remaining 458 patients were obtained from patient files. Live donors’ ages and genders, and deceased donors’ ages, sex, causes of death, history of diabetes, and presence of hypertension or cardiovascular events were obtained from donor files.
Based on the UNOS definition, all deceased donors older than 60 years, or donors aged 50–59 years, who met two of the following criteria: (1) history of hypertension, (2) cerebrovascular accident as a cause of death and (3) final pre-procurement serum creatinine (SCr) level >1.5 mg/dL were classified as ECDDs.Citation6 Live donors above the age of 60 were defined as elderly living donor (ELD), deceased donors younger than 60 and who did not have any clinical event were defined as standard criteria deceased donors (SCDD), and live donors younger than 60 were defined as standard living donors (SLD).
Serum creatinine, proteinuria and estimated glomerular filtration rate (eGFR) using Modification of Diet in Renal Disease (MDRD) formulaCitation8 were recorded for patients who had a functional graft in the post-transplant 3rd and 5th years and in the last control. For deceased patients and patients who had post-transplant graft loss their last follow-up was recorded as the last entry. The final follow up of patients with functional grafts was done at the end of 2012. Thus, a minimum follow-up of 5 years was recorded.
Graft losses were examined in four categories. The early graft losses were defined as primary non-functionality, surgical complications, early irreversible rejection and thrombotic microangiopathy. Chronic graft loss was defined as chronic rejection, unspecified interstitial fibrosis and tubular atrophy (IFTA), BK nephropathy and other chronic infections. Recurrent glomerular disease was defined as a specific category. Finally, the fourth group consisted of unknown or other reasons of graft loss. The causes of death were categorized as follows: infection, cardiovascular events, malignancies, and unknown/other.
The immunosuppressive therapy varied over time due to long duration of the study period. Prior to 1999 primary immunosuppressive regimen consisted of corticosteroids, azathioprine, and cyclosporine. During that period, antithymocyte globulin (ATG) was used in the induction therapy in transplantation from deceased donors. Starting from 2001 mycophenolate mofetil was used instead of azathioprine. Cyclosporine was used in living donor transplants, and tacrolimus was used in deceased donor and living unrelated donor kidney transplants. Then, starting from 2002 IL-2 antagonists were used in living donor transplants and ATG was used in transplants from deceased donors.
Statistical methods
Data are reported as mean ± SD unless otherwise stated. Between-group comparisons were made with ANOVA tests, categorical variables were compared with chi-squared tests. Survival analysis was performed using the Kaplan–Meier method testing for statistical significance using the log-rank test. For independent predictors associated with overall and death censored graft survival, adjusted Cox regression analysis was performed including variables statistically significant in the univariate analysis. Statistical significance was defined as p < 0.05. All analyzes were performed using SPSS software version 13.0 (SPSS Inc., Chicago, IL).
Results
The mean age of the 458 patients from our study at the time of transplantation was 33 ± 10 years and 40% (n = 184) of them were female. Preemptive transplantation was performed in 38 patients. In others, the mean duration of dialysis before transplantation was 26 ± 30 (1–192) months. Twenty patients underwent re-transplantation. The average number of pre-transplant blood transfusions was 3 ± 7 units. The recipients were divided into four groups according to the donor type. In each group the number of patients for SLD, ELD, SCDD, and ECDD were 191, 67, 154, and 46, respectively. Approximately one-quarter of the study group (24.6%) consisted of non-ideal donors.
The demographic and clinical characteristics of groups according to the type of donors are shown in . We determined that recipients form the SLD group were younger compared to the ELD group (p < 0.001), and that the recipients from the ECDD group were mostly women. Incidence of repeat transplant was similar between groups. The frequency of preemptive transplantation was the highest in SLD group. In the deceased groups the duration of pre-transplantation dialysis was longer (p < 0.001). More women donors were observed in the living donor transplantation, while more men donors were observed in the deceased donor transplantation. Unrelated liver transplants were only seen in SLD group. One haplotype match was similar between SLD and ELD groups. The mismatched HLA antigen number was lower in the deceased donor groups compared to the SLD group (p < 0.001). The frequency of DGF was similar between deceased donor groups.
Table 1. Demographic and clinical characteristics of recipients and donors.
The mean follow-up time for all patients was 83.4 ± 43.1 (0–193) months, and in the ECDD group the follow-up period was significantly shorter. In the SCDD group, 45% of donor cause of death was traumatic brain death (traffic accident in majority), while in the ECDD group 75% of donor cause of death were brain deaths associated with cerebrovascular events.
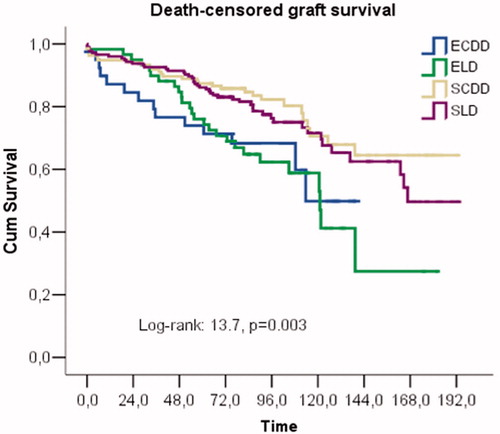
During the follow-up, graft loss occurred in 115 patients. Seven-year death-censored graft survival in SLD, ELD, SCDD, and ECDD were 81.6%, 64.8%, 84.7%, and 68.3%, respectively (log rank p = 0.003) (). The death-censored graft survival in the ELD group was significantly lower than in the SLD (p = 0.007) and SCDD (p = 0.007) groups, while in the ECDD group it was significantly lower than the SCDD group (p = 0.026).
The distribution of groups and details about causes and timing of the graft losses are shown in . We did not detect any significant differences between groups in terms of causes and timing of graft loss. However, although not statistically significant the graft loss in the ECDD group occurred earlier compared to other groups.
Table 2. Causes and timing for graft losses and recipient deaths.
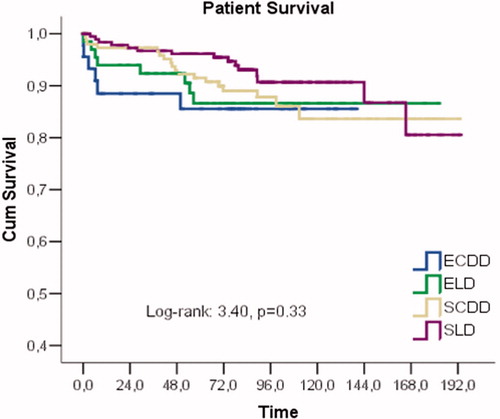
A total of 47 patients died. Seven-year patient survival in SLD, ELD, SCDD, and ECDD groups were 93.1%, 86.6%, 89.1%, and 85.5%, respectively (log rank: 0.333) (). The causes of deaths in 66.6% of the ECDD group were due to infections. The distribution of causes of deaths did not differ significantly between the groups (). However, in the ECDD group the post-transplant deaths occurred at a mean of 11 months and 83% of total deaths happened within the first 3 years (p < 0.05).
The incidence of acute rejection episode was 44.3% in the whole group. In SCDD group incidence of acute rejection was the lowest (29.2%), compared with SLD (54.9%), ELD (47.7%) and ECDD (45.6%) groups (p < 0.05). The serum creatinine, proteinuria, and eGFR values measured at the post-transplant 3 years, 5 years and at the time of the last control are shown in . At 3rd year, eGFR with MDRD in ELD group was significantly lower than SLD (p: 0.004) and SCDD (p < 0.001) groups, In ECDD group eGFR was significantly lower than SLD (p: 0.016) and ECDD (p < 0.001) groups. At 5th year, eGFR in ELD group was significantly lower than SLD (p: 0.003) and SCDD (p < 0.001) groups, in ECDD group eGFR was significantly lower than SLD (p: 0.008) and ECDD (p < 0.001) groups. At last follow up, eGFR was lower in ELD than SLD (p: 0.030) and SCDD (p < 0.001), while in ECDD was lower than SCDD (p: 0.010). Although spot urine protein/creatinine ratio was not significant among groups at 3rd and 5th years after transplantation, at last follow up it was significantly higher in ECDD group compared to SCDD (p: 0.005).
Table 3. Course of graft functions according to the donor groups.
To determine the independent predictors of death censored graft failure, Cox proportional hazard model was applied. When the clinically relevant variables (recipient age at transplantation, gender, dialysis vintage, number of mismatch, presence of delayed graft function, acute rejection and donor group) included into the model, it was found that ELD with reference to SLD (p: 0.001, HR: 2.270, CI: 1.380–3.735), experience of an acute rejection episode (p: 0.000, HR: 3.375, CI: 2.195–5.189) and presence of delayed graft function (p: 0.002, HR: 2.541, CI: 1.390–4.643) were the independent predictors for death censored graft loss.
Discussion
The increasing number of patients waiting for organs and limited number of potential resources pushes physicians to search for ways to improve their patient’s length and quality of life. In this context, one of the solutions is the use of expanded criteria for live or cadaveric donors. During our study period, 24.8% of live donor transplants and 23% of the deceased donors transplants could be described as non-ideal. In this study donor quality was found to be important in long-term graft survival and graft function. In addition, we found that the graft survival and graft function were worse in ELD and ECDD groups compared to standard live or deceased donors. There were no differences in terms of patient survival.
The effects of donor characteristics on graft prognosis have been investigated in previous studies and contradictory results have been reported. Some studies have reported that recipients of kidneys from ELD and ECDD have shown negative trend in terms of graft survival and/or graft function compared to recipients of the standard donor kidney. On the other hand some studies have found a similar pattern.
Stratta et al. found that graft and patient survival and morbidity were similar between ECDD and SCDD groups, moreover serum creatinine levels were similar at a mean of 18th month after transplantation.Citation9 In another study, it has been showed that older living donors provide excellent quality, moreover recipient’s serum creatinine was also similar at 2-year between transplants from young and older live donor.Citation10 In another study, the authors did not detect any difference between SCDD and ECDD groups in terms of graft survival; moreover, shorter waiting time on the cadaver waiting list has been shown to have a positive impact on patients and graft survival with a mean follow up of 3.5 years.Citation11
In a study comparing recipients of elderly living, standard deceased and young living donors, the authors reported similar patient survival, but poorer graft survival in elderly living donors. Therefore, transplantation of the kidney from an elderly living donor into a patient with a long life expectancy should be considered very carefully.Citation12 Noppakun et al. found that transplantation from older kidneys was associated with impaired graft function and proteinuria, and the impact on graft survival was noted particularly beyond 4 years after transplantation.Citation13 In a systematic review ECD kidneys were found to have worse graft survival than standard criteria donor kidneys.Citation14
In addition to clinical and co-morbidity characteristics of the donor, some studies added the kidney histology obtained from the implantation biopsies to the evaluation. The delayed graft function was found in the ECDD kidneys that had interstitial fibrosis and fibrous intimal thickening of Banff score 1 or higher during the pre-implant biopsy and it was indicated that these histologic findings may influence the graft’s long-term survival.Citation15 In a center where pre-implant biopsy has become routine in ECDD and where they do not implant kidneys with disturbed histology, physicians did not detect any difference between ECDD and SCDD in terms of graft survival.Citation16 Optimal ECDD should lead to acceptable glomerular filtration rate and histological changes in the kidney.Citation14
The reasons for these conflicting results might be the following: the cut-off value for age in those studies, the differences regarding the description of comorbidities in the donor, the extent to which the histology was affected at the time of the pre-implantation biopsy, and follow-up period after transplantation. In fact, the detection of negative effects of donors’ age and histologic injury at the time of transplantation on long-term post-transplant allograft function is not a surprising finding. Here, the main issue to be discussed is whether non-ideal kidney transplant provides more survival advantages to the recipient compared to patient staying on dialysis. In a pioneering study Ojo et al. compared patients who received non-ideal organs with patients who remained in the waiting list and reported that non-ideal donor transplantations provided more advantages.Citation7 In our study, 7-year death censored graft survival and patient survival rates were 64.8% and 86.6% for ELD and 68.3% and 85.5% for ECDD. These obtained ratios are still higher than the ratios obtained with current dialysis treatment. Therefore, rather than focusing on the supremacy of non-ideal transplantations over dialysis we need to focus on the issues such as how to provide longer survival of transplanted kidneys with reduced nephron mass.
Previous studies have generally focused on graft survival and function. In our study we compared both patient survival and causes of death between the groups. We did not detect any difference between the four groups in terms of patient survival rates. However, the deaths were literally more frequent in the early post-transplantation period in the ECDD group and the majority of deaths were infection related. This situation can be explained with the presence of delayed graft function, graft function remaining at suboptimal level, and long periods of hospitalization of those patients. Therefore, patients who underwent extended criteria donor transplantations should undergo infection prophylaxis during post-transplant follow-up and physicians should be watchful for early diagnosis of infection.
There are some limitations of our study. The patient characteristics differ between groups due to the retrospective nature of the study and because we included both living and deceased donor transplants. Recipient's age, pre-transplant dialysis duration, the number of mismatched antigens, and the presence of cold ischemia naturally lead to variation between groups. We tried to partially overcome this problem by performing multivariate analyses. Deceased donor transplants accounted for 43.6% of our study group. In our country, the majority of transplants are living donor transplants and especially during our study period there were no old-for-old programs available. Furthermore, immunosuppressive therapy showed variation among patients over the follow-up years. There are now studies that recommend calcineurin inhibitor sparing regimens as available options for ECDD and ELD groups.Citation17,Citation18
In conclusion, transplantation of a kidney that has only sustained structural damage due to age or comorbid conditions associated with age provides inferior graft survival and function compared to the ideal kidney. Although, there were no differences between the groups in terms of patient survival, a higher number of deaths due to infection in the early post-transplant period in the ECCD group are noteworthy. Therefore, efforts should focus on prolonging the survival of non-ideal kidneys and on reducing premature deaths.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- United States Renal Data System Annual Data Report 2013. Available at: http://www.usrds.org/2013/view/v2_05.aspx. Accessed July 4, 2014
- Suthanthiran M, Strom TB. Renal transplantation. N Engl J Med. 1994;331(6):365–376
- Schnuelle P, Lorenz D, Trede M, Van Der Woude FJ. Impact of renal cadaveric transplantation on survival in end-stage renal failure: Evidence for reduced mortality risk compared with hemodialysis during long-term follow up. J Am Soc Nephrol. 1998;9(11):2135–2141
- Port FK, Wolfe RA, Mauger EA, Berling DP, Jiang K. Comparison of survival probabilities for dialysis patients vs. cadaveric renal transplant recipients. JAMA. 1993;270(11):1339–1343
- Ratner LE, Kraus E, Magnuson T, Bender JS. Transplantation of kidneys from expanded criteria donors. Surgery. 1996;119(4):372–377
- Metzger RA, Delmonico FL, Feng S, et al. Expanded criteria donors for kidney transplantation. Am J Trans. 2003;3(suppl. 4):114–125
- Ojo AO, Hanson JA, Meier-Kriesche H, et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-list transplant candidates. J Am Soc Nephrol. 2001;12(3):589–597
- Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470
- Stratta RJ, Rohr MS, Sundberg AK, et al. Increased kidney transplantation utilizing expanded criteria deceased organ donors with results comparable to standard criteria donor transplant. Ann Surg. 2004;239(5):688–695 ; discussion 695–697
- Johnson SR, Khwaja K, Pavlakis K, Monaco AP, Hanto DW. Older living donors provide excellent quality kidneys: A single center experience (older living donors). Clin Transplant. 2005;19(5):600–606
- Carrier M, Lize JF, Quebec-transplant programs. Impact of expanded criteria donors on outcomes of recipients after kidney transplantation. Transplant Proc. 2012;44(7):2227–2230
- Lim WH, Clayton P, Wong G, et al. Outcomes of kidney transplantation from older living donors. Transplantation. 2013;95(1):106–113
- Noppakun K, Cosio FG, Dean PG, Taler SJ, Wauters R, Grande JP. Living donor age and kidney transplant outcomes. Am J Transplant. 2011;11(6):1279–1286
- Pasccual J, Zamora J, Pirsch JD. A systematic review of kidney transplantation from expanded criteria donors. Am J Kidney Dis. 2008;52:553–586
- Balaz P, Rokosny S, Wohifahrtova M, et al. Identification of expanded-criteria donor kidney grafts at lower risk of delayed graft function. Transplantation. 2013;96(7):633–638
- Hofer J, Regele H, Böhmig GA, et al. Pre-implant biopsy predict outcome of single-kidney transplantation independent of clinical donor variables. Transplantation. 2014;97(4):426–432
- Pestana JO, Grinyo JM, Vanrenterghem Y, et al. Three-year outcomes from BENEFIT-EXT: A phase III study of belatacept versus cyclosporine in recipients of extended criteria donor kidneys. Am J Transplant. 2012;12(3):630–639
- Uslu A, Nart A, Taşlı FA, et al. Sirolimus-based triple immunsupression with antithymocyte globulin in expanded criteria donor kidney transplantation. Nephrology (Carlton). 2008;13(1):80–86