Abstract
Background and aim: Trendelenburg positioning (TP) is a common approach used during internal jugular vein (IJV) cannulation. No evidence indicates that TP significantly increases the cross-sectional area (CSA) of the IJV or decreases the overlap between the carotid artery (CA) and the IJV in dialysis patients. The primary aim of this study was to investigate the effects of the TP on the CSA of the right IJV and on its relationship to the CA. Methods: Thirty-seven consecutive hemodialysis patients older than 18 years of age were enrolled. We measured the CSA of the right IJV and overlap rate (at end-expiration at the level of the cricoid cartilage) between the CA and the IJV in two positions: State 0, table flat (no tilt), with the patient in the supine position; State T, in which the operating table was tilted to 15° of TP. Results: Data were collected for all of the 37 patients enrolled in the study. The change in CSA and overlap between the CA and the IJV from the supine to the TP was not significantly different. The CSA was paradoxically decreased in 11 of 37 patients when changed from State 0 to State T. Conclusions: TP does not significantly increase the CSA of the right IJV or decrease the overlap between the CA and the IJV in dialysis patients. In fact, in some patients, it reduces the CSA. Therefore, the use of the TP for IJV cannulation in dialysis patients can no longer be supported.
Introduction
Hemodialysis is the most frequently utilized therapy and the right internal jugular vein (IJV) is a commonly used cannulation site for central venous access in chronically dialyzed patients.Citation1,Citation2 The safe and successful placement of the central venous line correlates with the cross-sectional area (CSA) of the veins and the degree of overlap between the carotid artery (CA) and the IJV.Citation3–5 Successful placement of an IJV catheter is difficult in patients whose veins have small CSA.Citation2,Citation4 Inadvertent CA puncture is seen in up to 21%Citation6 of patients during IJV catheterization and may result in serious morbidity, and even mortality, in high-risk hemodialysis patients.Citation7,Citation8 Ultrasound guidance has been recommended to increase the success of IJV catheterization and decrease the incidence of complications but it is not always routinely used.Citation4 Thus, it would be of great interest to clinicians if one approach could be shown to increase the CSA and decrease the overlap with the CA in order to improve patient safety.
Trendelenburg positioning (TP) is a common approach for gaining access to the IJV.Citation8,Citation9 No evidence indicates that changing the body position of dialysis patients to the TP significantly increases the CSA of the IJV or decreases the overlap between the CA and the IJV. Recently, Wu et al.Citation2 conducted an ultrasound study to investigate the efficacy of the use of the TP during tunneled dialysis catheter insertion via the right IJV in patients with chronic kidney disease. The overlap rate of the CA and the IJV was not evaluated in their study. They found that, in contrast to healthy volunteers, there was no increase in the CSA of the right IJV when dialysis patients were in the TP. Wu et al.Citation2 suggest that the use of the TP for dialysis catheter insertion may not be appropriate and should not be encouraged, although it continues to be widely used for central venous catheterization in chronically dialyzed patients. However, this requires further evaluation before a final conclusion can be made.
The primary aim of this study was to investigate the effects of the TP on the CSA of the IJV and the overlap rate between the CA and the right IJV in dialysis patients.
Methods
The study protocol was approved by the Institutional Review Board of the Medical Faculty, and written informed consents were obtained from all the participants prior to the start of the study. Between July 2013 and December 2013, a total of 37 consecutive hemodialysis patients older than 18 years of age were enrolled. All the ultrasound examinations were performed by the same radiologist (A.N.) in order to maintain consistency. Patients with a history of prior right IJV cannulation or neck surgery were not included in this study. Patients with stenotic or thrombosed right IJVs were also excluded from the study.
The right IJV and its relationship with the CA were ultrasonographically measured using a 13.5-MHz linear array transducer (Acuson, Antares, Siemens). Ultrasound images of the IJVs were obtained in a transverse orientation at the cricoid level. The IJVs were depicted in the middle of the ultrasound image. Probe pressure was kept as low as possible to avoid compression of the IJV.
All of the patients were positioned with their neck in extension and head rotated left at ∼20–30°. Patients were studied in State 0, table flat (no tilt), with the patients in the supine position, and State T, in which the operating table was tilted 15° to a TP. A goniometer was used to measure the tilt angle of the table from the horizontal plane. After images were obtained for State 0, the patients were positioned to State T. Images of the right IJV were obtained at most 1 min after changing the patient’s body position to the 15° TP. The images for each state were obtained at end-expiration at the level of the cricoid cartilage. After freezing the real-time image, the circumference of the IJVs was delineated using an electronic marker, and the CSA of the IJVs were calculated using a program pre-loaded into the ultrasound unit.
The following measurements were carried out at each position:
the CSA of the right IJV,
the degree of overlap between the IJV and the CA,
the transverse and anteroposterior diameters of the right IJV and
the margin of safety.
Demographic data of the studied patients were also collected.
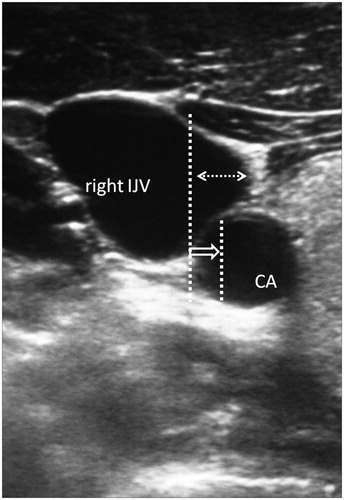
The overlap between the IJV and the CA was categorized on the basis of the percentage of overlap: with (1) being an overlap <25% of the diameter of the CA and (2) being an overlap of ≥25% of the diameter of the CA ().
Figure 1. Ultrasound image of the right IJV and relationship with CA. Interrupted white arrow represents the overlap between CA and IJV. Short arrow shows 25% diameter of CA and long arrow shows 50% diameter of CA. IJV, internal jugular vein; CA, carotid artery.
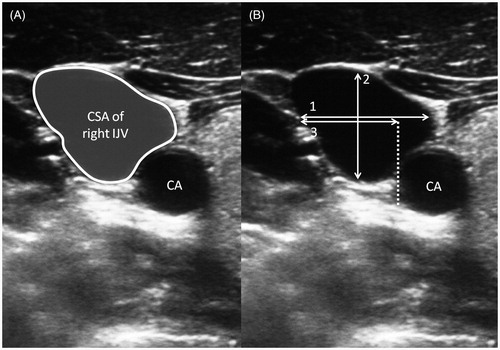
The transverse and anteroposterior diameters of the right IJV were measured by drawing a line between the furthest two points of the vein wall in the transverse and anteroposterior planes. The margin of safety was defined as the distance from the lateral-most border of the right IJV and the lateral-most border of the CA at which the right IJV could be punctured without contacting the CA ().
Figure 2. Ultrasound images of the right IJV and relationship with CA. (A) Cross-sectional area of right IJV. (B) (1) Transverse diameter of IJV, (2) A-P diameter of IJV and (3) safety margin. CA, carotid artery; A-P, anteroposterior; IJV, internal jugular vein.
Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL). The data were tested for normality using the Kolmogorov–Smirnov test. The paired sample t-test was used to compare the diameters and CSA changes between the State 0 and the State T in all the patients. Categorical data were analyzed using the McNemar test. A p value <0.05 was considered statistically significant.
Results
Data were collected for all of the 37 patients (25 male and 12 female) enrolled in the study. No stenotic or thrombosed right IJVs were noted during the ultrasound measurements. Age, gender and body mass index (BMI) of the patients were recorded. Chronic renal failure was associated with hypertension in 16 cases, diabetes mellitus in seven cases and coronary heart disease in five cases. The characteristics of the patients are shown in . The study measurements are summarized in .
Table 1. Characteristics of 37 dialysis patients.
Table 2. Outcome measurements in the State 0 and State T.
The CSA of the right IJV, the degree of overlap between the right IJV and the CA, the transverse and anteroposterior diameters of the right IJV, and the margin of safety from the supine to the TP was not significantly different. The CSA was paradoxically decreased in 11 of 37 patients (8 of 11 were male).
Discussion
This study has three major findings. First, the TP did not increase the CSA of the right IJV in dialysis patients. Second, TP may have actually made the vein smaller in a subset of subjects. Finally, there were no significant differences between the positions with respect to the overlap rate between the CA and the right IJV.
Hemodialysis catheterization through the IJV is widely used for mid- to long-term vascular access.Citation2,Citation7 Use of the right IJV is more favorable than the left IJV because of its direct route to the superior vena cava, its position being far from the pleura and the absence of a thoracic duct in the right side of the chest.Citation2–4 In addition, the right IJV has a much wider diameter and runs more superficially than the left IJV, and anatomical variations of the left IJV may partly account for the difficulty in achieving successful cannulation of the left IJV in certain patients.Citation10 Hemodialysis patients generally have an increased risk of catheter complications because of impaired hemostasis secondary to platelet dysfunction and repeated catheterization of the IJVs with large-bore dialysis catheters.Citation11,Citation12 Vascular perforation and rupture may complicate catheter insertion, especially in older patients with multiple vascular problems due to thrombotic complications and decreased elasticity of the vessels.Citation13 Therefore, IJV catheterization in patients with chronic renal failure requires more patience and the avoidance of CA puncture is an absolute necessity.Citation3,Citation11
The TP is the elevation of the pelvis above the horizontal plane in the supine position. A survey of 140 physicians revealed that 91% choose the TP when inserting a jugular venous catheter.Citation14 It is assumed that body inversion produces a shifting of blood from the legs and abdomen toward the heart by gravitational displacement. This shifting leads to an increase of venous return to the heart and hence, an increase in the CSA of the IJV, left ventricular end-diastolic volume and cardiac output.Citation2,Citation9,Citation15 One meta-analysis concluded that cardiac output increased by 9% at 1 min of TP. This effect persisted after the first minute by 4% and returned to baseline 10 min after equilibrium by autoregulation.Citation15 Furthermore, TP has potentially deleterious effects, especially in critically ill patients.Citation9 Increased work of breathing, decreased lung compliance, cardiac ischemia, raised intracerebral and intraocular pressures, decreased cerebral perfusion pressure, cardiac dysrhythmias, hypoxemia, and subjective distress and discomfort have all been reported.Citation9,Citation15–17
Most studies which evaluate the effects of the TP on the CSA of the IJV have been performed on healthy subjects, surgical patients or intensive care patients.Citation9,Citation18–22 The effect of the TP on the CSA of the IJV in dialysis patients is largely unknown. To the best of our knowledge, this is the second study in English literature after than Wu et al. study,Citation2 of the responsiveness of jugular veins to TP in dialysis patients. Wu et al.Citation2 reported that, in contrast to healthy volunteers, the calculated CSA of the right IJV was not significantly higher in the TP, when compared with the supine position, in dialysis patients. Our findings are consistent with the Wu et al.Citation2 study and support its conclusion.
Abnormalities of cardiac structure and function and abnormalities in cardiovascular autonomic regulation are closely related to morphological and characteristic alterations of cardiovascular vessels. These factors are well documented in chronic dialysis patients.Citation2,Citation23–25 Anemia, left ventricular hypertrophy, diastolic dysfunction and vascular dysfunction are all the characteristic manifestations in dialysis patients. An increasing number of older dialysis patients with diabetes mellitus and autonomic neuropathy caused by uremic poisoning of the baroreceptorsCitation25–27 may stimulates morbidity of autonomic disorder in dialysis patients. Stimulation of the sympathetic nervous system seems to be the mechanism that is likely to cause cardiovascular complications, including sudden cardiac death, in chronically dialyzed patients. It is observed in both asymptomatic patients and in those diagnosed with cardiac disease.Citation24 Any of those cardiac abnormalities in dialysis patients may inhibit the desired engorgement of the IJV in the TP. To clarify which is the main cause, further studies that evaluate the relationship between CSA and vascular dysfunction, autonomic dysfunction or structural dysfunction will be required. Furthermore, the TP may affect both cardiac structure and cardiac autonomic function.Citation9 In other words, use of the TP in dialysis patients during IJV catheterization may worsen their clinical condition.Citation2,Citation9
In this study, we also found that TP paradoxically made the IJV vein smaller in 11 of 37 dialysis patients. This may reduce the safety or success of cannulation and may increase the risk of air embolism occurring during the procedure. A similar finding was observed in a study by Nassar et al.Citation9 which found that the TP actually made the vein smaller in 9 of 51 subjects. Hence, clinicians ought to keep in mind that the TP may predictably decrease the CSA of the IJV in dialysis patients and may also increase the risk of air embolism occurring during the procedure.
The factors predicting the effects of TP on the CSA of the IJV are largely unknown. A recently published study conducted by Nassar et al.Citation9 compared the CSA of the IJV in the TP, supine and reverse TP in 51 intensive care unit (ICU) patients (without respect to any specific diagnosis). They demonstrated that moving patients from supine to the TP increased the CSA by only 17%. Similar findings were reported in another study conducted by Modeliar et al.Citation24 who found that the TP increased the mean CSA by only 15% in 60 ICU patients. Maratea et al.Citation28 evaluated the extent of change of the CSA of the right IJV in response to TP in anesthetized patients and its predictive factors. They showed that right IJV dilation in response to TP was only significantly different in male patients. All of the other factors considered, including body-surface area, central venous pressure, type of surgery and ejection fraction did not show any correlation with the degree of right IJV CSA change. Most of the patients in our study were male (70%), yet in contrast to the result of Maratea et al., our patients had similar CSAs in the supine and TP. Moreover, in our study, 8 of the 11 patients whose CSA was paradoxically smaller in the TP were male.
The avoidance of CA puncture during IJV cannulation is correlated with the overlap rate between the CA and the IJV, and this provides one of the most important points for reducing CA puncture-related complications.Citation3,Citation4,Citation29 When the head is rotated away from the midline, the IJV becomes more directly anterior to the CA, resulting in a greater overlap of the IJV and the CA.Citation10 Therefore, excessive left rotation should be avoided to minimize the risk of unintentional CA puncture during right IJV cannulation. In the present study, each patient’s head was positioned with the head rotated left at ∼20–30°. According to our review of the literature, the effects of TP on the overlap between the CA and the IJV have not yet been evaluated. The patients in our study did not show significant changes in overlap between the CA and the IJV when placed in the TP. The transverse diameter, the AP diameter, and the margin of safety were similar for both the supine and TP.
This study has several limitations. We studied consecutive subjects with chronic renal failure who required IJV cannulation. This patient population presents with multiple comorbidities which can alter the normal function of blood vessels. These include cardiac dysfunction, autonomic dysfunction, volemic status and concurrent drugs used in these patients, none of which were evaluated before measurements were taken. Detailed cardiac function profile of the patients such as echocardiographic information was not evaluated in this study. Another limitation is that we obtained the images of the IJV after at most 1 min following the change of the patient’s body position from supine to 15° TP. Although the maximum effect of the TP is seen in the first minutes in healthy volunteers, further studies should be carried out to determine if greater changes occur following a longer period in the TP. In this study, measurements were obtained in only 15° Trendelenburg for state T. Although the angle of Trendelenburg has not been shown to affect the CSA of the IJVCitation30 in patients without chronic kidney failure, further studies with different angles should be done in dialysis patients. A final limitation is that ultrasound measurements can be operator-dependent, so errors in measurement cannot be excluded.
In conclusion, by studying the ultrasound images of the right IJV of dialysis patients, we determined that the TP changes neither the CSA of the right IJV nor the overlap rate between the CA and the IJV. In fact, the use of the TP for IJV cannulation may actually decrease the CSA and increase the risk of complications. Therefore, the TP can no longer be supported for IJV cannulation without ultrasound guidance.
Declaration of interest
The authors declare that they do not have any conflict of interest.
References
- Koroglu M, Demir M, Koroglu BK, et al. Percutaneous placement of central venous catheters: Comparing the anatomical landmark method with the radiologically guided technique for central venous catheterization through the internal jugular vein in emergent hemodialysis patients. Acta Radiol. 2006;47:43–47
- Wu H-L, Ting C-K, Chen C-Y, et al. No enlargement of the right internal jugular vein of the dialysis patients in the Trendelenburgposition. J Chin Med Assoc. 2013;76:401–406
- Apiliogullari B, Kara I, Apiliogullari S, Arun O, Saltali A, Celik JB. Is a neutral head position as effective as head rotation during landmark-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. J Cardiothorac Vasc Anesth. 2012;26:985–988
- Massimo L, Matteo S, Paolo C, et al. Is a neutral head position safer than 45-degree neck rotation during ultrasound-guided internal jugular vein cannulation? Results of a randomized controlled clinical trial. Anesth Analg. 2012;114:777–784
- Manikappa S, Cokis C. Assessment of internal diameter and cross-sectional area of right internal jugular vein pre-induction and post-intubation. Anaesth Intensive Care. 2005;33:381–383
- Feller-Kopman D. Ultrasound-guided internal jugular access: A proposed standardized approach and implications for training and practice. Chest. 2007;132:302–309
- Lee Y-M, Kim H-J, Lee J-E, et al. Cardiac tamponade following insertion of an internal jugular vein catheter for hemodialysis. Clin Nephrol. 2009;72:220–223
- Sayani R, Anwar M, Tanveer-ul-Haq, Al-Qamari N, Bilal MA. Outcome of radiologically placed tunneled haemodialysis catheters. J Coll Physicians Surg Pak. 2013;23:837–841
- Nassar B, Deol GR, Ashby A, Collett N, Schmidt GA. Trendelenburg position does not increase cross-sectional area of the internal jugular vein predictably. Chest. 2013;144:177–182
- Ozbek S, Apiliogullari S, Kıvrak AS, Kara I, Saltali AO. Relationship between the right internal jugular vein and carotid artery at ipsilateral head rotation. Ren Fail. 2013;35:761–765
- Ishizuka M, Nagata H, Takagi K, Kubota K. Right internal jugular vein is recommended for central venous catheterization. J Invest Surg. 2010;23:110–114
- Bahcebasi S, Kocyigit I, Akyol L, et al. Carotid-jugular arteriovenous fistula and cerebrovascular infarct: A case report of an iatrogenic complication following internal jugular vein catheterization. Hemodial Int. 2011;15:284–287
- Lin BS, Huang TP, Tang GJ, Tarng DC, Kong CW. Ultrasound-guided catheterization of the internal jugular vein for dialysis vascular access in uremic patients. Nephron. 1998;78:423–428
- Aydin Z, Batu A, Gursu M, et al. Perforation of the left brachiocephalic vein secondary to central venous catheterization. Turk Neph Dial Transpl. 2010;19:130–133
- Bellazzini MA, Rankin PM, Gangnon RE, Bjoernsen LP. Ultrasound validation of maneuvers to increase internal jugular vein cross-sectional area and decrease compressibility. Am J Emerg Med. 2009;27:454–459
- Marcus HE, Bonkat E, Dagtekin O, et al. The impact of Trendelenburg position and positive end-expiraory pressure on internal jugular cross sectional area. Anesth Analg. 2010;111:432–436
- Lobato EB, Florete OG Jr, Paige GB, Morey TE. Cross-sectional area and intravascular pressure of the right internal jugular vein during anesthesia: Effects of Trendelenburg position, positive intrathoracic pressure, and hepatic compression. J Clin Anesth. 1998;10:1–5
- Lewin MR1, Stein J, Wang R, et al. Humming is as effective as Valsalva’s maneuver and Trendelenburg’s position for ultrasonographic visualization of the jugular venous system and common femoral veins. Ann Emerg Med. 2007;50:73–77
- Kim JT, Kim HS, Lim YJ, et al. The influence of passive leg elevation on the cross-sectional area of the internal jugular vein and the subclavian vein in awake adults. Anaesth Intensive Care. 2008;36:65–68
- Ely EW, Hite RD, Baker AM, Johnson MM, Bowton DL, Haponik EF. Venous air embolism from central venous catheterization: A need for increased physician awareness. Crit Care Med. 1999;27:2113–2117
- Geerts BF, van den Bergh L, Stijnen T, Aarts LP, Jansen JR. Comprehensive review: Is it better to use the Trendelenburg position or passive leg raising for the initial treatment of hypovolemia? J Clin Anesth. 2012;24:668–674
- Fahy BG, Barnas GM, Nagle SE, Flowers JL, Njoku MJ, Agarwal M. Effects of Trendelenburg and reverse Trendelenburg postures on lung and chest wall mechanics. J Clin Anesth. 1996;8:236–244
- Ford DR, Witting MD, Vora MV, Sommerkamp SK, Euerle BD. No effect of Valsalva maneuver or Trendelenburg angle on axillary vein size. J Emerg Med. 2013;45:452–457
- Modeliar SS, Sevestre MA, De Cagny B, Slama M. Ultrasound evaluation of central veinsin the intensive care unit: Effects of dynamic manoeuvres. Intensive Care Med. 2008;34:333–338
- Whalley GA, Marwick TH, Doughty RN, et al. Effect of early initiation of dialysis on cardiac structure and function: Results from the echo substudy of the IDEAL trial. Am J Kidney Dis. 2013;61:262–270
- Chrapko BE, Jaroszyński AJ, Głowniak A, Bednarek-Skublewska A, Załuska W, Ksiażek A. Iodine-123 metaiodobenzylguanidine myocardial imaging in haemodialysed patients asymptomatic for coronary artery disease: A preliminary report. Nucl Med Commun. 2011;32:515–521
- Okano K, Tsuruta Y, Yamashita T, Echida Y, Kabaya T, Nitta K. Cardiovascular autonomic neuropathy studied by a laser-Doppler blood flowmeter in hemodialysis patients. Intern Med. 2010;49:2669–2675
- Maratea E, Castillo-Pedraza C, Cooper L, Olivera H, Gologorsky E. Factors predictive of right internal jugular vein cross-sectional area change in response to Trendelenburg positioning. World J Cardiovasc Surg. 2013;3:27–30
- Rostand SG, Brunzell JD, Cannon RO 3rd, Victor RG. Cardiovascular complications in renal failure. J Am Soc Nephrol. 1992;2:1053–1062
- Clenaghan S, McLaughlin RE, Martyn C, McGovern S, Bowra J. Relationship between Trendelenburg tilt and internal jugular vein diameter. Emerg Med J. 2005;22:867–868

