Abstract
Objective: The objective of this study is to compare the catheter-related complications as well as catheter survival between laparoscopic and traditional surgery in peritoneal dialysis catheter insertion. Results: Five randomized controlled trials and 11 cohort studies were identified. Meta-analysis showed laparoscopic catheter is superior to traditional surgery in terms of controlling catheter migration (OR 0.17, 95% CI 0.08–0.33; p < 0.00001) and catheter survival rate (1-year survival rate: OR 3.05, 95% CI 1.72–5.41, p = 0.0001; 2-year survival rate: OR 2. 07, 95% CI 1.29–3.33, p = 0.0001), but slightly increases the risk of bleeding (OR 2.13, 95% CI 1.07–4.23, p = 0.03). The two groups were not significantly different in other catheter-related complications. As regards the quality of the analysis, only the migration analysis ranked A-level, while the rest fell into Class B or C. The overall research quality was moderate. Conclusion: Laparoscopic surgery is superior to traditional surgery on reducing catheter migration and prolonging catheter survival rate according to our analysis.
Peritoneal dialysis (PD) is one of the basic renal replacement therapies. Comparing with hemodialysis, PD has more advantages in preserving residual renal function, clearing middle molecules, and reducing cardiovascular events.Citation1 Peritoneal dialysis catheter is the lifeline of the patients, many patients cannot benefit from PD due to a series of catheter-related complications such as in- and outflow obstruction, leakage, and catheter migration. Studies have found that the insertion technique may influence the function of PD catheters.Citation2–17 In clinical practice, peritoneal dialysis catheter (PDC) insertion is most commonly performed via traditional (open) or laparoscopic surgery. However, the optimal approach of PDC insertion is still under debate. Öğünç et al.Citation14 reported that laparoscopic approach had an advantage in reducing peritonitis in a small observational study,Citation8 while Qiao came to the opposite conclusion.Citation14
In recent years, PD has been popularized on a grand scale in China. Several centers have performed observational studies or RCTs on this topic, collecting a mass of primary data.Citation12–17 In this article, we conducted a systematic analysis based on both English and Chinese literature to obtain a comprehensive understanding of these two insertion technique in terms of complications and catheter survival.
Materials and methods
Searching strategy
We searched Pubmed, Elsevier Sciencedirect, Cochrane Library, Springer as well as CNKI by using the keywords “peritoneal dialysis”, “laparoscopic", “laparoscopy", “peritoneal dialysis” without language restriction. The search was performed for articles published up to 2 September 2014.
Including and excluding criteria
We included full-text articles following PICOS principle. This principle includes (1) specific patients(P) and here we chose those with end-stage renal disease (ESRD) who need dialysis treatment, (2) specific intervention(I) and we chose PDC insertion by laparoscopic surgery, (3) specific comparison(C) and we chose PDC insertion by open surgery, (4) specific outcome(O) and we chose catheter-related complications as well as catheter survival, and (5) specific types of study(S), in this article, we chose randomized controlled studies as well as observational studies for few RCTs on this subject had been published. We excluded the article if involving the same sample or not in conformity with the above principle.
Literature screening
A supervisor (Lu): Two steps were performed by two independent researchers (Qiao and Zhou), namely initial and the second screening. In step 1, researchers read the title and abstract of each searched literature to determine the relevance. Reviews, case-reports, letters, and other types of studies were excluded during the prescreening, so were studies concerning patients without ESRD. In step 2, full-text reading was performed by the researchers and studies not up to PICOS principle were excluded. Particularly, another study by Crabtree was excluded for involving the same sample. An experienced supervisor (Lu) leads a discussion if there was controversy.
Outcome measures
We extracted the following information: (1) perforation; (2) bleeding; (3) peritonitis and skin or tunnel infection; (4) catheter migration; (5) catheter obstruction; (6) leakage, including early and late leakage; (7) hernia; and (8) PD catheter survival.
Quality assessment
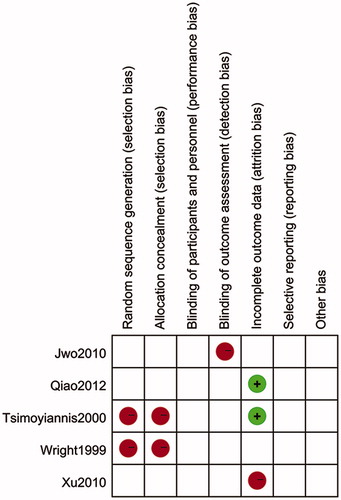
Randomized controlled trials were accessed by using criteria for evaluating the risk of bias offered by Cochrane Collaboration.Citation18 The assessing items consist of sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other potential sources of bias.
As all observational studies in the present analysis included were cohort studies, we adopted “Newcastle–Ottawa scale” (NOS) evaluation criteria for cohort studies, which comprise the study of choice (four items, four points), group comparability (one item, two points), and outcome measures (three items, three points), a total of nine points.Citation19
Statistical analysis
We performed the meta-analysis by using RevMan5.3 software (Revman International, Inc., New York, NY) provided by The Cochrane Collaboration. Heterogeneity between studies was tested by I2 statistics. For homogeneous studies, we adopted fixed effects model and the Mantel–Haenszel method for calculating. While for a smaller event rates, as in the comparison of the incidence of perforation and other issues, we used the Peto method. If the studies had significant heterogeneity, the random effects model and DL method were used. p < 0.05 was considered statistically significant. For dichotomous outcomes, we reported results as odds ratio (OR), while reporting continuous outcomes, weighted mean difference (WMD) was used. Forest maps were drawn based on the results. Finally, we assessed the quality of each conclusion by the GRADE tool (Tajima Tool Corporation, Torrance, CA). The software we used was GRADEprofeler3.6 (Tajima Tool Corporation, Torrance, CA). While grading the results, we treated the results as obtained by cohort studies for the sake of caution.
Results
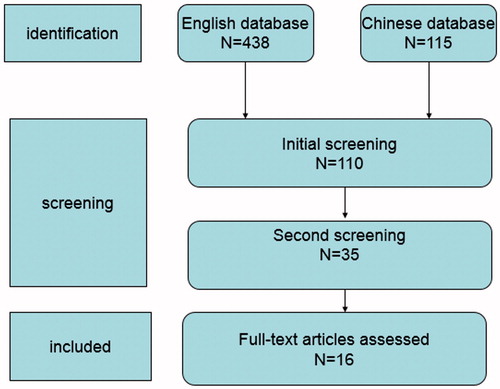
We found 553 papers after initial search, and then after the initial and second screening, as well as group discussion, 16 papers were enrolled in the final analysis, including five randomized controlled trials and 11 cohort studies.Citation2–17 The PRISMA flow diagram for systematic reviews is drawn in . One publication (by Crabtree et al. 2005) was excluded for describing patients that were already reported in another paper in 2000 by the same group.
Study quality
Generally speaking, the randomized controlled trials were of medium quality, as shown in .Citation5,Citation10,Citation11,Citation14,Citation16 While by NOS evaluation criteria, the Cohort studies scored an average of 6.2 points, with a medium quality.Citation2–4,Citation6–9,Citation12,Citation13,Citation15,Citation17
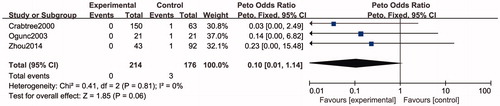
Perforation and bleeding
Perforation is defined as perforation of bowel or bladder. For perforation, a total of three researches involving 390 patients were included in the analysis.Citation2,Citation8,Citation15 Because of the low incidence of perforation, we used the Peto method in hypothesis testing. The results indicated that there is no significant difference in the incidence of perforation (OR 0.10, 95% CI 0.01–1.14, p = 0.06). The forest plot of this analysis is shown in .
Figure 3. Forest plot. Odds ratios of the incidence of performation between laparoscopic and traditional PD catheter insertion. CI: confidence interval. Experimental: laparoscopic surgery, control: traditional surgery.
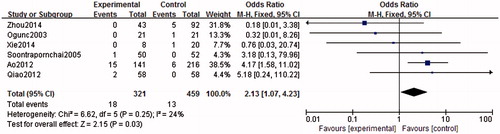
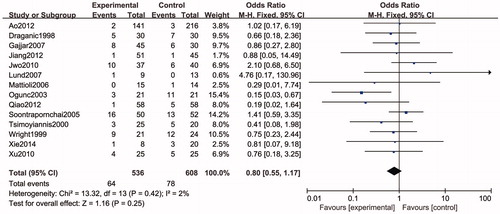
With a total of 780 patients from six studies, our result showed there is a higher risk of bleeding in laparoscopic method than traditional surgery (OR 2.13, 95% CI 1.07–4.23, p = 0.03).Citation8,Citation9,Citation12,Citation14,Citation15,Citation17 The forest plot of this analysis is shown in .
Peritonitis and tunnel or skin infections
Fourteen studies involving a total of 1144 cases of patients described the incidence of peritonitis, the result showed that laparoscopic surgery and traditional catheterization have no significant difference in the incidence of peritonitis (OR 0.80, 95% CI 0.55–1.17, p = 0.25).Citation3–11,Citation13,Citation14,Citation16,Citation17 The forest plot of this analysis is shown in .
Figure 5. Forest plot. Odds ratios of the incidence of peritonitis between laparoscopic and traditional PD catheter insertion. CI: confidence interval. Experimental: laparoscopic surgery, control: traditional surgery.
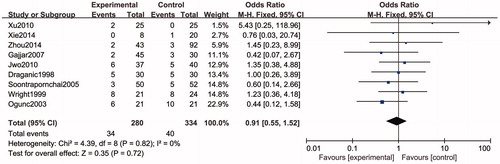
The analysis for skin or tunnel infection involved a total of 614 cases reported by nine papers. The result showed that there is no statistically significant difference between the two groups (OR 0.91, 95% CI 0.55–1.52, p = 0.72),Citation3–5,Citation8,Citation9,Citation11,Citation15–17 The forest plot of this analysis is shown in .
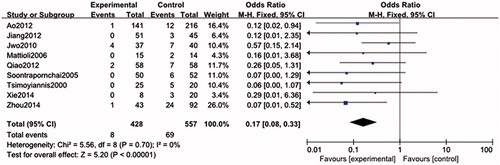
Catheter migration, obstruction, and leakage
There were 985 cases and nine studies included in the analysis, the result showed that comparing with traditional surgery, laparoscopic insertion can significantly reduce the incidence of catheter migration (OR 0.17, 95% CI 0.08–0.33, p < 0.00001).Citation5,Citation7,Citation9,Citation10,Citation12–15,Citation17 The forest plot of this analysis is shown in .
Figure 7. Forest plot. Odds ratios of the incidence of migration between laparoscopic and traditional PD catheter insertion. CI: confidence interval. Experimental: laparoscopic surgery, control: traditional surgery.
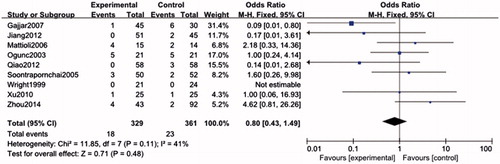
Nine studies involving a total of 690 cases were included in the analysis for obstruction. The results showed that there is no significant difference between the two methods (OR 0.80, 95% CI 0.43–1.49, p = 0.48).Citation4,Citation7–9,Citation11,Citation13–16 The forest plot of this analysis is shown in .
Figure 8. Forest plot. Odds ratios of the incidence of obstruction between laparoscopic and traditional PD catheter insertion. CI: confidence interval. Experimental: laparoscopic surgery, control: traditional surgery.
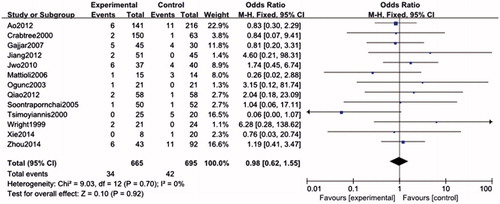
Some papers described the incidence of early and late-period leakage. In this analysis, we combined them together. This analysis included 13 studies involving a total of 1360 cases. The results showed that there is no significant difference between laparoscopic surgery and traditional catheterization in the incidence of leakage (OR 0.98, 95% CI 0.62–1.55; p = 0.92).Citation2,Citation4,Citation5,Citation11,Citation7–15 The forest plot of this analysis is shown in .
Hernia
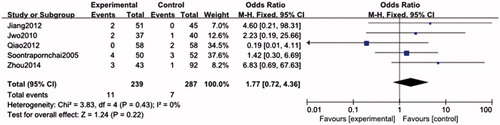
By analyzing 526 cases described in five studies, we found that there is no significant difference between these two methods in the incidence of hernia (OR 1.77, 95% CI 0.72–4.36, p = 0.22).Citation5,Citation9,Citation13–15 The forest plot of this analysis is shown in .
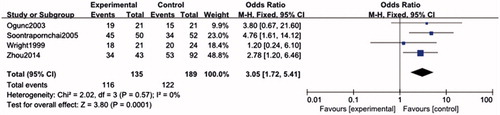
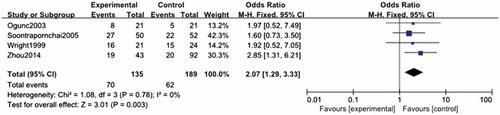
Dialysis catheter survival
A total of four studies involving 324 cases were included in the analysis, the results showed that compared with traditional surgery, laparoscopic insertion has both better catheter 1-year survival rate and 2-year survival rate (1-year survival rate: OR 3.05, 95% CI 1.72–5.41, p = 0.0001; 2-year survival rate: OR 2. 07, 95% CI 1.29–3.33, p = 0.0001).Citation8,Citation9,Citation11,Citation15 The forest plots of these two analyses are shown in and .
GRADE classification
Among all the analysis, only the migration analysis ranked A-level, while the rest fell into Class B or C. The risk of bias accounted for the most of downgrading. The summary of finding table is shown in .
Table 1. Question: should laparoscopy versus traditional surgery be used for PD catheter insertion? (Bibliography: Peritoneoscope versus open surgery for PD. Cochrane Database of Systematic Reviews [Year], Issue [Issue]).
Discussion
Our analysis revealed that laparoscopic surgery is superior to traditional surgery on reducing catheter migration and prolonging catheter survival rate. However, we found a slight increase in the risk of bleeding in laparoscopic surgery. There is no significant difference between the two methods in other catheter-related complications.
Xie et al. first published a systematic review of this topic in 2012, concluding that the two methods had no significant difference in the incidence of catheter-related complications. However, this systematic analysis was based on fewer studies.Citation20 Hagen et al. published another detailed meta-analysis in 2013 which showed that compared with traditional catheter insertion, laparoscopic catheterization can reduce the incidence of catheter migration and prolong 1-year survival but not 2-year survival, which is contrary to Xie’s conclusion.Citation21 By including more studies from China, we came to the above conclusion, which is similar to Hagen’s. And to make the results more instructive, we graded each analysis by GRADEprofeler3.6 (Tajima Tool Corporation, Torrance, CA).
Perforation, defined as the perforation of bowel and bladder, is a relatively rare but serious catheter-related complication, which is mostly due to misoperation during the surgery. Other risk factors include the tension of the intestinal tract and bladder. Our analysis showed the incidence of perforation in laparoscopic group is borderline significantly different from that of the control group. Although laparoscopic method is direct-viewing, patients with previous abdominal surgery, however, are suitable for laparoscopic surgery, which would increase the difficulty and the risk of perforation. Besides, Trocar is more likely to cause intestinal perforation during the puncture of the abdominal wall. As the incidence is not high enough to apply the M–H method, the Peto method is preferred during meta-analysis. The quality of this analysis ranked low for its very serious imprecision. In addition, laparoscopic surgery and traditional surgery are often performed by different operators, which might cause bias.
We found a slightly higher incidence of bleeding in laparoscopic surgery than that of traditional technique. This may partly due to the additional procedure performed in laparoscopic method, including the process of puncturing the abdominal wall by Trocar and suturing PD catheter to the abdominal cavity or peritoneum in laparoscopic surgery.Citation9,Citation12,Citation14,Citation17 Although Öğünç et al.Citation8 reported additional operation during the laparoscopic surgery, such as fixation suture of the omentum (every patient) selective liver biopsy and inguinal hernioplasties, significant risk of bleeding was not observed in this study. In addition, coagulation disorders and preoperative anticoagulant drugs use may also cause bleeding. The studies included did not control these risks, which might cause bias.
In this article, we reached the conclusion that there is no significant difference in the incidence of peritonitis between the two groups. Risk factors include hypoalbuminema, decreased resistance of the patients, and non-standard operation when infusing dialysate. Some studies showed that the kind of preoperative antibiotics prophylaxis may also influence the incidence of peritonitis. Gadallah reported that the use of preoperative single-dose i.v. vancomycin prophylaxis for permanent peritoneal dialysis catheter placement reduced the risk of postoperative peritonitis, while cefazolin did not have statistically significant difference from the control group.Citation22 Among the studies included, two studies reported the use of ceftriaxone and vancomycin (in the case of cephalosporin allergy) as prophylaxis,Citation16,Citation17 six studies did not mention the use of antibiotics,Citation3,Citation4,Citation6,Citation9,Citation12,Citation13 two studies reported the use of cefazolin,Citation5,Citation8 one study reported the use of cefotaxime,Citation7 one study reported that all patients received 2 g of vancomycin intravenously prior to surgery as prophylaxis,Citation11 one study reported antibiotic prophylaxis but did not mention the specific drug, which might cause bias. Furthermore, the small-scale observational study by Öğünç’s is the only one that observed a significant lower incidence in laparoscopic surgery, the four out of 11 cases of peritonitis in open surgery group, however, are associated with exit site infection according to the author.Citation8
Skin and tunnel infection is another major complication after PDC insertion. Leakage, poor resistance of the patients, and non-standard dressing change are among the risk factors. Theoretically, as the procedures of constructing subcutaneous tunnel are similar between these two methods, there might be, regardless of the random effects of other risk factors, a similar incidence of skin and tunnel infection. Our analysis showed no significant difference between the two groups and by more detailed inspection of each study included, we found none of them reached a significant conclusion.
PD catheter migration is a common cause of poor drainage. The underlying mechanism is that external force from either intestinal peristalsis or other mechanical factors pulls the PDC out of the minor pelvis. Our analysis suggested that laparoscopic surgery can significantly reduce the incidence of catheter migration. Specifically, two of the nine studies included showed significant reduction of migration in laparoscopic groups,Citation12,Citation15 and three borderline significant.Citation9,Citation10,Citation14 The visualized process of inserting catheter into the minor pelvis as well as suturing PD catheter to the abdominal cavity may account for this superiority.
PD catheter obstruction resulting from omentum wrapping, protein clots, and tubal blockage of the catheter is another important cause of poor drainage. The study suggested the two methods have similar catheter obstruction incidence. Swartz et al.Citation23 reported a lower incidence of obstruction in curved tube than that of straight tube and among the studies, GajjarCitation4 did not give the corresponding description, while others used the same type of tubes between the experimental and contol groups.Citation7–9,Citation11,Citation13–16 Omentectomy may help reduce migration, which can be performed during laparoscopic method.Citation24 Only Mattioli et al.Citation7 reported the procedure of omentectomy in laparoscopic group, in which the incidence of obstruction, however, is not significantly reduced.
There is no significant difference in the incidence of dialysate leakage between the laparoscopic and open surgery insertion technique. Dialysate leakage occurring in 30 d after surgery is called the early dialysate leakage, which is usually associated with surgery, while that occurring after 30 d is called the late dialysate leakage, which is often associated with mechanical factors. The quality of purse-string or inner suture influences the incidence of leakage, other factors include coughing, obesity, diabetes, age, grand multipara, long-time steroids usage, and recurrent catheter insertions.Citation25 Most leakage can be well controlled after appropriate treatment, and refractory leakage is rare in clinical practice.
Incisional hernia is a common complication that results from poor healing. In clinical practice, the risk factors include infection, which is the most common, the length and location of incision, suturing skills, drainage materials, and general conditions.Citation26 The incidence of hernia is 5–10% in abdominal surgery, 50% of which occur 1–2 years after operation.Citation27 In the above text, we concluded that two groups have no difference in the incidence of infection, and we also found no difference in the incidence of hernia between these two groups.
Last but not the least, we also drew another exciting conclusion that PD catheters inserted by laparoscopic surgery have a significantly higher 1- and 2-year survival rate than the open surgery group. In Xie’s analysis, catheter survival rate was not included as an outcome, and Hagen had concluded that the 2-year catheter survival was only borderline significantly different between the two groups.Citation20,Citation21 Hagen had included 262 patients in their analysis, while we got the above conclusion from 324 cases. Zhou’s study may partly account for the difference. Although many studies reported the 1 year and 2 year survival, only five of them were included for analysis. The rest of them described the survival data by the Kaplan–Meier curve, in which the accurate rate was hard to get. Singh et al.Citation28 analyzed the infectious and non-infectious causes of PD catheter removal based on the data from a single center with a 3-year follow-up, among which migration account for 34.7% of all cases (8/23). We assume that laparoscopic PDC insertion improves catheter survival rate by reducing the incidence of migration significantly.
Besides the above advantages and disadvantages on complications, we also observed other superiorities of laparoscopic method such as the convenience for performing herniorrhaphy during surgery, more suitable for obese patients and those with previous abdominal surgeries, and less operating time. On the contrary, the higher cost, as well as the necessity of general anesthesia and specialized equipment of laparoscopic method, impedes its wider application.
This paper also has some limitations. As RCTs on this study were not sufficient, we included both RCTs and observational studies, which may influence the quality of our study. In addition, the average quality of including studies are medium, and according to GRADE, most of the quality of our analysis ranks B or C, the only study ranking A level was upgraded for the significant differences.
Conclusion
Laparoscopic catheter insertion is superior to traditional technique on reducing catheter migration and prolonging catheter survival rate according to our analysis, but may slightly increase the risk of bleeding. Clinicians should weigh the advantages and disadvantages before selecting the appropriate surgery approach. Specifically, the collaboration of surgeon and nephrologist is recommended for the decision of surgery approach as well as the management of PDC-related complications.
In recent years, transumbilical endoscopic surgery (TUES) has become a new hotspot in minimally invasive surgery, which may reduce surgical trauma and bring the same benefits.Citation29 Despite the limitations of our analysis, this article provides a more concrete answer to this controversial issue. To find out the optimal surgical approach still needs larger randomized controlled trials.
Acknowledgements
The authors thank Dr. Tang Wen of Peking University for her work of revising this paper.
Declaration of interest
The authors report that they have no conflicts of interest.
References
- Wang HY. Nephrology. 3rd ed. Beijing: People's Medical Publishing House; 2008
- Crabtree JH, Fishman A. Videolaparoscopic implantation of long-term peritoneal dialysis catheters. Surg Endosc. 1999;13(2):186–190
- Draganic B, James A, Booth M, Gani JS. Comparative experience of a simple technique for laparoscopic chronic ambulatory peritoneal dialysis catheter placement. Aust N Z J Surg. 1998;68(10):735–739
- Gajjar AH, Rhoden DH, Kathuria P, Kaul R, Udupa AD, Jennings WC. Peritoneal dialysis catheters: Laparoscopic versus traditional placement techniques and outcomes. Am J Surg. 2007;194(6):872–875; discussion 875–6
- Jwo SC, Chen KS, Lin YY. Video-assisted laparoscopic procedures in peritoneal dialysis. Surg Endosc. 2003;17(10):1666–1670
- Lund L, Jonler M. Peritoneal dialysis catheter placement: Is laparoscopy an option? Int Urol Nephrol. 2007;39(2):625–628
- Mattioli G, Castagnetti M, Verrina E, et al. Laparoscopic-assisted peritoneal dialysis catheter implantation in pediatric patients. Urology. 2007;69(6):1185–1189
- Öğünç G, Tuncer M, Ogunc D, Yardimsever M, Ersoy F. Laparoscopic omental fixation technique versus open surgical placement of peritoneal dialysis catheters. Surg Endosc. 2003;17(11):1749–1755
- Soontrapornchai P, Simapatanapong T. Comparison of open and laparoscopic secure placement of peritoneal dialysis catheters. Surg Endosc. 2005;19(1):137–139
- Tsimoyiannis EC, Siakas P, Glantzounis G, et al. Laparoscopic placement of the Tenckhoff catheter for peritoneal dialysis. Surg Laparosc Endosc Percutan Tech. 2000;10(4):218–221
- Wright MJ, Bel'eed K, Johnson BF, Eadington DW, Sellars L, Farr MJ. Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int. 1999;19(4):372–375
- Ao X, Zhou Q, Nie W, Ouyang Y. Clinical comparison of peritoneal dialysis catheter placement under laparoscope and by conventional surgical methods. Chin J Blood Purif. 2012;11(10):544–548
- Jiang H, Li YL, Jia YNX, Song X, Yue H, Lu C. Clinical comparative study of two peritoneal dialysis surgery catheterization. Prog Mod Biomed. 2012;12(30):5878–5881
- Qiao Q, Lu GY, Xu DY, Zhou XJ, Li L. A comparison of two methods for catherization in peritoneal dialysis. Jiangsu Med J. 2012;38(23):2812–2814
- Zhou CM, Zhao X, Zhang JH, Tai QW. Comparison of laparoscopic and open surgical placement of peritoneal dialysis catheters. J Xinjiang Med Univ. 2014;37(05):598–602
- Xu T, Zang L, Xie JY. Efficacy and safety of laparoscopic and conventional placement of peritoneal dialysis catheters in patients with ESRD. J Nephrol Dialy Transplant. 2010;19(5):430–434
- Xie P, Yuan L, Liu F. The comparision of efficacy and safety between laparoscopic and conventional placement of peritoneal dialysis catheters. Hebei Med. 2014;20(04):562–566
- Higgins JPT, Green S. The Cochrane Collaboration: Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.2011; Available at: www.cochrane-handbook.org
- Wells GA, Shea B, O'Connell D, Petersen J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale(NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2015; Available at: http://www.ohri.ca/
- Xie H, Zhang W, Cheng J, He Q. Laparoscopic versus open catheter placement in peritoneal dialysis patients: A systematic review and meta-analysis. BMC Nephrol. 2012;13:69
- Hagen SM, Lafranca JA, Steyerberg EW, JN IJ, Dor FJ. Laparoscopic versus open peritoneal dialysis catheter insertion: A meta-analysis. PLoS One. 2013;8(2):e56351
- Gadallah MF, Ramdeen G, Torres C, et al. Preoperative vancomycin prophylaxis for newly placed peritoneal dialysis catheters prevents postoperative peritonitis. Adv Perit Dial. 2000;16:199–203
- Swartz R, Messana J, Rocher L, Reynolds J, Starmann B, Lees P. The curled catheter: Dependable device for percutaneous peritoneal access. Perit Dial Int. 1990;10(3):231–235
- Crabtree JH, Fishman A. Laparoscopic omentectomy for peritoneal dialysis catheter flow obstruction: A case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 1999;9(3):228–233
- Dombros N, Dratwa M, Feriani M, et al. European best practice guidelines for peritoneal dialysis. 3 Peritoneal access. Nephrol Dial Transplant. 2005;20(Suppl. 9):ix8–ix12
- Lauwers P, Bracke B, Hubens G, Vaneerdeweg W. Unusual complications of preperitoneal mesh implantation in the treatment of inguinal hernia. Acta Chir Belg. 2003;103(5):513–516
- Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. 2011;3(3):CD007781
- Singh N, Davidson I, Minhajuddin A, Gieser S, Nurenberg M, Saxena R. Risk factors associated with peritoneal dialysis catheter survival: A 9-year single-center study in 315 patients. J Vasc Access. 2010;11(4):316–322
- Canes D, Desai MM, Aron M, et al. Transumbilical single-port surgery: Evolution and current status. Eur Urol. 2008;54(5):1020–1029