Abstract
Objectives: To compare the renal outcomes in patients of unilateral renal cell carcinoma (RCC) with upper tract urothelial carcinoma (UTUC) following surgical resection of the tumor-bearing kidney, and to investigate the potential predictors in renal function decline. Patients and methods: In this retrospective cohort study, 319 RCC patients undergoing radical nephrectomy (RN) and 297 UTUC patients undergoing radical nephroureterectomy were recruited from a tertiary medical center between 2001 and 2010. Demographic data, co-morbidity, smoking habit, baseline estimated glomerular filtration rate (eGFR) calculated by chronic kidney disease-epidemiology equation, as well as tumor staging of RCC and UTUC, were recorded. The primary endpoint was serum creatinine doubling and/or end-stage renal disease (ESRD) necessitating long-term dialysis. Cox proportional hazard model and Fine and Gray's competing risk regression accounting for death were used to model renal outcome. Results: UTUC patients had a higher incidence rate of renal function deterioration than RCC patients did (15.01 vs. 2.68 per 100 person-years, p<0.001). In Cox proportional hazard model and Fine and Gray's competing risk regression, UTUC was significantly associated with increased risk of creatinine doubling and/or ESRD necessitating dialysis (hazard ratio, 3.13; 95% confidence interval, 2.01–4.87) as compared to RCC following unilateral RN. Nevertheless, our study is observational in nature and cannot prove causality. Conclusions: UTUC per se is strongly associated with kidney disease progression as compared to RCC following unilateral nephrectomy. Further studies are needed to elucidate this association.
Introduction
Among the malignancies of genitourinary system, most tumors in the renal parenchyma are renal cell carcinomas (RCCs), while those in the renal pelvis and urinary tract are urothelial carcinomas (UCCs). RCCs are responsible for approximately 90–95% of kidney cancers,Citation1 whereas upper tract urothelial carcinomas (UTUCs) account for only 5–10% of kidney cancers in the USA.Citation1,Citation2 So far, tumor excision or total resection of the tumor-bearing kidney offers the only chance of cure for localized RCCs and UTUCs.Citation3,Citation4 For small and solitary RCCs, partial nephrectomy has been advocated for the potential benefit of nephron preservation.Citation5 However, radical nephrectomy (RN) still remains the most commonly surgical procedure for the treatment of localized RCCs if there was no solitary kidney or severe renal impairment.Citation6 As to UTUCs, radical nephroureterectomy (RNU) with excision of the bladder cuff is the golden standard treatment, regardless of the tumor size or location within the upper urinary tract.Citation4 The generally accepted principle of the extensive resection is to avoid tumor seeding and minimize the risk of tumor recurrence.
To date, currently available data in kidney function deterioration after unilateral RN are still controversial. In comparison with partial nephrectomy for RCCs, some studies showed that RN led to a postoperative decline in the estimated glomerular filtration rate (eGFR).Citation6–8 As for UTUCs, some studies also showed a decline in renal function following unilateral RNU.Citation9–11 By contrast, other studies found that renal function in RCC patients was relatively stable after RN even in the presence of compromised baseline renal function in 5–10 years observation period.Citation12,Citation13 Reasons for the conflicting results may be due to differences in sample size, methodology, and follow-up period, and statistical drawbacks. Mortality commonly occurs in cancer patients and is a competing factor with the initiation of dialysis in postoperative follow-up. However, investigators rarely applied the competing risk regression accounting for death to model kidney function decline and the need for dialysis in most studies. The impairment or loss of renal function may render patients ineligible for chemotherapy after surgery as well as requiring long-term dialysis.Citation10 Therefore, it is imperative to investigate and validate the relationship between urological cancers and chronic kidney disease (CKD). To date, limited information is available to compare the long-term kidney function change between the two major urological cancers after unilateral RN. Accordingly, we utilized the mortality as a competing factor in Cox regression models to assess the effect of unilateral RN on renal outcome between RCCs and UTUCs in a 10-year follow-up study. We further assessed the potential predictors of postoperative kidney disease progression.
Patients and methods
Study cohort
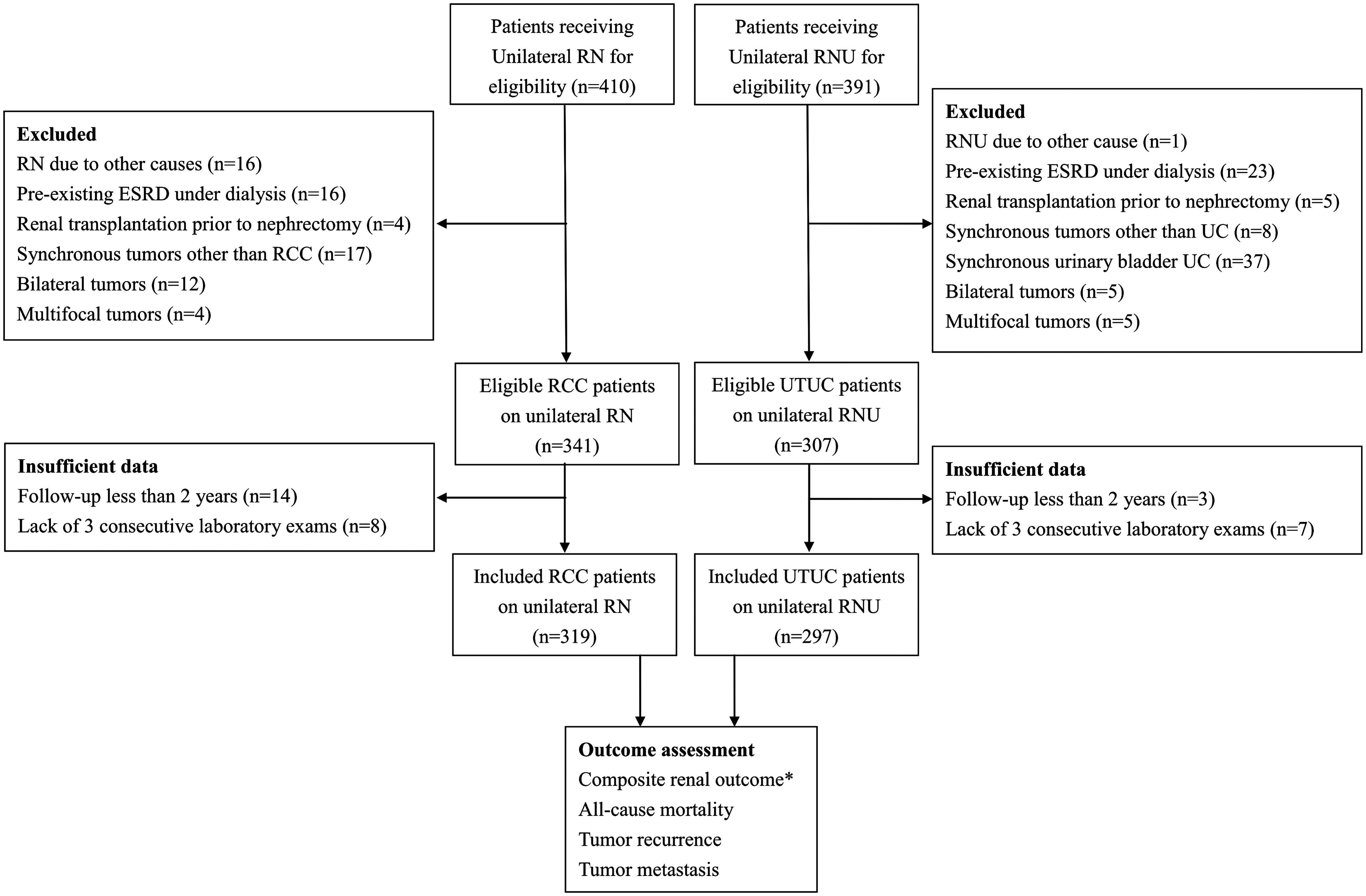
A retrospective cohort study was conducted at Taipei Veteran General Hospital, Taiwan. We used codes from International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) within the medical database to identify patients receiving RN (n=410) and RNU (n=391) between 2000 and 2010 (). The exclusion criteria in this study were an abnormal contralateral radiological kidney or solitary functional kidney, synchronous malignancy other than UTUC and RCC, bilateral or multifocal tumors within the urinary system, receiving nephrectomy for other cause, and ESRD underwent maintenance dialysis or renal transplantation prior to nephrectomy. Because the postoperative eGFR dropped significantly during the first 3–5 months after unilateral nephrectomy, and then remained stable in the following 1–2 years,Citation11,Citation12 the observation period should be at least 2 years to assess the rate of eGFR decline for CKD progression. Moreover, patients with a rapid kidney function decline within 2 year after unilateral RN may be attributed to other aggravating factors such as surgical complications, trauma, sepsis and cardiovascular events. Therefore, patients with a follow-up less than 2 years, and a lack of three consecutive laboratory examinations, were excluded from this study. Finally, a total of 319 RCC and 297 UTUC patients presented a solitary tumor mass following unilateral RN and RNU, respectively, were enrolled in this study. The study was based on the Declaration of Helsinki and approved by the Institutional Research Board at National Yang-Ming University, Taiwan. The informed consent was waived due to the reidentified personal information in the Database at Taipei Veterans General Hospital.
Data collection and follow-up
The clinical characteristics and laboratory data at the time of nephrectomy included gender, age, smoking history, co-morbidities such as hypertension, diabetes mellitus (DM), cerebrovascular disease, coronary artery disease (CAD), and peripheral artery disease (PAD), body mass index, and eGFR calculated by the CKD-epidemiology formula. The tumor staging was determined according to the 2010 American Joint Committee on Cancer,Citation14,Citation15 with variables of tumor size, extraparenchymal extension, lymph node involvement and presence of metastasis. In addition, laboratory data of pre- and postoperative serum albumin and serum creatinine, CKD stages according to KDOQI,Citation16 and time to serum creatinine doubling or to initiate dialysis were recorded. The survival period was calculated from the date of surgery until death, and the disease-free interval was calculated from the date of surgery until onset of the first event of tumor recurrence or distant visceral metastasis. The two cohorts were observed from the date of the nephrectomy until death or censoring. Patients who had no events were therefore censored at the time of their last follow-up or until 31 October 2014.
Endpoints
The primary endpoint was renal outcomes defined as doubling of baseline serum creatinine and/or end-stage renal disease (ESRD) necessitating long-term dialysis. The second endpoints were all-cause mortality, cancer recurrence and distant visceral metastasis after nephrectomy.
Statistical analysis
Descriptive statistics were used to characterize the study cohorts at baseline. Baseline characteristics were compared between the two cohorts, using χ2 test for categorical variables and independent t-test and Mann–Whitney U-test for parametric and nonparametric continuous variables, respectively. We calculated and compared the cumulative incidences of renal outcome and all-cause mortality by the modified Kaplan–Meier method and tested with the log-rank statistic. The risks of endpoints were analyzed by Cox proportional hazard models with adjusted covariates listed in . Besides, Fine and Gray's competing risk regression accounting for death was used to model renal outcome, tumor recurrence and metastasis.Citation17 Finally, to determine the independent risk factors of composite renal outcome, multivariable analyses were conducted by modified Cox proportional hazard models. Data management and analyses were conducted using STATA statistical software (version 13.0; StataCorp., College Station, TX). Statistical significance was defined as p<0.05.
Table 1. Demographic and clinical characteristics of study subjects with UTUC and RCC receiving unilateral RN.
Results
Baseline characteristics
During a 10-year follow-up, a total of 297 UTUC and 312 RCC patients were recruited. The clinical characteristics at baselines are presented in . As compared to RCC patients, UTUC patients were older and more likely to have DM, CAD and PAD, as well as had lower percentage in man, and lower BMI and serum albumin at study entry. According to the eGFR-based definition of KDOQI,Citation16 UTUC patients were more likely to have moderate to advanced CKD (stages 3b–5), whereas RCC patients were mainly of early CKD (stages 1–3a). Tumor stages were predominantly III–IV in UTUC patients while I–II in RCC patients.
Renal outcome
The incidence rates of serum creatinine doubling and ESRD necessitating dialysis are shown in . The incidence rate of composite renal outcome was 15.01 per 100 patient-years in UTUC patients and 2.68 per 100 patient-years in RCC patients, respectively. Kaplan–Meier curve showed that the cumulative incidence of composite renal outcome was significantly higher among UTUC patients than RCC patients (). In the Cox proportional hazard model, UTUC patients were associated with an increased risk of serum creatinine doubling and/or ESRD necessitating dialysis [HR, 2.90; 95% confidence interval (CI), 1.88–4.49; p< 0.001] as compared to RCC patients after unilateral RN with adjusted covariates listed in . The risk for composite renal outcome (HR, 3.13; 95% CI, 2.01–4.87; p<0.001) in UTUC patients was consistent in Fine and Gray's competing risk regression accounting for death ().
Figure 2. Kaplan–Meier curves of the cumulative incidence of serum creatinine doubling and/or ESRD necessitating dialysis (A) and all-cause mortality (B) in patients of UTUC and RCC after unilateral RN during a 10-year follow-up. Notes: RCC, renal cell carcinoma; UTUC, upper tract urothelial carcinoma.
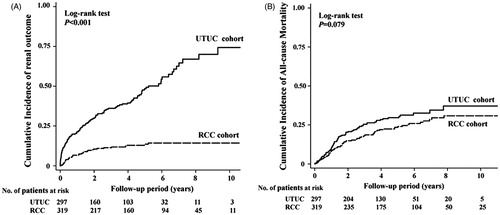
Table 2. Incidence rate and risk of renal outcome, overall mortality, tumor recurrence and metastasis among patients with UTUC compared with those with RCC receiving unilateral RN.
The univariate analysis showed that UTUC receiving RNU as well as age, female, current smoker, presence of DM, CAD and PAD, preoperative eGFR <45 mL/min/1.73 m2 and low serum albumin were potential predictors of composite renal outcome (). Factors with p<0.1 in univariate analysis were included in the multivariate regression analysis, by which the independent predictors were determined (). The results revealed that 1-year increase of age (HR, 1.03; 95% CI, 1.01–1.04), presence of DM (HR, 1.52; 95% CI, 1.07–2.14), preoperative eGFR <15 mL/min/1.73 m2 (HR, 4.14; 95% CI, 2.20–7.78) and UTUC after RNU (HR, 3.73; 95% CI, 2.46–5.65) were the independent predictors associated with the risk of serum creatinine doubling and/or ESRD necessitating dialysis.
Figure 3. Multivariate regression analysis of potential predictors for composite renal outcome among patients with UTUC and RCC after unilateral RN. *Composite renal outcome: serum creatinine doubling and/or ESRD necessitating dialysis. Notes: RCC, renal cell carcinoma; UTUC, upper tract urothelial carcinoma.
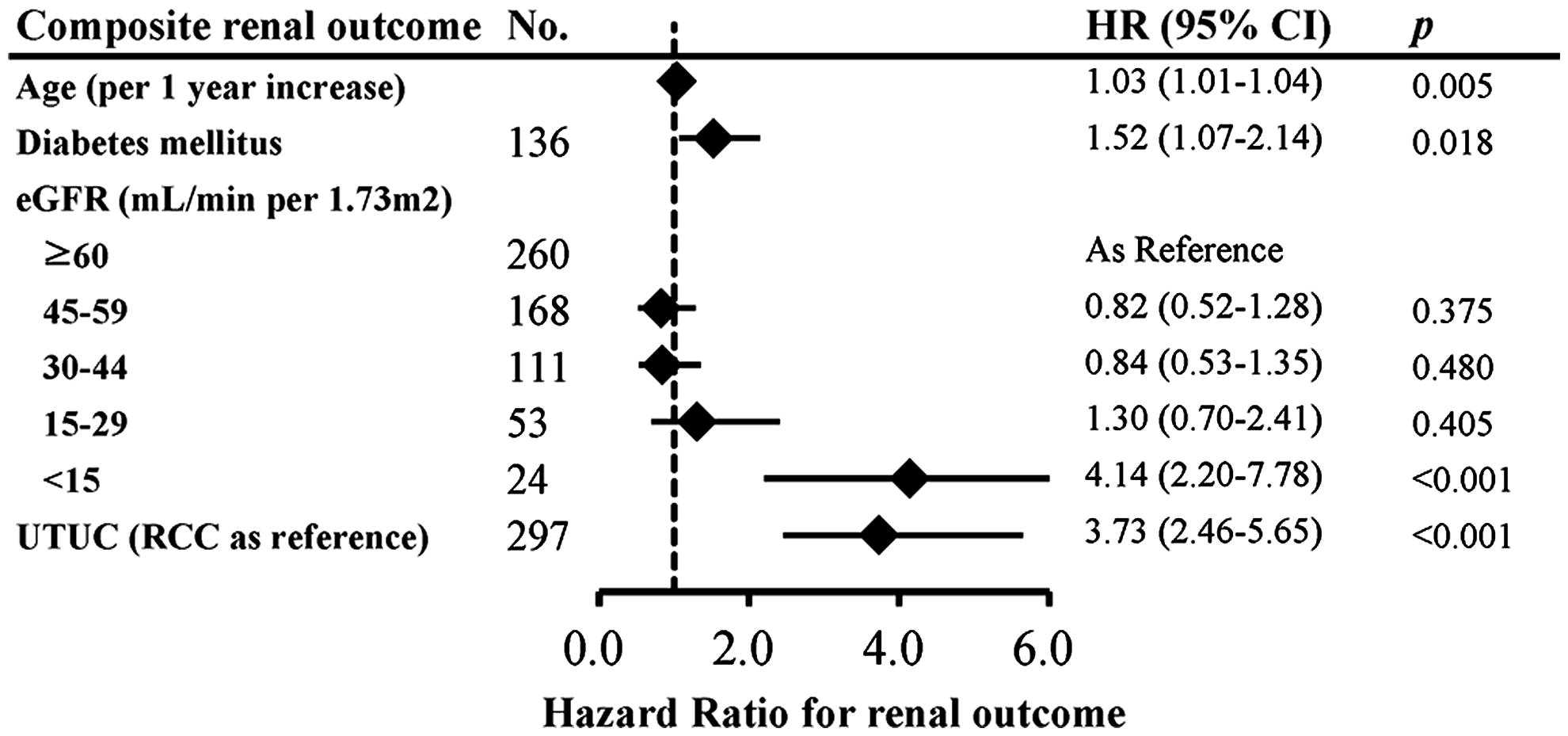
Table 3. Potential predictors for composite renal outcome in patients with UTUC and RCC receiving unilateral RN.
Oncological outcomes
The incidence rates of all-cause mortality were 7.36 per 100 person-years in UTUC patients and 4.97 per 100 person-years in RCC patients. Kaplan–Meier curve () showed a modest difference in the cumulative incidence of all-cause mortality between UTUC and RCC patients (log-rank, p=0.079). In the Cox proportional hazard model, UTUC patients receiving RNU were associated a lower risk of all-cause mortality (HR, 0.62; 95% CI, 0.41–0.94) as compared to RCC patients receiving RN.
The incidence rates of tumor recurrence were 15.81 per 100 person-years in UTUC patients and 0.89 per 100 person-years in RCC patients. In Cox proportional hazard model and Fine and Gray's competing risk regression accounting for death, UTUC exhibited a higher risk of tumor recurrence (HR, 17.04; 95% CI, 8.75–33.19) as compared with RCC.
The incidence rates of tumor metastasis were 4.01 per 100 person-years in UTUC patients and 4.82 per 100 person-years in RCC patients. In Cox proportional hazard model and Fine and Gray's competing risk regression accounting for death, UTUC patients were significantly associated with a lower risk of tumor metastasis (HR, 0.47; 95% CI, 0.26–0.84) as compared with the RCC patients.
Discussion
To our best knowledge, we, for the first time, performed a head-to-head comparison of postoperative renal outcomes between UTUC and RCC receiving RNU and RN, respectively. The multivariate analysis showed that old age, presence of DM and low baseline eGFR (<15 mL/min/1.73 m2) were the independent predictors of kidney function deterioration after unilateral RN. Most importantly, by competing with the risk of death, UTUC patients were strongly associated with an increased risk of serum creatinine doubling and/or ESRD necessitating dialysis as compared to RCC patients.
Theoretically, the loss of one kidney by surgical removal would result in compensatory hyperfiltration and hypertrophy of the contralateral kidney. Previous studies have shown that the living kidney transplant donors have nearly equivalent rate of kidney failure or death compared with normal individuals.Citation18,Citation19 Therefore, the impact of RN on renal function was minimal as long as the patient has a normal contralateral kidney. In a retrospective cohort study, Hew et al. illustrated that RCC patients receiving RN and living kidney donors matched for age and gender had similar renal function at 6 months and 1 year postoperatively, despite a higher co-morbidity load and lower baseline eGFR in patients with RCCs.Citation20 However, more emerging evidence revealed that the genitourinary (GU) cancers following unilateral RN could cause a detectable and permanent rise in serum creatinine through a longer period, owing to the underlying co-morbidities, intrinsic renal abnormalities and limited number of remnant nephrons to overwhelm the renal compensatory mechanism.Citation6,Citation8,Citation10 In the present study, we found that UTUCs were associated with the deleterious renal outcomes as compared to RCCs after unilateral RN. Although UTUC patients were more likely to have advanced CKD than RCC patients, their risk of composite renal outcome is still existed after adjusting for the baseline eGFR and all co-morbidities in Cox regression analysis. A questionnaire survey of 350 hemodialysis patients indicated that only 7 (2%) ESRD patients were identified as having unilateral RCCs.Citation21 By contrast, UTUCs pose a remarkably high prevalence among ESRD patients.Citation22 Therefore, it is speculated that some pathology processes may exist within the contralateral kidney in UTUC patients, leading to the indolent and persistent renal damage even after removal of the tumor-involved kidney.
In the present study, the ratio of female to male among nearly 300 UTUC patients was approximately 1:1. The results corroborate the data in a nationwide epidemiology study of UTUC in Taiwan, showing a significantly higher ratio of UTUC among all urinary tract tumors, as well as an unusual increase in the ratio of female to male incidence.Citation23 Besides chronic analgesic abuse, cigarette consumption and arsenic poisoning in drinking water, the population-based case–control studies in Taiwan indicated that aristolochic acid (AA) exposure was significantly associated with an enhanced risk of UTUC,Citation24 and there was a dose-dependent relationship between cumulative AA exposure and ESRD development.Citation25 Among the risk factors, AA exposure and chronic analgesic abuse have been recognized as potent urological carcinogens together with nephrotoxins. Since urothelial neoplasms may precede renal dysfunction after AA or analgesic exposure, it is reasonable to speculate that indolent renal tubular damage and interstitial fibrosis might have been existed in the tumor-uninvolved renal tissues at the time of UTUC development.Citation26 Accordingly, the deleterious renal function changes following RNU for UTUC in our study may be explained by the presence of interstitial inflammation and fibrosis induced by AA or nephrotoxic carcinogens within the contralateral kidney.
Identification of patients at risk of CKD progression is crucial to physicians for better optimized treatment to preserve residual renal function. Old age and low baseline eGFR are well-known predictors for postoperative renal deterioration.Citation8,Citation11 Therefore, for RCC patients with old age and advanced CKD, partial nephrectomy is considered to avoid accelerating ESRD development postoperatively.Citation3 By contrast, in selected UTUC patients with a greater burden of co-morbidities, nephron-sparing procedure like endoscopic resection of tumor carries a much higher burden of local recurrence and years of complicated and costly surveillance.Citation27 RNU may render many older and CKD patients ineligible for adjuvant platinum-based chemotherapy. Thereafter, neoadjuvant regimens for systemic therapy were strongly indicated in such high risk group.Citation20 Our finding that DM is an independent risk factor of renal function deterioration following RN is compatible with the accepted concept in medical practice. It may emphasize the need for adequate glycemic control in renal preservation for diabetes patients with GU cancers following RN.
Some limitations should be acknowledged in this study. First, the study population was composed of Taiwanese patients from a single medical center, and thus the results may not be applicable to other ethnic groups. Second, in lack of specific details on surgical techniques, we could not assess whether different techniques used may have a differential effect on CKD and related outcomes. Third, the details on analgesic and AA exposure were not available in our study. Fourth, selection bias may exist because this study was based on a retrospective cohort design. However, we have adjusted for the potential confounders and competed with the risk of death in the multivariate Cox regression models. Finally, our study is observational in nature, so it cannot prove causality.
Conclusion
Our study demonstrated that UTUC per se is associated with a high risk of serum creatinine doubling and/or ESRD necessitating dialysis following unilateral RNU. Physicians should pay more attention to the high risk group, especially in those with old age, DM, and low baseline eGFR. Further studies are needed to assess this association.
Declaration of interest
This work was supported by grants from the National Science Council (NSC 102–2314-B-010-004-MY3; NSC 102–2314-B-303-003), Taipei Veterans General Hospital (V102C-129; V103C-024), Foundation for Poison Control, and Ministry of Education Aim for the Top University Plan in Taiwan.
References
- Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300
- Munoz JJ, Ellison LM. Upper tract urothelial neoplasms: Incidence and survival during the last 2 decades. J Urol. 2000;164:1523–1525
- Ljungberg B, Cowan NC, Hanbury DC, et al. EAU guidelines on renal cell carcinoma: The 2010 update. Eur Urol. 2010;58:398–406
- Roupret M, Babjuk M, Comperat E, et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 2013;63:1059–1071
- Li W, Cheng Y, Cheng Y, et al. Clinical efficacy of radical nephrectomy versus nephron-sparing surgery on localized renal cell carcinoma. Eur J Med Res. 2014;19:58
- Huang WC, Levey AS, Serio AM, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: A retrospective cohort study. Lancet Oncol. 2006;7:735–740
- Kim CS, Bae EH, Ma SK, et al. Impact of partial nephrectomy on kidney function in patients with renal cell carcinoma. BMC Nephrol. 2014;15:181
- Mariusdottir E, Jonsson E, Marteinsson VT, et al. Kidney function following partial or radical nephrectomy for renal cell carcinoma: A population-based study. Scand J Urol. 2013;47:476–482
- Meyer JP, Delves GH, Sullivan ME, Keoghane SR. The effect of nephroureterectomy on glomerular filtration rate. BJU Int. 2006;98:845–848
- Kaag MG, O'Malley RL, O'Malley P, et al. Changes in renal function following nephroureterectomy may affect the use of perioperative chemotherapy. Eur Urol. 2010;58:581–587
- Kaag M, Trost L, Thompson RH, et al. Preoperative predictors of renal function decline after radical nephroureterectomy for upper tract urothelial carcinoma. BJU Int. 2014;114:674–679
- Chung JS, Son NH, Byun SS, et al. Trends in renal function after radical nephrectomy: A multicentre analysis. BJU Int. 2014;113:408–415
- Lane BR, Campbell SC, Demirjian S, Fergany AF. Surgically induced chronic kidney disease may be associated with a lower risk of progression and mortality than medical chronic kidney disease. J Urol. 2013;189:1649–1655
- Moch H, Artibani W, Delahunt B, et al. Reassessing the current UICC/AJCC TNM staging for renal cell carcinoma. Eur Urol. 2009;56:636–643
- Roscigno M, Cha EK, Rink M, et al. International validation of the prognostic value of subclassification for AJCC stage pT3 upper tract urothelial carcinoma of the renal pelvis. BJU Int. 2012;110:674–681
- Inker LA, Astor BC, Fox CH, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. 2014;63:713–735
- Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509
- Vincenti F, Amend WJ Jr, Kaysen G, et al. Long-term renal function in kidney donors. Sustained compensatory hyperfiltration with no adverse effects. Transplantation. 1983;36:626–629
- Williams SL, Oler J, Jorkasky DK. Long-term renal function in kidney donors: A comparison of donors and their siblings. Ann Intern Med. 1986;105:1–8
- Hew MN, Opondo D, Cordeiro ER, et al. The 1-year decline in estimated glomerular filtration rate (eGFR) after radical nephrectomy in patients with renal masses and matched living kidney donors is the same. BJU Int. 2014;113:E49–E55
- Peces R, Alvarez-Navascues R. Unilateral renal cell carcinoma with coexistent renal disease: A rare cause of end-stage renal disease. Nephrol Dial Transplant. 2001;16:291–294
- Wang SM, Lai MN, Chen PC, et al. Increased upper and lower tract urothelial carcinoma in patients with end-stage renal disease: A nationwide cohort study in Taiwan during 1997–2008. Biomed Res Int. 2014;2014:149750
- Chou YH, Huang CH. Unusual clinical presentation of upper urothelial carcinoma in Taiwan. Cancer. 1999;85:1342–1344
- Lai MN, Wang SM, Chen PC, et al. Population-based case–control study of Chinese herbal products containing aristolochic acid and urinary tract cancer risk. J Natl Cancer Inst. 2010;102:179–186
- Lai MN, Lai JN, Chen PC, et al. Risks of kidney failure associated with consumption of herbal products containing Mu Tong or Fangchi: A population-based case–control study. Am J Kidney Dis. 2010;55:507–518
- Nortier JL, Schmeiser HH, Muniz Martinez MC, et al. Invasive urothelial carcinoma after exposure to Chinese herbal medicine containing aristolochic acid may occur without severe renal failure. Nephrol Dial Transplant. 2003;18:426–428
- Simhan J, Smaldone MC, Egleston BL, et al. Nephron-sparing management vs radical nephroureterectomy for low- or moderate-grade, low-stage upper tract urothelial carcinoma. BJU Int. 2014;114:216–220