Abstract
Neutrophil–lymphocyte ratio (NLR) is a marker of systemic inflammation that has been shown to predict mortality in patients with malignancies, ischemic heart disease and peripheral vascular disease. Its prognostic value in hemodialysis patients is unclear. The aims of this study were to: (i) explore the relationship between NLR and other biochemical parameters and (ii) to examine the value of NLR as a predictor of cardiovascular and all-cause mortality in hemodialysis patients. The study included all the incident hemodialysis patients from a single center between 2007 and 2012. NLR was calculated using samples obtained 3 months after commencing hemodialysis. One hundred seventy hemodialysis patients were included with a median follow-up of 37 months. There were 54 deaths (32%). NLR was positively correlated with C-reactive protein (r = 0.24, p = 0.0023) and negatively correlated with hemoglobin (r = −0.27, p = 0.00048), albumin (r = −0.23, p = 0.0034) and total cholesterol (r = −0.17, p = 0.049) levels. In multivariate Cox regression, NLR was independently associated with both all-cause mortality (adjusted hazard ratio [HR] 1.4; 95% confidence interval [CI], 1.2–1.6; p ≤ 0.0001) and cardiovascular death (HR 1.3, 95% CI 1.1–1.6, p = 0.0032). Other predictors of all-cause mortality were age (HR 1.6 per decade; 95% CI, 1.2–2.1; p = 0.0017), body mass index (HR 0.93; 95% CI, 0.88–0.98; p = 0.0047), albumin (HR 0.91; 95% CI, 0.86–0.97; p = 0.0035) and peripheral vascular disease (HR 2.7; 95% CI, 1.4–5.1; p = 0.0023). NLR is a practical, cost-efficient and easy to use predictor of cardiovascular and all-cause mortality in incident hemodialysis patients.
Introduction
Excessive mortality in patients with end-stage kidney disease (ESKD) has been attributed, in part, to its heightened pro-inflammatory state, characterized by increased levels of pro-inflammatory cytokines such as tumor necrosis factor (TNF)-alpha, interleukin (IL)-6 and C-reactive protein (CRP).Citation1–3 Inflammation has been shown to be important in the initiation and progression of atherosclerosis, the leading cause of death in ESKD patients, through leukocyte adhesion and infiltration of the vascular endothelium.Citation4 The etiology of systemic inflammation in ESKD patients is multifactorial and is contributed by both dialysis (e.g., membrane bioincompatibility, endotoxemia and loss of residual renal function) and non-dialysis related factors (e.g., infections and intercurrent clinical events).Citation1
Recent studies have demonstrated an association between the neutrophil–lymphocyte ratio (NLR) and pro-inflammatory cytokines including TNF-alpha and IL-6 levels in pre-dialysis and dialysis patients.Citation5,Citation6 Unlike TNF-alpha and IL-6, which require separate tests, NLR can be readily calculated from a patient’s full blood count without incurring additional cost. NLR has been identified as a marker of systemic inflammation and prognostic marker for mortality in patients with solid organ malignancies,Citation7 peripheral vascular disease,Citation8,Citation9 and in the setting of acute coronary syndrome.Citation10,Citation11 Despite this, few studies have investigated the prognostic value of NLR in patients with chronic kidney disease, with none focusing solely on hemodialysis patients.Citation12,Citation13
The aims of this study were to explore the relationship between NLR and other biochemical parameters, and to examine the value of NLR as a predictor of cardiovascular and all-cause mortality in hemodialysis patients.
Materials and methods
The human research ethics committee for the participating hospital approved the study (HREC/13/QCH/120). Informed patient consent was waived due to the retrospective nature of the study.
Settings and patients
All the incident hemodialysis patients between January 2007 and December 2012 at a single center were included in the study. Patients with active solid organ or hematological malignancies, those with chronic infections, and those who died within 6 months of commencing hemodialysis, were excluded from the study as their NLR levels would have been affected by “acute” factors (e.g., line-related bacteremia), rather than representing the background chronic inflammatory burden. Patients who had a failed renal transplant and returned to hemodialysis during the study period were also excluded. Patients receiving prednisolone or other immunosuppressive therapies were not excluded. All the patients underwent hemodialysis 3 times/week for 4–5 h/session, as specified by the treating nephrologist.
Clinical and biochemical variables assessed
A retrospective review of the electronic pathology system was conducted to record patient’s full blood count, biochemical and inflammatory biomarkers after the commencement of hemodialysis as part of routine clinical care. Full blood counts, including hemoglobin, total white blood cell count, neutrophils, and lymphocytes were obtained 3 months after the commencement of hemodialysis. This approach was chosen because patients were considered clinically stable at this time and to reduce the influence of other transient factors at the commencement of hemodialysis that might affect inflammatory status (e.g., temporary central venous catheter use). Results from patients who were hospitalized with an acute illness 3 months after dialysis initiation were excluded. In these cases, the next available outpatient dialysis unit results were included for analyzes. Biochemical variables including corrected calcium, phosphate, parathyroid hormone (PTH), serum albumin, ferritin, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides (TG), and CRP were recorded if results were available within 3 months of full blood count.
Biochemical information was analyzed by a single hospital pathology service except in the case of PTH. Full blood counts were measured using Roche XE-5000 and the XT-2000i. Electrolytes, renal and liver function, lipid profiles and CRP were performed on Beckman Coulter DX600i. PTH was performed on the Siemens Immulite 2000 XPi analyzer.
Information from the Australian and New Zealand Dialysis and Transplant Registry (ANZDATA) was recorded for each patient in the year of hemodialysis commencement. These clinical variables were used to describe baseline patient characteristics. Variables recorded were patient age, gender, Aboriginal or Torres Strait Islander ethnicity, smoking status, late referral to nephrologist (defined as referral within 3 months of dialysis initiation), vascular access at first hemodialysis, underlying renal disease, body mass index (BMI), presence of diabetes mellitus, ischemic heart disease, peripheral vascular disease, cerebrovascular disease, and chronic lung disease. ANZDATA information was also obtained to determine the cause of death.
Follow-up and statistical analysis
Descriptive statistics were calculated for the study cohort and reported as mean ± SD or median and interquartile range for continuous data, depending on their distribution, and frequency (%) for categorical variables. Baseline characteristics of patients grouped according to the median NLR value were compared using Student’s t test or Mann–Whitney’s U test for continuous variables and chi-squared test or Fisher’s exact test for dichotomous variables. The relationship between the NLR and other metabolic and inflammatory markers was assessed using Spearman’s rank correlation.
Patient survival curves for all-cause and cardiovascular mortality based on NLR groupings were generated according to the Kaplan–Meier method. Statistical significance was assessed using log-rank test. Patients were followed up until July 2014 or death and censored for loss to follow-up or transplantation. Univariate Cox regression analysis was used to identify predictors of cardiovascular and all-cause mortality. Cardiovascular mortality was defined as death due to myocardial infarction, heart failure, cardiac arrest, cerebrovascular accident or peripheral vascular disease. Significant predictors were subsequently added to the multivariable model and forward stepwise Cox regression identified the most parsimonious model. The probability used for the stepwise regression was set at 0.05 for entry of variables and 0.1 for removal. All data were recorded and analyzed by using SPSS software (version 21; IBM, Armonk, New York). p Values <0.05 were considered to be statistically significant.
Results
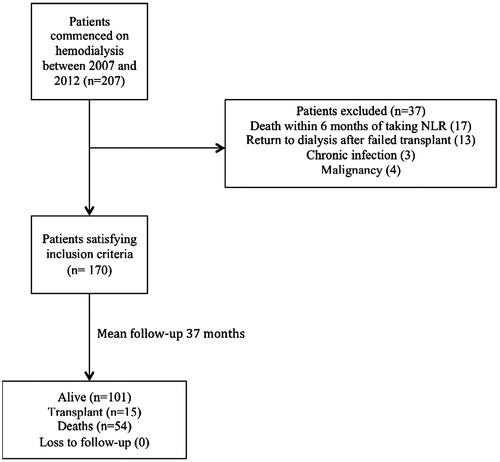
During the study period, 207 patients commenced hemodialysis of whom 37 patients were excluded (). The mean follow-up duration was 37 months, and 54 patients died during the study period (32%). Cardiovascular death was the most common cause of mortality (n = 24; 44.4%), followed by infection (n = 11; 20.4%) and treatment withdrawal (n = 11; 20.4%). Male (60%) and Indigenous patients (63%) predominated, with diabetic nephropathy being the most common underlying renal disease (69%; ). The median NLR value was 3.0 (interquartile range 2.3–3.8). Other baseline biochemical variables are summarized in . Patients with NLR value >3.0 were significantly more likely to be diabetic, have a higher white cell count and CRP, and lower hemoglobin and albumin ().
Table 1. Baseline patient characteristics.
There was a significant correlation between NLR and CRP (r = 0.24, p = 0.0023). NLR was significantly and inversely correlated with hemoglobin (r = −0.27, p = 0.00048), albumin (r = −0.23, p = 0.0034) and total cholesterol (r = −0.17, p = 0.049) levels.
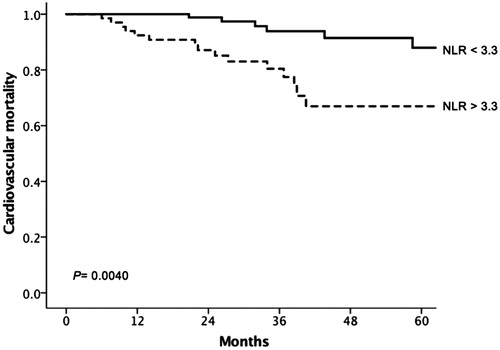
There was a significant association between increasing NLR per quartile and all-cause mortality (log-rank test, p = 0.0021; ). NLR >3.3 was associated with cardiovascular mortality compared with NLR <3.3 (log-rank test, p = 0.0040; ).
Figure 2. Kaplan–Meier estimates of cumulative overall survival rates. Patients stratified into four groups on the basis of the neutrophil–lymphocyte ratio (NLR): quartile 1 (NLR 0.85–2.34), quartile 2 (NLR 2.35–2.99), quartile 3 (NLR 3.0–3.83) and quartile 4 (NLR 3.83–12.97).
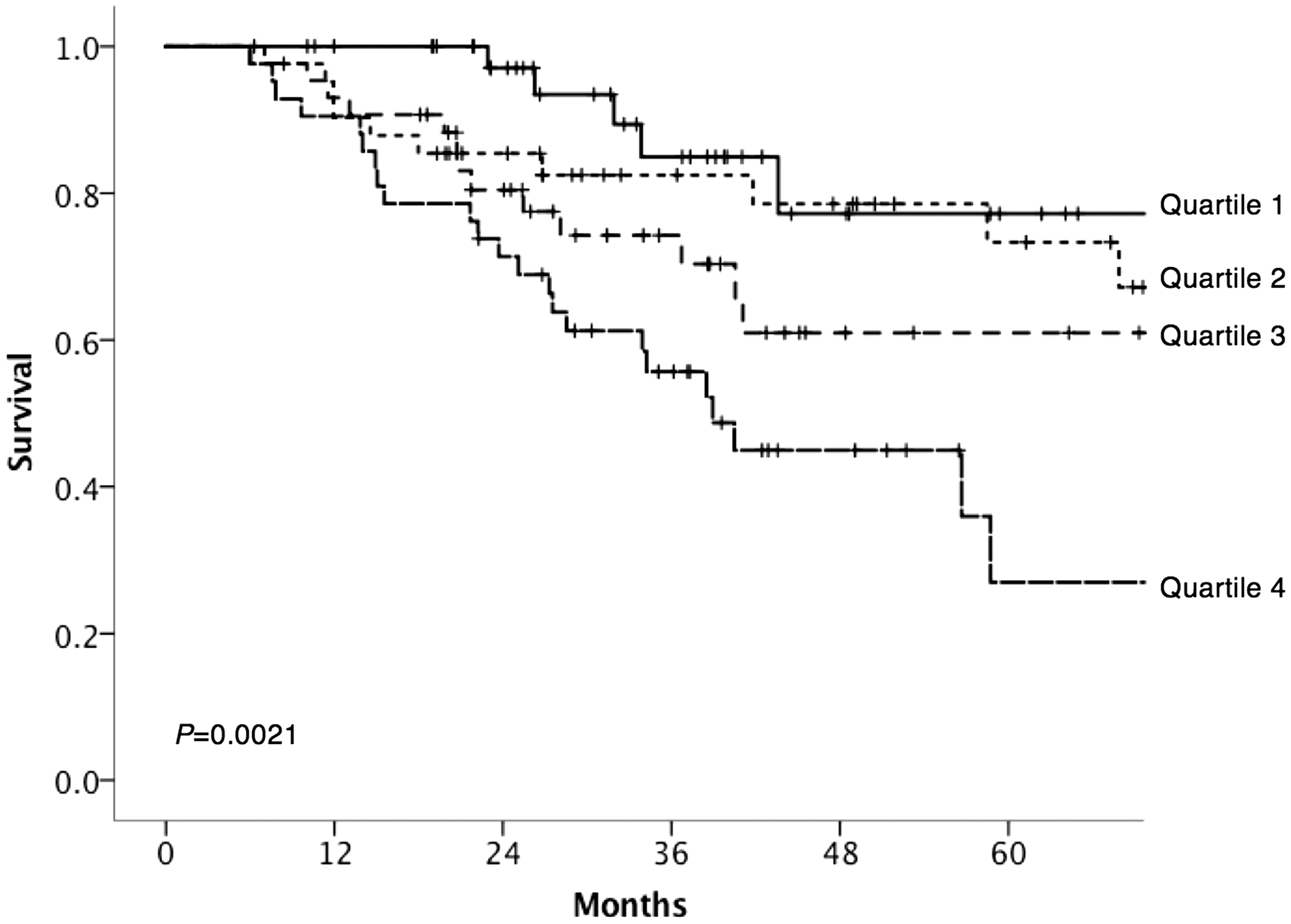
Figure 3. Kaplan–Meier estimates of cardiovascular mortality. Patients divided into two groups based on neutrophil–lymphocyte ratio (NLR) above and below 3.3.
In multivariate Cox regression, NLR was independently associated with all-cause mortality (hazard ratio [HR] 1.4; 95% confidence interval [CI], 1.2–1.6; p ≤ 0.0001). Increasing age (HR 1.6 per decade; 95% CI, 1.2–2.1; p = 0.0017), history of peripheral vascular disease (HR 2.7; 95% CI, 1.4–5.1; p = 0.0023), low BMI (HR 0.93; 95% CI, 0.88–0.98; p = 0.0047) and albumin (HR 0.91; 95% CI, 0.86–0.97; p = 0.0035) were also significantly associated with all-cause mortality ().
Table 2. Multivariate cox regression model for all-cause mortality.
In multivariate analysis of cardiovascular mortality, NLR was again a significant predictor of the outcome (HR 1.3, 95% CI 1.1–1.6, p = 0.0032), along with history of peripheral vascular disease (HR 3.7, 95% CI 1.5–8.6, p = 0.0031) ().
Table 3. Multivariate cox regression model for cardiovascular mortality.
Discussion
This is the first study conducted in incident hemodialysis patients demonstrating a significant association between NLR as a surrogate marker for systemic inflammation and both cardiovascular and all-cause mortality. Higher NLR was significantly associated with CRP and negatively correlated with hemoglobin, albumin and total cholesterol.
Several other studies have demonstrated the prognostic value of NLR in a variety of diseases in which the inflammatory response is central to the pathogenesis. The most comprehensive work on NLR has been in the setting of malignancies, including colorectal,Citation14 upper gastrointestinal,Citation15 and lung cancer,Citation16 where there is considerable interest in incorporating NLR into inflammation-based prognostic scores to aid treatment decision-making.
The prognostic value of NLR in patients with cardiovascular disease has been well documented in the general population. NLR has been shown to predict short and long-term mortality in patients with both ST and non-ST elevation myocardial infarction and in patients undergoing percutaneous coronary interventions.Citation10,Citation11,Citation17,Citation18 NLR has also been shown to be predict severity of coronary artery diseaseCitation19 and patency of bare metal stents after percutaneous coronary interventions and saphenous vein grafts after coronary artery bypass surgery.Citation20,Citation21
Despite this, relatively few studies have investigated the NLR in patients with chronic kidney disease. These studies demonstrated that NLR is associated with other inflammatory markers such as TNF-alpha and CRP along with lower hemoglobin, albumin and total cholesterol.Citation5,Citation6,Citation22 Lower total cholesterol and albumin are likely to reflect a combination of nutritional status and chronic inflammation in hemodialysis patients. The associations between NLR and CRP as well as lower hemoglobin, albumin and cholesterol in the present study are in keeping with published literature.
Inflammation also plays a key role in the initiation and progression of atherosclerosis, where atherosclerotic related cardiovascular events remains one of the most common causes of mortality in dialysis patients.Citation23 One previous study reported that NLR >3.5 was associated with an increase in the risk of cardiovascular and all-cause mortality in peritoneal dialysis patents.Citation13 Two studies have subsequently reported NLR >3.76 and 3.72 to be significant and independent (of CRP) predictors of cardiovascular events in pre-dialysis and dialysis-dependent patients, respectively.Citation12,Citation24 Our findings that an NLR >3.3 was associated with increased cardiovascular mortality therefore build on these findings in the hemodialysis population.
There are several potential mechanisms that may explain the relationship between NLR and atherosclerosis. Neutrophils have been shown to play a direct role in early endothelial dysfunction, atherogenesis and plaque destabilization.Citation25 Activated neutrophils have an increased tendency to adhere and penetrate the vascular endothelium and are involved in the release of reactive oxygen species, cytokines, and hydrolytic enzymes. In vitro studies have demonstrated that circulating neutrophil counts correlated with atherosclerotic lesion formation and that depletion of neutrophils was associated with a reduction in lesions.Citation26 Lymphopenia has also been shown to be associated with progression of atherosclerosis and adverse cardiovascular outcomes.Citation27 This may be related to lymphocyte apoptosis in atherosclerotic lesions or simply a reflection of cortisol induced stress response.Citation10,Citation28 Some have hypothesized that NLR may reflect increased sympathetic drive and therefore oxidative stress and cytokine production because of the possible influence of the autonomic nervous system on leukocyte subtype distribution.Citation29
Findings from this current study have potential implications for routine monitoring of inflammation in hemodialysis patients. There is an abundance of evidence demonstrating the association between CRP and mortality in dialysis patients, however no randomized-trials have demonstrated the advantage of regular CRP monitoring in dialysis units.Citation1 To the best of our knowledge, there are also none investigating the cost effectiveness of such practice. Despite this, routine monitoring of CRP is commonplace in many dialysis units. In contrast, NLR can simply be calculated from a patient’s full blood count, which is less costly compared with other inflammatory markers such as IL-6, TNF-alpha and CRP. In practice, this could mean that an NLR above a certain value might prompt additional investigations to determine the underlying cause(s) of inflammation and initiate treatment, similar to CRP.Citation1 However this is not entirely evidence-based suggestion, as there are no randomized trials targeting a decrease in inflammation to improve in clinical outcomes in dialysis patients.Citation30
The interpretation of our results is however challenged by several study limitations. We used single rather than serial measurements of NLR, which did not account for variations in patients’ inflammatory burden over time. Metabolic and inflammatory markers and lipid profiles were not always taken at the same time in each patient, so differences in time period between these measurements could have reduced the validity of the biochemical associations described. The effect of other unmeasured confounding factors, such as medications, remains unadjusted. Furthermore, the data pertaining to comorbid conditions were restricted to information available through the ANZDATA Registry. As such, more detailed information that could have impacted on the risk of cardiovascular events, including history of congestive cardiac failure and valvular heart disease could not be incorporated as part of analysis. A strength of this study was the significant representation of Indigenous subjects, which was not independently associated with mortality, increasing the generalizability of the model.
In summary, the NLR is a practical, cost-efficient and easy to use predictor of cardiovascular and all-cause mortality in hemodialysis patients. This is the first study to clearly demonstrate an association between NLR and cardiovascular and all-cause mortality in incident hemodialysis patients. However, there is a need for larger, prospective studies to investigate NLR in patients with chronic kidney disease prior to its implementation in clinical practice. These should aim to validate the role of NLR as a predictor of major cardiovascular events including cardiovascular mortality and to identify expected biological variation in its levels and reference ranges above which the associated adverse risks are heighted.
Acknowledgments
Parts of the data reported here have been supplied by the Australia and New Zealand Dialysis and Transplant Registry (ANZDATA). The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the Australia and New Zealand Dialysis and Transplant Registry.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
References
- Meuwese CL, Stenvinkel P, Dekker FW, Carrero JJ. Monitoring of inflammation in patients on dialysis: Forewarned is forearmed. Nat Rev Nephrol. 2011;7:166–176
- Stenvinkel P, Ketteler M, Johnson RJ, et al. IL-10, IL-6, and TNF-alpha: Central factors in the altered cytokine network of uremia-the good, the bad, and the ugly. Kidney Int. 2005;67:1216–1233
- Snaedal S, Heimbürger O, Qureshi AR, et al. Comorbidity and acute clinical events as determinants of C-reactive protein variation in hemodialysis patients: Implications for patient survival. Am J Kidney Dis. 2009;53:1024–1033
- Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32:2045–2051
- Turkmen K, Guney I, Yerlikaya FH, Tonbul HZ. The relationship between neutrophil-to-lymphocyte ratio and inflammation in end-stage renal disease patients. Ren Fail. 2012;34:155–159
- Okyay GU, İnal S, Öneç K, et al. Neutrophil to lymphocyte ratio in evaluation of inflammation in patients with chronic kidney disease. Ren Fail. 2013;35:29–36
- Guthrie GJK, Charles KA, Roxburgh CSD, et al. The systemic inflammation-based neutrophil-lymphocyte ratio: Experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88:218–230
- Chan C, Puckridge P, Ullah S, et al. Neutrophil-lymphocyte ratio as a prognostic marker of outcome in infrapopliteal percutaneous interventions for critical limb ischemia. J Vasc Surg. 2014;60:661–668
- Erturk M, Cakmak HA, Surgit O, et al. The predictive value of elevated neutrophil to lymphocyte ratio for long-term cardiovascular mortality in peripheral arterial occlusive disease. J Cardiol. 2014;64:371–376
- Tamhane UU, Aneja S, Montgomery D, et al. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102:653–657
- Park JJ, Jang H-J, Oh I-Y, et al. Prognostic value of neutrophil to lymphocyte ratio in patients presenting with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2013;111:636–642
- Solak Y, Yilmaz MI, Sonmez A, et al. Neutrophil to lymphocyte ratio independently predicts cardiovascular events in patients with chronic kidney disease. Clin Exp Nephrol. 2013;17:532–540
- An X, Mao H-P, Wei X, et al. Elevated neutrophil to lymphocyte ratio predicts overall and cardiovascular mortality in maintenance peritoneal dialysis patients. Int Urol Nephrol. 2012;44:1521–1528
- Seligmann J, Hall P, Wilson H, et al. Role of derived neutrophil lymphocyte ratio as a biomarker in advanced colorectal cancer. Lancet. 2014;383:S96
- Shimada H, Takiguchi N, Kainuma O, et al. High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer. Gastric Cancer. 2010;13:170–176
- Tomita M, Shimizu T, Ayabe T, et al. Preoperative neutrophil to lymphocyte ratio as a prognostic predictor after curative resection for non-small cell lung cancer. Anticancer Res. 2011;31:2995–2998
- Duffy BK, Gurm HS, Rajagopal V, et al. Usefulness of an elevated neutrophil to lymphocyte ratio in predicting long-term mortality after percutaneous coronary intervention. Am J Cardiol. 2006;97:993–996
- Azab B, Zaher M, Weiserbs KF, et al. Usefulness of neutrophil to lymphocyte ratio in predicting short- and long-term mortality after non-ST-elevation myocardial infarction. Am J Cardiol. 2010;106:470–476
- Kaya H, Ertaş F, İslamoğlu Y, et al. Association between neutrophil to lymphocyte ratio and severity of coronary artery disease. Clin Appl Thromb Hemost. 2012;20:50–54
- Taşoğlu İ, Turak O, Nazli Y, et al. Preoperative neutrophil-lymphocyte ratio and saphenous vein graft patency after coronary artery bypass grafting. Clin Appl Thromb Hemost. 2014;20:819–824
- Turak O, Ozcan F, Isleyen A, et al. Usefulness of the neutrophil-to-lymphocyte ratio to predict bare-metal stent restenosis. Am J Cardiol. 2012;110:1405–1410
- Malhotra R, Marcelli D, von Gersdorff G, et al. Relationship of neutrophil-to-lymphocyte ratio and serum albumin levels with C-reactive protein in hemodialysis patients: Results from 2 international cohort studies. Nephron. 2015;130:35–42
- Johnson DW, Dent H, Hawley CM, et al. Association of dialysis modality and cardiovascular mortality in incident dialysis patients. Clin J Am Soc Nephrol. 2009;4:1620–1628
- Abe T, Kato S, Tsuruta Y, et al. Neutrophil/Lymphocyte ratio as a predictor of cardiovascular events in incident dialysis patients: A Japanese prospective cohort study. Clin Exp Nephrol. 2014;19:718–24
- Soehnlein O. Multiple roles for neutrophils in atherosclerosis. Circ Res. 2012;110:875–888
- Drechsler M, Megens RTA, van Zandvoort M, et al. Hyperlipidemia-triggered neutrophilia promotes early atherosclerosis. Circulation. 2010;122:1837–1845
- Nunez J, Minana G, Bodi V, et al. Low lymphocyte count and cardiovascular diseases. Curr Med Chem. 2011;18:3226–3233
- Núñez J, Sanchis J, Bodí V, et al. Relationship between low lymphocyte count and major cardiac events in patients with acute chest pain, a non-diagnostic electrocardiogram and normal troponin levels. Atherosclerosis. 2009;206:251–257
- Park B-J, Shim J-Y, Lee H-R, et al. Relationship of neutrophil-lymphocyte ratio with arterial stiffness and coronary calcium score. Clin Chim Acta. 2011;412:925–929
- González-Espinoza L, Rojas-Campos E, Medina-Pérez M, et al. Pentoxifylline decreases serum levels of tumor necrosis factor alpha, interleukin 6 and C-reactive protein in hemodialysis patients: Results of a randomized double-blind, controlled clinical trial. Nephrol Dial Transplant. 2011;27:2023–2028