Abstract
Objective: In this retrospective matched-cohort study, the association between potassium supplementation and long-term outcomes was determined.
Methods: Chronic peritoneal dialysis (PD) patients, aged ≥ 16 years, being referred to four PD centers in China, with serum potassium levels ≤ 3.5 mEq/L on three consecutive monthly in Q4 2008 and without receiving oral potassium supplementation in the prior three months were included in this study. Patients were divided into two groups, either to receive (test group) or not (control group) oral potassium supplementation in both Q4 2008 and the subsequent follow-up period, until 31 December 2014. The patients from the test group were matched to those from the control group using a propensity score. The clinical outcomes for all-cause and cardiovascular mortality were estimated by Matched Cox regression models during 61.5 months of median follow-up. All patients were also categorized according to serum potassium correction levels (<3.0, 3.0 to <4.0, 4.0 to <5.0 and ≥5.0 mEq/L) after the whole follow-up. The hazard ratios (HRs) were used to assess the relationship between corrected potassium levels and all-cause and cardiovascular mortality in PD patients. Subgroup analysis was used to determine the homogeneity of the associations between potassium supplementation and all-cause mortality.
Results: All-cause mortality occurred in 108 patients (605/10,000 person-years) in the test group and 114 patients (677/10,000 person-years) in the control group during 1786- and 1685-year follow-up, respectively [hazard ratio (HR), 0.89; 95% confidence interval (CI), 0.68–1.16; p = 0.38]. Cardiovascular mortality occurred in 97 patients (542/10,000 person-years) in the test group and 101 patients (598/10,000 person-years) in the control group (HR, 0.89; 95% CI, 0.67–1.18; p = 0.43). There were no significant interactions between potassium supplementation and any of the subgroups, except for diabetes mellitus and volume overload. During a median follow-up of 61.5 months, adjusted all-cause mortality hazard ratio (HR) and 95% confidence interval (CI) for corrected serum potassium of <3.0, 3.0 to < 4.0, and ≥5.0 mEq/L, compared with 4.0 to < 5.0 mEq/L (reference), were 2.23 (1.17–3.72), 1.35 (0.89–1.81), and 1.74 (1.05–3.72), respectively.
Conclusion: The use of potassium supplementation in chronic PD patients is not associated with mortality. While it may be necessary for the correction of hypokalemia or the maintenance of normokalemia, and the consequent reduction of hypokalemia-associated mortality. Additionally, use of aldosterone antagonists may be preferable for the handling of hypokalemia in PD patients.
Introduction
Hypokalemia is generally defined as serum potassium level less than 3.5 mEq/L (K), on three consecutive monthly measurements, or require potassium supplementation to maintain a normal serum potassium level.Citation1 Hypokalemia is common in chronic peritoneal dialysis (PD) patients with end-stage renal disease (ESRD) and its prevalence is about 16-60%.Citation2–4 Several factors contribute to that higher occurrence, and more specifically, differences in dietary potassium consumption, if PD patients may be instructed to restrict K-rich foods, increased loss through the dialysate, enhanced removal from the large intestine, or the contest of use of non-K-sparing diuretics. Moreover, hypokalemia in PD patients could be due to a shift of potassium into the intracellular space, probably because of insulin release during the continuous dwell of the glucose-containing dialysis solution. Because of overload volume, the effect of dilution can also result in hypokalemia in PD patients. It should be mentioned that the common potassium losses in PD patients cannot exceed 52 mEq/d, while the average daily intakes of potassium in the adult US population range from 54 to 86 mEq/d. Thus, dialysate potassium losses are insufficient to induce hypokalemia in most US patients and likely require the presence of other factors, such as inadequate dietary intakes and/or transcellular shifts induced by insulin releasing from absorption of glucose from peritoneal dialysate. But, it was found from a present study that the adult Chinese diet had lower daily intakes of potassium compared to the adult US diets.Citation5
Hypokalemia is associated with poor outcomes including malnutrition, higher cardiac morbidity, and mortality ratesCitation6 as it could affect myocardial resting membrane potential, repolarization and relative refractory times, as well as conduction velocity.Citation7 According to clinical experience and small, single-center studies, the more increased incidence of hypokalemia was found in PD patients than in HD patients,Citation8 which results in the requirement for the entry to potassium supplementation for chronic PD patients. Oral potassium supplementation is often used to correct hypokalemia and maintain normokalemia in chronic PD patients with low serum K levels. However, the long-term effects of potassium supplementation on outcomes in chronic PD patients are unknown. We pursue the hypothesis that potassium supplementation does have a mortality benefit among chronic PD patients with ESRD. We created a propensity-matched cohort of patients receiving and not receiving potassium supplementation to identify the associations of potassium supplementation with mortality and hospitalization in chronic PD patients with ESRD.
Materials and methods
Study patients
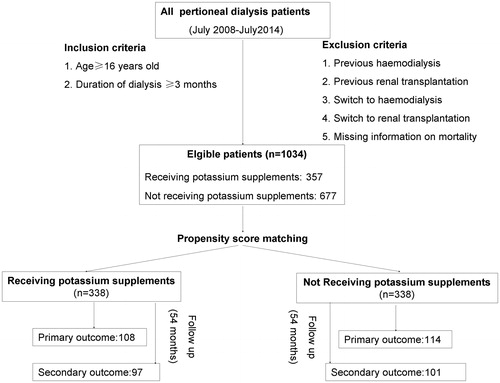
Chronic peritoneal dialysis patients (older than 16 years), being referred to four PD centers in China, with serum potassium levels ≤3.5 mEq/L on three consecutive monthly in Q4 2008 and without receiving oral potassium supplementation in the prior three months were included in this study. Patients were divided into two groups, either to receive (test group) or not (control group) oral potassium supplementation in both Q4 2008 and the subsequent follow-up period, until 31 December 2014. The 53 patients with missing information on mortality were excluded. Overall, 1174 patients were included in the final analysis, including 507 (43.2%) receivers and 667 (56.8%) non-receivers of potassium supplementation. The study was approved by the Ethics Committee of each hospital.
Study method
All patients were also categorized according to serum potassium correction levels (<3.0, 3.0 to <4.0, 4.0 to <5.0 and ≥5.0 mEq/L), since it could be important to determine to what extent the serum potassium correction occurred, as this could be a possible determining factor for all-cause and cardiovascular mortality in PD patients.Citation9
The three initial serum potassium measurements, apart from definition issues were of great importance, since there was a U-shaped relationship between time-averaged serum potassium and all-cause and cardiovascular mortality in PD-treated patients.Citation10 Meanwhile, serum potassium levels were measured at anytime when a discomfort of suspected cardial origin(such as palpitation) occurred. For the purpose of this analysis, the following demographic and clinical data were included: age, sex, causes of ESRD, duration of PD, diabetes status, dialysis adequacy (KT/V), history of cardio-cerebrovascular (CCV) disease (including congestive heart failure, ischemic heart disease, cerebrovascular disease, and peripheral artery disease), and the Charlson comorbidity index (CCI).Citation11 To reduce potential confounding and treatment selection bias, we adjusted significant difference in baseline covariates with the use of propensity score matching (PSM).Citation12–15 We matched receivers of potassium supplementation with non-receivers with similar propensity of potassium reception. An absolute standardized difference (ASD) of 0% would suggest no residual bias and ASD < 10% suggests negligible bias. In the last, 338 receivers of potassium supplementation in a test group and 338 non-receivers in a control group were included in the current analysis through PSM ().
Study outcomes
The clinical outcome was all-cause mortality and secondary outcomes included mortality due to cardiovascular causes.
Statistical analysis
The results were expressed as mean ± standard deviation (SD) and p < 0.05 was considered significant (α = 0.05 in two-tailed). For descriptive analyses, we used Pearson’s Chi square and Wilcoxon rank-sum tests for prematch comparison, and McNemar’s test and paired sample t-test for post-match comparison, as appropriate. The Kaplan–Meier plots and matched Cox regression analysis were used to estimate associations of potassium supplementation with all-cause and cardiovascular deaths in the matched cohort. Formal sensitivity analyses were conducted to determine the effect of a potential hidden confounder on our study findings.
Subgroup analyses were conducted to determine the homogeneity of the associations between potassium supplementation and all-cause mortality. We calculated absolute risk differences, and then estimated the effect of potassium supplementation on mortality in each subgroup using a Cox regression model. Odds ratios and 95% confidence intervals (95% CIs) were calculated by means of logistic regression models for the mortality of different level of corrected serum potassium, with adjustment for age, sex, BMI, etiology of ESRD, diabetic status, duration of dialysis, Total Kt/v urea and the Charlson comorbidity index. All statistical tests were evaluated using two-tailed 95% confidence interval (CI) using SPSS 18.0 for Windows (IBM Corporation, Armonk, NY).
Results
Patient characteristics
Patients (n = 676) with a mean age 53.7(±11.3) years old and 58.7% males were included in our study. The median follow-up time was 63.7 months in the test group and 59.8 months in the control group. There were significant pre-match imbalances in key baseline covariates, including age, sex, etiology of ESRD, diabetes mellitus, mean plasma K level, mean plasma high sensitive C-reactive protein (Hs-CRP) level, and CCI, all of which were balanced after matching (). All ASDs were below 10%.
Table 1. Baseline characteristics of potassium supplementation and no potassium supplementation, before and after propensity score matchingTable Footnotea.
Potassium supplementation and mortality
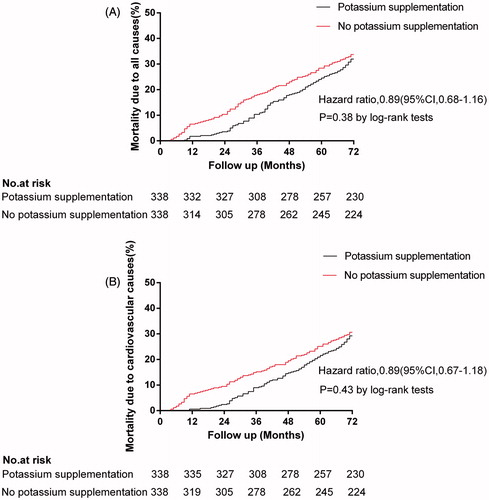
During a median follow up of 61.5 months, 222 (32.8%) patients died from all causes, with 198 (29.3%) due to cardiovascular causes. All-cause mortality occurred in 108 patients (605/10,000 person-years) in the test group and 114 patients (677/10,000 person-years) in the control group during 1786- and 1685-year follow-up, respectively (HR, 0.89; 95% CI, 0.68–1.16; p = 0.38]. Cardiovascular mortality occurred in 97 patients (542/10,000 person-years) in the test group and 101 patients (598/10,000 person-years) in the control group (HR, 0.89; 95% CI, 0.67–1.18; p = 0.43, ).
Figure 2. The Kaplan–Meier plots for all-cause mortality and cardiovascular mortality by the use of oral potassium supplementation.
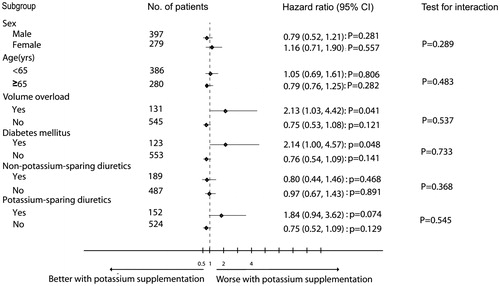
In subgroup analyses, the associations between potassium supplementation and all-cause mortality were observed in a wide spectrum of chronic PD patients (). There was no significant interaction between potassium supplementation and any of the subgroups, except for diabetes mellitus and volume overload (p = 0.048 and 0.041, respectively).
The relationship between hypokalemia correction and all-cause and cardiovascular mortality was also U-shaped, with lowest mortality rates observed in patients with potassium levels of 4.0 to 5.0 mEq/L and highest in that of potassium < 3.0 mEq/L. Both all-cause and cardiovascular mortality rates were higher for potassium levels of ≥5.0 mEq/L, compared with those with levels between 4.0 and 5.5 mEq/L. After adjustments, the risk of all-cause and cardiovascular mortality rates was significant in those with potassium of <3.0 mEq/L [adjusted HR for all-cause mortality rate, 2.23 (1.17–3.72); adjusted HR for cardiovascular mortality rate, 2.18 (1.18–4.31), respectively] and >5.0 mEq/L [adjusted HR for all-cause mortality rate, 1.74 (1.05–3.72); adjusted HR for cardiovascular mortality rate, 1.89 (1.11–3.95), respectively], shown in .
Table 2. The relationship between hypokalemia correction and all-cause and cardiovascular mortality.
Discussion
Our results demonstrate that in chronic PD patients who were well-balanced in all measured baseline covariates, potassium supplementation was not associated with an increased risk of mortality due to all causes or cardiovascular causes. But we did find an U-shaped association of hypokalemia and all-cause and cardiovascular mortality rates in PD patients, with the highest mortality rate observed for potassium levels <3.0 mEq/L, which was somewhat consistent with previous study. To the best of our knowledge, this is the first study reporting an association between potassium supplementation and long-term outcomes in a propensity score matching cohort of chronic PD patients with ESRD.
As reported previously,Citation16,Citation17 serum potassium level <4 mEq/L was associated with an increased mortality, but oral potassium supplementation is also not associated with an increased risk of mortality due to all causes or cardiovascular causes among chronic heart failure patients. These results suggest that hypokalemia-associated mortality was eliminated in receivers of potassium supplementation via the correction of hypokalemia. In the present study, hypokalemia-associated mortality, including fatal cardiac arrhythmias, sudden cardiac death, and respiratory myoparalysis were investigated. Our results suggest that potassium supplementation did neutralize the hypokalemia-associated excess deaths, but did not additionally reduce mortality. The reasons were as follows: first, use of non-potassium-sparing diuretics is an important cause of low-serum potassium level for chronic HF patients. The causes of hypokalemia for chronic PD patients are multifactorial. We do not know whether or not hypokalemia has a direct effect on the increase of mortality rate or is just a surrogate marker of comorbidities despite the good quality of previous studies. Nevertheless, hypokalemia is frequently associated with conditions that are known risk factors for poor outcomes, such as malnutrition,Citation18,Citation19 inflammation (peritonitis or PD-non related infections),Citation20,Citation21 hypomagnesemia and hyponatremia in PD patients. Malnutritional conditions (assessed by mean plasma albumin and mean plasma pre-albumin levels) could not be totally corrected by single potassium supplementation, which was seen in the present study. Second, PD-non-related infections, were the main cause of death, followed by cardiovascular diseaseCitation22 in PD patients. But it was found that there were no variations in the incidence of infections (assessed by Hs-CRP, data were not shown), after potassium supplementation. At the same time, potassium supplementation for PD patients with hypokalemia may be theoretically be reviewed as providing better care in other domain and supplemented hypokalemia patients may be less likely to achieve normokalemia with diet compared to non-supplemented hypokalemia patients.
Subgroup analyses suggest that potassium supplementation is significantly associated with increased all-cause mortality with the complication of diabetes mellitus (). Higher frequency of hypokalemia in diabetic PD-treated patients is explained by insulin actions together with continuous peritoneal glucose absorption, which could both promote an excess of potassium redistribution into the intracellular compartment by activating Na+-K+-ATPase, thus resulting in active potassium uptake. For that reason, potassium supplementation could result in potential increase of serum potassium level. We also observed potassium supplementation-associated increase of all-cause mortality with the complication of volume overload (). The reason for hypokalemia among the patients with volume overload is an effect of dilution. Clinical studies suggest that hyperkalemia is associated with an increased risk of cardiovascular mortality. Thus, hyperkalemia, rather than hypokalemia, is a reason for concern for adverse outcomes in these patients. It was suggested that aldosterone antagonists may be preferable over chronic potassium supplementation for maintenance of normokalemia once hypokalemia has been corrected.Citation13 Our subgroup analyses also suggest that reception of potassium-sparing diuretics is associated with a trend of increased mortality when using potassium supplementation (p = 0.074, ). Spironolactone may improve hypokalemia, while the risk of severe hyperkalemia is not significantly elevated among PD patients.Citation23 Nevertheless, when selecting potassium supplementation, spironolactone 25 mg/day does not have a significant effect on serum potassium or urine and peritoneal excretion rate in PD patients, who have a history of hypokalemia.Citation24
Our study has several limitations. Firstly, propensity matching may not be able to balance unmeasured confounders. Even though the presence of such an unmeasured confounder cannot be confirmed by sensitivity analysis, our main conclusions may be sensitive to a hidden confounder. However, for any unmeasured or hidden covariate to become a confounder, it must be strongly associated with both potassium supplementation and mortality, but not with any of the covariates used in the propensity score model. Secondly, small sample size in addition to limited racial diversity of the study would be severely underpowered to draw the concise conclusion. Finally, because of lack of data on serum magnesium, we do not know to what extent the observed effect may be caused by low magnesium.
Conclusions
The use of potassium supplementation in chronic PD patients is not associated with mortality. While it may be necessary for the correction of hypokalemia or the maintenance of normokalemia, and the consequent reduc-tion of hypokalemia-associated mortality. Additionally, use of aldosterone antagonists may be preferable for the handling of hypokalemia in PD patients.
Disclosure statement
The authors have no financial conflicts of interest to declare.
Funding
This study was supported by Guangzhou Medical Key Subject Construction Project (2013–2015).
References
- Katerinis I, Fumeaux Z. [Hypokalemia: Diagnosis and treatment]. Rev Med Suisse. 2007;3:579–582.
- Zanger R. Hyponatremia and hypokalemia in patients on peritoneal dialysis. Semin Dial. 2010;23:575–580.
- Tziviskou E, Musso C, Bellizzi V, et al. Prevalence and pathogenesis of hypokalemia in patients on chronic peritoneal dialysis: One center's experience and review of the literature. Int Urol Nephrol. 2003;35:429–434.
- Szeto CC, Chow KM, Kwan BC, et al. Hypokalemia in Chinese peritoneal dialysis patients: Prevalence and prognostic implication. Am J Kidney Dis. 2005;46:128–135.
- Zhang R, Wang Z, Fei Y, et al. The difference in nutrient intakes between Chinese and Mediterranean, Japanese and American diets. Nutrients. 2015;7:4661–4688.
- Kwan BC, Szeto CC. Dialysis: Hypokalaemia and cardiac risk in peritoneal dialysis patients. Nat Rev Nephrol. 2012;8:501–503.
- Alper AB, Campbell RC, Anker SD, et al. A propensity-matched study of low serum potassium and mortality in older adults with chronic heart failure. Int J Cardiol. 2009;137:1–8.
- Choi HY, Ha SK. Potassium balances in maintenance hemodialysis. Electrolyte Blood Press. 2013;11:9–16.
- Xu Q, Xu F, Fan L, et al. Serum potassium levels and its variability in incident peritoneal dialysis patients: Associations with mortality. PLoS One. 2014;9:e86750.
- Torlen K, Kalantar-Zadeh K, Molnar MZ, Vashistha T, Mehrotra R. Serum potassium and cause-specific mortality in a large peritoneal dialysis cohort. Clin J Am Soc Nephrol. 2012;7:1272–1284.
- Liu J, Huang Z, Gilbertson DT, Foley RN, Collins AJ. An improved comorbidity index for outcome analyses among dialysis patients. Kidney Int. 2010;77:141–151.
- Lee J, An JN, Hwang JH, et al. Effect of dialysis initiation timing on clinical outcomes: A propensity-matched analysis of a prospective cohort study in Korea. PLoS One. 2014;9:e105532.
- Iimori S, Mori Y, Akita W, et al. Effects of sevelamer hydrochloride on mortality, lipid abnormality and arterial stiffness in hemodialyzed patients: A propensity-matched observational study. Clin Exp Nephrol. 2012;16:930–937.
- Wilson FP, Yang W, Machado CA, et al. Dialysis versus nondialysis in patients with AKI: A propensity-matched cohort study. Clin J Am Soc Nephrol. 2014;9:673–681.
- Lee JE, Oh KH, Choi KH, et al. Statin therapy is associated with improved survival in incident peritoneal dialysis patients: Propensity-matched comparison. Nephrol Dial Transplant. 2011;26:4090–4094.
- Ekundayo OJ, Adamopoulos C, Ahmed MI, et al. Oral potassium supplement use and outcomes in chronic heart failure: A propensity-matched study. Int J Cardiol. 2010;141:167–174.
- Ahmed A, Zannad F, Love TE, et al. A propensity-matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J. 2007;28:1334–1343.
- Blumenkrantz MJ, Kopple JD, Moran JK, Coburn JW. Metabolic balance studies and dietary protein requirements in patients undergoing continuous ambulatory peritoneal dialysis. Kidney Int. 1982;21:849–861.
- Jung JY, Chang JH, Lee HH, Chung W, Kim S. De novo hypokalemia in incident peritoneal dialysis patients: A 1-year observational study. Electrolyte Blood Press. 2009;7:73–78.
- Chuang YW, Shu KH, Yu TM, Cheng CH, Chen CH. Hypokalaemia: An independent risk factor of Enterobacteriaceae peritonitis in CAPD patients. Nephrol Dial Transplant. 2009;24:1603–1608.
- Shu KH, Chang CS, Chuang YW, et al. Intestinal bacterial overgrowth in CAPD patients with hypokalaemia. Nephrol Dial Transplant. 2009;24:1289–1292.
- Ribeiro SC, Figueiredo AE, Barretti P, Pecoits-Filho R, de Moraes TP. Low serum potassium levels increase the infectious-caused mortality in peritoneal dialysis patients: A propensity-matched score study. PLoS One. 2015;10:e0127453.
- Ito Y, Mizuno M, Suzuki Y, et al. Long-term effects of spironolactone in peritoneal dialysis patients. J Am Soc Nephrol. 2014;25:1094–1102.
- Yongsiri S, Thammakumpee J, Prongnamchai S, et al. Randomized, double-blind, placebo-controlled trial of spironolactone for hypokalemia in continuous ambulatory peritoneal dialysis patients. Ther Apher Dial. 2015;19:81–86.