Sir,
We read with interest the recent prospective cohort study by Sun et al. on the association of intraoperative hypotension (IOH) with acute kidney injury (AKI) after elective non-cardiac surgery in the journal, Anesthesiology.Citation1 AKI occurred in 324 (6.3%) patients and was associated with mean arterial pressure (MAP) < 60 mmHg for 11–20 min, and MAP <50 mmHg for more than 10 min in a graded fashion.Citation1 The adjusted odds ratio of AKI for MAP less than 55 mmHg was 2.34 (1.35–4.05) for 11–20-min exposure and 3.53 (1.51–8.25) for more than 20 min.Citation1 For MAP, less than 60 mmHg, the adjusted odds ratio for AKI was 1.84 (1.11–3.06) for 11–20-min exposure.Citation1 This was a well-designed and large study, involving a retrospective cohort study of 5127 patients undergoing non-cardiac surgery with invasive MAP monitoring and length of stay of 1 or more days in the hospital.Citation1 The authors then concluded that the study provided an impetus for clinical trials to determine whether interventions to promptly treat IOH tailored to individual patient physiology could help reduce the risk of AKI.Citation1
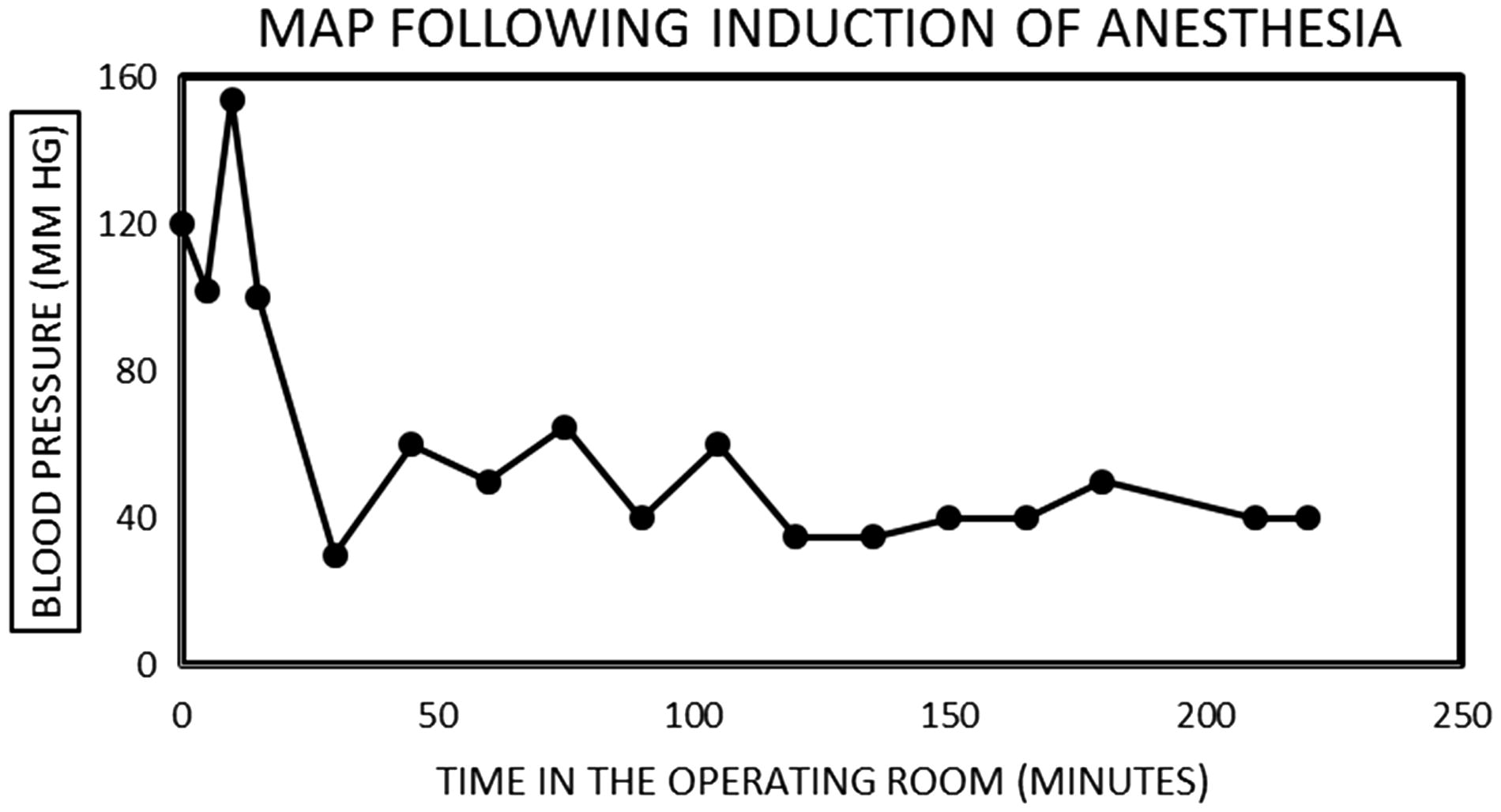
We recently reported on the role of IOH as a neglected causative factor in hospital-acquired AKI.Citation2 Notably, in the AKI-surgery literature, there has existed for a long time, this generally held consensus that IOH following hypotensive anesthesia or controlled hypotension (CH) in the operating room has no significant short-term and long-term impacts on renal function.Citation3–5 We showed in our recent paper published in the journal, Journal of Renal Injury Prevention, the clear association of IOH with the causation of AKI in two patients managed in the Mayo Clinic Health System in Northwestern Wisconsin.Citation2 Sun et al. had furthermore acknowledged the complex and heterogeneous nature of individual patients’ physiology in response to different anesthetic techniques, further complicating the relationship between MAP and AKI in the perioperative setting.Citation1 Indeed, in our first case presentation, a 46-year-old male patient who underwent right hip arthroplasty, with preoperative hypertension and CKD III, MAP preoperatively was up to 120 mmHg, but had dropped precipitously to as low as 40 mmHg within half an hour of induction of anesthesia in the operating room and his MAP generally remained in the 40–50 mmHg range for several hours throughout the surgical procedure ().Citation2
Whereas Sun et al. had demonstrated a long list of other risk factors associated with AKI, we agree with the authors that blood pressure (BP) was one of the very few modifiable intraoperative risk factors for adverse outcomes in the perioperative setting. We would rather propose the avoidance of IOH rather than developing new strategies to treat IOH, as suggested by Sun et al. Prevention is far way better, and cheaper, than cure.Citation2,Citation6,Citation7 We posit that the avoidance of IOH, with preferably higher floors for intraoperative BP (MAP >70 mmHg) especially in older (>65-year-old) later stage CKD (≥ stage III) patients, as well as the preemptive withdrawal of nephrotoxic agents, about 3–5 d before surgery would indeed go a long way toward reducing postoperative AKI in our patients.Citation2,Citation6,Citation7
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Macaulay Amechi Chukwukadibia Onuigbo
Mayo Clinic College of Medicine, Rochester, MN, USA
Department of Nephrology, Mayo Clinic Health System
Eau Claire, WI, USA
Nneoma Agbasi
North East London NHS Foundation Trust, London, UK
Received 8 October 2015; accepted 22 November 2015
References
- Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology 2015;123:515–523.
- Onuigbo MA, Agbasi N. Intraoperative hypotension – a neglected causative factor in hospital-acquired acute kidney injury; a Mayo Clinic Health System experience revisited. J Renal Inj Prev. 2015;4:61–67.
- Choi WS, Samman N. Risks and benefits of deliberate hypotension in anaesthesia: A systematic review. Int J Oral Maxillofac Surg. 2008;37:687–703.
- Thompson GE, Miller RD, Stevens WC, Murray WR. Hypotensive anesthesia for total hip arthroplasty: A study of blood loss and organ function (brain, heart, liver, and kidney). Anesthesiology 1978;48:91–96.
- Papalia R, Simone G, Ferriero M, et al. Laparoscopic and robotic partial nephrectomy with controlled hypotensive anesthesia to avoid hilar clamping: Feasibility, safety and perioperative functional outcomes. J Urol. 2012;187:1190–1194.
- Onuigbo MA. Reno-prevention vs. reno-protection: A critical re-appraisal of the evidence-base from the large RAAS blockade trials after ONTARGET – a call for more circumspection. QJM 2009;102:155–167.
- Onuigbo MA. Renoprevention: A new concept for reengineering nephrology care – an economic impact and patient outcome analysis of two hypothetical patient management paradigms in the CCU. Ren Fail. 2013;35:23–28.