Sir,
T-cell lymphoblastic lymphoma is a high-grade hematologic neoplasia requiring intensive chemotherapy similar to that employed for lymphoblastic acute leukemia based on intrathecal methotrexate (MTX), e.v. (endovenous) vincristine, daunorubicin, asparaginase/cyclophosphamide, cytarabine, 6-mercaptopurine.Citation1 The consolidation protocol for young patient employed by our Hematology Department is characterized by e.v. administration of high-dose MTX (5 g/mq).
MTX is a known potential cause of severe acute renal injury.Citation2,Citation3 One patient receiving low-dose dopamine 2–3 μg/kg bw/min infusion. Dopamine at “renal” dosage is a known glomerular vasodilator, that reduce resistances and improves renal blood flow.Citation4
Here, we present two cases of severe MTX nephrotoxicity. Case #2 was successfully treated by infusion of low-dose dopamine showing effective MTX renal clearance, resulting in a fast and complete recovery of kidney function.
Case #1. A 42-year-old male with serum creatinine (sCr) 0.84 mg/dL affected by T-cell lymphoblastic lymphoma in complete remission became eligible for consolidation with high-dose MTX. Twenty-four hours after MTX infusion, its serum levels increased to 113 μm/L and sCr initially reached 3.77 mg/dL, and soon after 5.71 mg/dL. Rescue therapy with glucarpidase was administrated with beneficial reduction of serum MTX levels and sCr to 0.94 mg/dL (). Satisfactory diuresis and neutral fluid balance avoided hemodialysis treatment.
Figure 1. Two cases of severe MTX nephrotoxicity. Case #1 was treated by glucarpidase infusion. Case #2 received low-dose dopamine 2–3 ng/kg bw/min infusion.
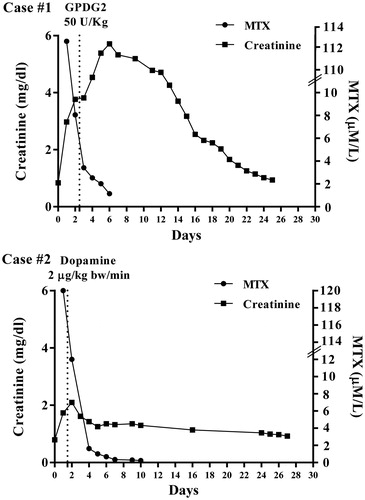
Case #2. A 22-year-old male with acute lymphoblastic leukemia in complete remission showed sCr 0.8 mg/dL. Consolidation by high-dose MTX infusion was carried out. Twenty-four hours after MTX administration, its serum levels increased to 120 μm/L and sCr to 2.1 mg/dL. “Renal” low-dose dopamine infusion () was given with beneficial progressive reduction of MTX levels and sCr to 0.92 mg/dL (). Adequate diuresis and neutral fluid balance were observed as for Case #1.
In Case #1, glucarpidase standard treatment explains the reduction of MTX and sCr levels. In Case #2, stable lower sCr encouraged a different approach aimed to increase MTX renal clearance by low-dose dopamine infusion. Our hypothesis is that resting renal reserve stimulated by low-dose dopamine provided a further renal function for MTX kidney excretion.Citation5 Both cases showed the fast lowering of serum MTX levels (). Although some evidences prove that kidney tubulesCitation3 are the main way for MTX renal clearance, its renal excretion still needs a full clarification. Future studies will explain MTX renal metabolism and the potential role of low-dose dopamine after high-dose MTX infusion. Meanwhile, in order to expose MTX high-dose infusion to a potentially improved excretion, we propose infusion of low-dose dopamine to improve MTX renal clearance during consolidation therapies.
Acknowledgments
Informed consent was obtained from all individual participants included in the study.
Declaration of interest
The authors declare that they have no conflicts of interest.
References
- Mathisen MS1, Jabbour E, Kantarjian HM. Treatment of adult acute lymphoblastic leukemia (ALL) with a focus on emerging investigational and targeted therapies. Oncology. 2012;26(9):851–859.
- Winograd B, Lippens RJ, Oosterbaan MJ, Dirks MJ, Vree TB, van der Kleijn E. Renal excretion and pharmacokinetics of methotrexate and 7-hydroxy-methotrexate following a 24-h high dose infusion of methotrexate in children. Eur J Clin Pharmacol. 1986;30(2):231–238.
- Takeuchi A, Masuda S, Saito H, Doi T, Inui K. Role of kidney-specific organic anion transporters in the urinary excretion of methotrexate. Kidney Int. 2001;60(3):1058–1068.
- Pereira CN, Machado FR, Guimarães HP, Senna AP, do Amaral JL. Hemodynamics and renal function during administration of low-dose dopamine in severely ill patients. Sao Paulo Med J. 2004;122(4):141–146.
- Thomas DM, Coles GA, Williams JD. What does the renal reserve mean? Kidney Int. 1994;45(2):411–416.
