Abstract
Importance Autosomal dominant polycystic kidney disease (ADPKD) has been associated with cardiovascular abnormalities such as intracranial and aortic aneurysms. Objective To systematically review the case reports and case series of ADPKD patients with coronary artery dissection or aneurysm. Evidence review Systematic review registration number: CRD42015015723. Data sources: MEDLINE, Web of Science and OpenGrey, reference lists of studies. Study selection: Published case reports and case series. Data extraction: Two parties analyzed the studies. Disagreements were solved by consensus or by a third party. Funding: none. Findings The reports of 23 patients (22 from 17 studies – six with coronary artery dissection and 16 with coronary artery aneurysm – and one with coronary dissection) were analyzed and reported here. Most patients were symptomatic. Coronary dissection showed female and left descending anterior artery predominance, features similar to non-ADPKD patients, but a median diagnostic age below expected (41 vs. 50 years old). Coronary aneurysms had male and right coronary artery predominance but lower median diagnostic age (44 years old) and higher rate of multiple vessel affection than reported for non-ADPKD patients. Conclusion and relevance Clinical disparities may suggest a different mechanism of aneurysm formation compared to the population without ADPKD. Nevertheless, lack of access to data of one patient and text of one article limited our conclusions. Coronary aneurysms and dissections represent a source of coronary syndromes and death in ADPKD. Mutation of ADPKD-related genes may predispose to coronary abnormalities, especially aneurysms. Further analysis regarding this association is necessary.
Introduction
Autosomal dominant polycystic kidney disease (ADPKD) is the most frequent hereditary renal cystic disease.Citation1 This monogenic disorder is caused by mutation with loss of function of one of two genes: PKD1, that encodes polycystin-1, and PKD2, that encodes polycystin-2.Citation2 PKD1 mutation is responsible for 85% of cases and PKD2 mutation for the remainder.Citation1
ADPKD is associated with a wide phenotypic range. Manifestations include renal, hepatic, pancreatic, seminal vesicle and arachnoid cysts, intracranial and aortic aneurysms, cardiac valvular abnormalities, colonic diverticula, and bronchiectasis.Citation3 Although apparently rare, arterial aneurysms and dissections on other locations, such as the coronary arteries, have also been described.Citation3
In this article, we have conducted a systematic review of case reports and series of ADPKD patients who developed coronary artery dissection or aneurysm and included the case of a patient followed in our center.
Materials and methods
Case report
The case report was prepared after patient's consent as defined by the ethical guidelines at Centro Hospitalar Lisboa Norte, Portugal. Data was gathered retrospectively from medical records. For the purposes of case reporting we used STROBECitation4 and CARE guidelines.Citation5
Systematic review
The systematic review was conducted in line with MOOSECitation6 and PRISMACitation7 statements. The study protocol was published at PROSPERO (CRD42015015723; available at: http://www.crd.york.ac.uk/PROSPERO_REBRANDING/display_record.asp?ID=CRD42015015723).
Eligibility criteria
All case reports and case series reporting original cases of pediatric and adult ADPKD patients with coronary artery dissection or aneurysm were accepted. Only published data was accepted. Other types of studies and abstract presentations, oral or poster, were excluded. There were no language or time restrictions and non-English reports were translated.
Definitions
In at-risk individuals, ADPKD diagnosis was based on the presence of: at least three renal cysts unilaterally or bilaterally in individuals between 15 and 39 years old; at least two cysts in each kidney in individuals between 40 and 59 years old; and four or more cysts in each kidney in individuals over 60 years old.Citation8
Coronary artery dissection was defined as: contrast dye staining of arterial wall with multiple radiolucent lumen; or appreciable (often subtle) abrupt change in arterial caliber, with demarcation from normal diameter to diffuse narrowing; or long (11–20 mm), hazy or linear stenosis without evidence of atherosclerotic changes in other coronary arteries.Citation9
The definition of coronary artery aneurysm or ectasia used was: focal or segmental dilation that exceeds by 50%, the diameter of healthy adjacent reference segments or vessels.Citation10 Focal or segmental dilations of inferior diameter, sometimes mentioned as “minor ectasias”, were not considered for analysis.
Data sources
Electronic database identification of reports was conducted on MEDLINE and Web of Science. Grey literature was searched via appropriate databases (i.e., OpenGrey). The last search was done on 27 December 2014. Whenever needed authors were contacted via email for further access to data. References of included studies were crosschecked.
Search strategy
The developed search strategy for all databases combined the terms “Autosomal Dominant Polycystic Kidney Disease” with “Coronary Artery Diseases OR Coronary Aneurysm OR Coronary Dissection.” A highly sensitive filter was used to avoid retrieval of non-observational studies.Citation11 Participants were restricted to humans. All terms were searched as free-text and controlled vocabulary. The reference lists of selected studies were crosschecked for additional potentially eligible studies and cited reference research was done using studies’ titles and authors.
Study selection
Reports retrieved through electronic identification were screened for eligibility by title and abstract analysis. Exclusion reasons were not recorded. The full text of potentially eligible studies was screened for appropriateness for inclusion. Exclusion reasons were recorded. Two screeners (FBR, JBN) conducted this process. Disagreements were solved by consensus or by a third party (JAL). Cohen's kappa (κ) coefficient was used to calculate inter-observer bias.Citation12
Data extraction
Two independent parties (FBR, JBN) extracted data from the included studies’ full text to an electronic form. Disagreements were solved by consensus or by a third party (JAL).
Data synthesis and analysis
The following data were extracted: surname of first author, publication year, clinical characteristics, personal and family history of extra-renal ADPKD manifestations, diagnosis of coronary dissection or aneurysm, local treatment, and outcome. Gathered data were subject to descriptive analysis.
Results
Case report
We report the case of a female Portuguese patient, with 41 years old, and a diagnosis of ADPKD with renal and hepatic cysts, without mutation analysis. Currently overweight (body mass index 28 kg/m2), the patient had normal renal function and no other cardiovascular risk factors, namely arterial hypertension. Her family history was remarkable for ADPKD: her father and brother had renal cysts but no extra-renal manifestations.
The patient was asymptomatic until 1 week before admission, when she started complaining of progressively worsening precordial discomfort with irradiation to both upper limbs. She went to see her family physician, where an electrocardiogram (EKG) was ordered. An elevation of the ST segment on DIII and aVF leads prompted the diagnosis of inferior myocardial infarction. The patient was then transferred to a central hospital, where an urgent coronary catheterization showed a co-dominant system, with 99% stenosis of the circumflex artery suggestive of either diffuse or spastic disease and 30% ostial stenosis of the right coronary artery. Balloon angioplasty was performed on the circumflex artery, with an end-thrombolysis in myocardial infarction (TIMI) flow grade of 3.
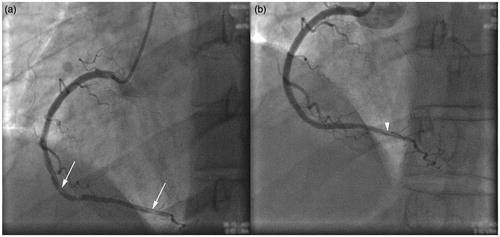
The patient remained asymptomatic for 6 days, after which anterior thoracic discomfort recurred. The EKG remained unchanged but troponin I levels raised from normal values to 2.45 ng/mL (laboratory cutoff: 0.02 ng/mL). A second coronary catheterization was performed, revealing a permeable circumflex artery despite complete right coronary artery occlusion due to dissection (). Reperfusion was accomplished after proximal placement of a drug-eluting stent under optical coherence tomography (OCT) guidance, with an end-TIMI flow grade of 3 (). Thereafter the patient became asymptomatic and troponin I levels progressively normalized.
Figure 1. Coronary angiography showing (a) proximal dissection of the right coronary artery and (b) reperfusion after proximal drug-eluting stent placement.
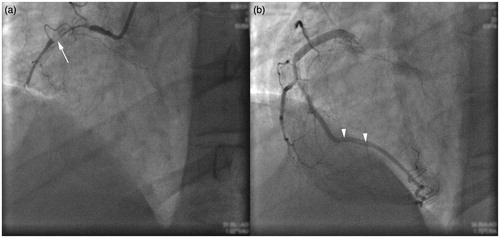
At two months of follow-up, coronary catheterization demonstrated maintenance of dissection of the right coronary artery (). Two drug-eluting stents were placed distally to the first under OCT guidance with an end-TIMI flow grade of 3, except for the distal part of the vessel, which was very thin and remained dissected (). At 6 months of follow-up, the patient remained asymptomatic.
Systematic review
Study selection
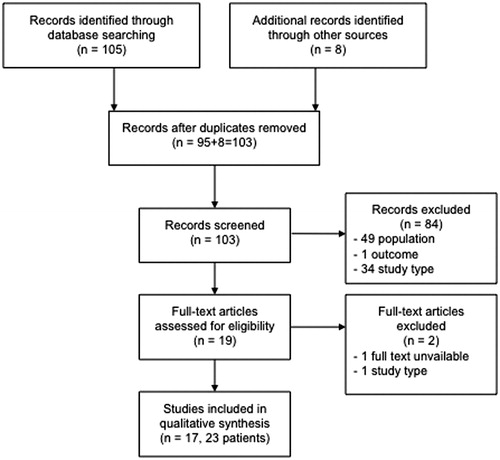
Database and manual search yielded 113 records. After duplication, 103 records were screened and 84 were discarded after title and abstract inspection due to lack of eligibility. A κ of 0.70 (95%CI 0.50–0.90) was calculated for inter-observer bias, reflecting good agreement between screeners.Citation12 Of the 19 potentially eligible studies, the full text was unavailable for one, even after contacting the first author and the journal editor. The full text of 18 potentially eligible studies was analyzed: one was excluded due to lack of eligibility criteria and 17 were included for analysis ().Citation13–29
Study characteristics
All included studies were case reports except for three case series.Citation15–17 All were in English but one that was published in Portuguese.Citation25 Publication years ranged from 1993 to 2014. The studies had widespread distribution: six in Europe (Sweden, Germany, The Netherlands, Switzerland, France, and Italy), six in Asia (Israel, China, Iran, Japan, Turkey, and Korea), and three in America (USA and Brazil) and two in Oceania (Australia).
Analysis of study participants’ characteristics
The included studies reported on 23 patients but one had insufficient data.Citation16 After unsuccessful author contact, the latter patient was excluded from analysis.
Patient data extracted from the selected studies and from the case reported in this article are summarized in and , representing a total of 23 patients: seven (30.4%) with coronary artery dissection and 16 (69.6%) with coronary artery aneurysm. Genetic status was unknown for all patients.
Table 1. Clinical characteristics of adult dominant polycystic kidney disease patients with coronary artery dissection.
Table 2. Clinical characteristics of adult dominant polycystic kidney disease patients with coronary artery aneurysm.
Manifestations, diagnosis, and treatment of ADPKD patients with coronary artery dissection
Most patients were female (n=5; 71.4%). The median age of diagnosis was 41 years (range: 36–59). Extra-renal manifestations of ADPKD were reported as follows: two patients had hepatic cysts (patients 1 and 6), one had cardiac valvulopathy (patient 2 had mitral valve prolapse and regurgitation, and tricuspid valve prolapse), and none had extra-coronary aneurysms or dissections.
End-stage renal disease (ESRD) was absent in all coronary dissection patients. Arterial hypertension was diagnosed in two patients (28.6%) and coronary atherosclerosis was described in another two patients, one of them on the same dissected artery (left anterior descending artery on patient 5). None of the cases reported association with connective tissue disorders, systemic inflammatory diseases, or the peripartum period. In one (patient 2), the use of combined hormone therapy was registered.
None of the patients had a positive family history of coronary or extra-coronary aneurysms or dissections.
All cases were symptomatic: two patients (28.6%) had angina and five (71.4%) had a myocardial infarction. The primary method of diagnosis was coronary angiography (n=7, 100%). In one case (14.3%), computer tomography coronary angiography was also diagnostic. The most frequently affected artery was the left anterior descending vessel (n=5; 71.4%).
Coronary angioplasty was conducted on four patients (57.1%), with good control of symptoms in three patients. Outcome was not reported in all patients with conservative management and in one who underwent angioplasty.
Manifestations, diagnosis, and treatment of ADPKD patients with coronary artery aneurysm
Male predominance was registered in coronary aneurysm patients (n=10; 76.9% of all patients with known gender). The median age of diagnosis was 44 years (range: 23–78). Extra-renal manifestations of ADPKD were reported as follows: four patients had hepatic cysts (patients 8, 20, 22, and 23); five had cardiac valvulopathy (patients 8 and 23 had mitral valve prolapse; patients 17, 22, and 23 had mitral regurgitation; and patients 18 and 22 had aortic regurgitation); and four had extra-coronary aneurysms (patients 18, 21, and 23 had aortic aneurysms; patient 20 had aneurysms on one renal artery; patient 23 had bilateral femoral artery aneurysms; and patient 18 had bilateral iliac artery aneurysms).
Six patients had ESRD (patients 8, 17, and 18 were transplant recipients, and patients 9, 20, and 23 were on hemodialysis). Arterial hypertension was diagnosed in five patients with coronary aneurysm (50% of all patients with reported blood pressure status). Six patients with coronary aneurysms had atherosclerosis, two of them on the same aneurysmatic artery (right coronary artery on patient 8 and right and left coronary arteries on patient 23). None of the cases reported association with connective tissue disorders, systemic inflammatory diseases, hormonal therapy, or the peripartum period.
A positive family history of coronary aneurysms was registered for patients 13, 14, 15, and 16. No family history of other aneurysmatic or dissecting complications was reported.
Six patients (46.1%) were asymptomatic. However, four cases (30.8%) presented with myocardial infarction and three (23.1%) with angina. In 13 cases (81.3%), coronary aneurysms were diagnosed by coronary angiography. Three cases were diagnosed by other methods: one (6.3%) during autopsy, one (6.3%) with computer tomography coronary angiography, and one (6.3%) with transthoracic echocardiography.
In six cases (40%), multiple coronary arteries were aneurysmatic, with three-vessel aneurysms in three patients (20%). Overall, the right coronary was the most affected vessel (n=7), followed by the left anterior descending (n=6), and the circumflex artery (n=6).
Local treatment was reported in a single patient (patient 11): a coronary bypass surgery that, due to operative complications, lead to patient death. Two other patients died, one due to sepsis (patient 18) and another due to rupture of the coronary aneurysm (patient 21). Regarding the remaining patients, only two had outcomes reported and both remained asymptomatic at follow-up (patients 22 and 23).
Discussion
In this study, we report and systematically analyze the previous reports of coronary dissection and aneurysm in ADPKD patients.
Cardiovascular disease is the main cause of death among ADPKD patients, with half of the mortality cases being attributable to ischemic heart disease.Citation30 Ischemic heart disease is highly prevalent in ADPKD and is present even before ESRD.Citation31 However, coronary atherosclerosis may not be the sole source of cardiac associated-morbidity and mortality in ADPKD. As the present study shows, coronary artery dissections and aneurysms also represent a cause of angina, myocardial infarction, and death in ADPKD patients.
Polycystin-1 and -2, the two mutated proteins responsible for ADPKD,Citation2 are expressed in smooth muscle cells and myofibroblasts of the tunica media and in the endothelial layer of vessels.Citation32 It has been proposed that mutation of either of these proteins could contribute to vascular wall weakness.Citation32 An autopsy analysis revealed focal media defects on extracranial arteries that could represent precursor lesions of aneurysms.Citation24 Thus, mutation of ADPKD-related genes could be responsible for an arteriopathy that predisposes to aneurysm formation or vessel wall dissection.
Concerning the clinical case reported here we must acknowledge that, especially without access to images from the first coronary angiography, it is difficult to classify the right coronary artery dissection culpable for the second coronary syndrome as spontaneous or secondary to endovascular manipulation. Spontaneous coronary artery dissections are rare events. However, in this case balloon angioplasty was only performed on the circumflex artery and the rates of dissection solely due to guide-wire insertion are also low. Even if the dissection was triggered by the angiographic manipulation, we cannot ascertain whether the patient already had vessel weakness – either due to atherosclerosis or due to an arteriopathy caused by mutation of ADPKD genes.
With regards to coronary artery dissection, the findings of the present study are in line with previous reports for non-ADPKD patients, such as female predominance, age of presentation before 50 years old and left anterior descending as the most affected artery.Citation33 Coronary atherosclerosis and use of hormonal therapyCitation33 were the only potentially predisposing factors of coronary artery dissection denoted here. Despite previous reports of familial association of aortic dissections on ADPKD individuals,Citation34 we did not observe the same for coronary dissections.
In the majority of the cases described, including the clinical case reported, percutaneous intervention with stent placement was the therapy of choice and provided good symptomatic relief. Nevertheless, half of patients maintained a dissected vessel on follow-up. The overall success rate described for percutaneous intervention in dissection is poorCitation33 and spontaneous resolution has also been described after dissection.Citation35
As far as coronary aneurysms in ADPKD patients are concerned, a controlled case series has reported a higher prevalence than in the general population undergoing coronary angiography.Citation16 In accordance to previous reports,Citation36,Citation37 we registered male predominance, frequent concomitant presence of atherosclerosis and arterial hypertension and right coronary artery predominance. However, the median age at diagnosis was lower than expected – we observed a median age of diagnosis of 44 years and previous reports on general population note that only 16% of patients are diagnosed before reaching 50 years old.Citation38 Multiple coronary artery involvement was also more frequent than reported for non-ADPKD patients,Citation36,Citation37 and high rates of personal and family history of aneurysmatic burden on other extracranial vessels were registered.
Only one ADPKD patient with coronary aneurysm underwent coronary bypass surgery. The largest therapeutic experience with coronary aneurysms is still surgicalCitation36 but recent, minimally-invasive, percutaneous treatments to exclude the aneurysm appear to lead to reduced complication rates.Citation39
While the clinical characteristics of coronary dissection in ADPKD patients appear to mimic the ones for non-ADPKD individuals, we believe that the younger age at diagnosis, the aneurysmatic involvement of other vessels, the high family burden and the more frequent involvement of multiple arteries suggest a different mechanism of aneurysm formation as compared to the population without ADPKD diagnosis.
The clinical course of coronary aneurysms can be complicated by thrombosis, thromboembolism, formation of arteriovenous fistulae, vasospasm, and rupture.Citation36 We registered a high rate of myocardial infarction-associated diagnosis, and a complicated aneurysm and an operative complication as causes of death of two of the reported patients. Further studies are needed to confirm if coronary artery aneurysms confer worse outcomes to ADPKD patients and if asymptomatic diagnosis is worthwhile to prevent deleterious events.
Finally, the reported proportions of patients with arterial hypertension and coronary atherosclerosis in this systematic review are lower (<50%) than their incidence in non-ESRD ADPKD patients.Citation40,Citation41 This indicates that these may not have been predisposing factors for coronary abnormalities and that other sources of vessel weakness may be at play.
Study limitations
The limitations of the present analysis are the lack of access to all published cases, the small number of patients, the short-follow up and the incomplete outcome reporting of most studies. However, its systematic nature allows for conclusions of greatly enhanced quality.
Conclusions
Mutation of ADPKD-related genes could lead to an arteriopathy that predisposes to coronary artery abnormalities. Atherosclerosis may not be the sole source of cardiac associated-morbidity and mortality in ADPKD since dissections and aneurysms also represent a cause of angina, myocardial infarction, and death in ADPKD patients. This study highlights the need for more extensive analysis to evaluate the prevalence, risk factors and adequate intervention in these individuals – analysis of data from patients included in the CRISP cohortCitation42 and HALT-PKD trialsCitation43 may help further elucidate on these matters.
Disclosure statement
The author has completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. The authors have declared that no conflict of interest exists.
References
- Torres VE, Harris PC, Pirson Y. Autosomal dominant polycystic kidney disease. Lancet. 2007;369:1287–1301.
- Happe H, Peters DJ. Translational research in ADPKD: Lessons from animal models. Nat Rev Nephrol. 2014;10:587–601.
- Pirson Y. Extrarenal manifestations of autosomal dominant polycystic kidney disease. Adv Chronic Kidney Dis. 2010;17:173–180.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement. Epidemiology. 2007;18:800–804.
- Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. The CARE guidelines: Consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67:46–51.
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA. 2000;283:2008–2012.
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. An Intern Med. 2009;151:W-65–W-94.
- Pei Y, Obaji J, Dupuis A, et al. Unified criteria for ultrasonographic diagnosis of ADPKD. J Am Soc Nephrol. 2009;20:205–212.
- Saw J. Coronary angiogram classification of spontaneous coronary artery dissection. Catheter Cardiovasc Intervent. 2014;84:1115–1122.
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation. 1983;67:134–138.
- BMJ Clinical Evidence – MEDLINE cohort, case-control, case series and case study filter. URL: http://clinicalevidence.bmj.com. Available at: http://clinicalevidence.bmj.com/x/set/static/ebm/Learn/665076.html. Accessed December 1, 2014.
- Higgins J, Deeks J. Chapter 7: Selecting studies and collecting data. In: Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (Updated March 2011). The Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org
- Christ M, Bechtel U, Schnaack S, Theisen K, Wehling M. Aneurysms of coronary arteries in a patient with adult polycystic kidney disease: Arteriosclerosis or involvement by the primary disease? Clin Investig. 1993;71:150–152.
- Adubofour K, Sidaway L, Glatter T. Coronary artery aneurysms in association with adult polycystic kidney disease. Am Heart J. 1994;127:1411–1413.
- Bobrie G, Brunet-Bourgin F, Alamowitch S, et al. Spontaneous artery dissection: is it part of the spectrum of autosomal dominant polycystic kidney disease? Nephrol Dial Transplant. 1998;13:2138–2141.
- Hadimeri H, Lamm C, Nyberg G. Coronary aneurysms in patients with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1998;9:837–841.
- Magadle R, Weiner P, Rabner M, Mizrahi-Reuveni M, Davidovich A. Polycystic kidney disease as a new risk factor for coronary events. Isr Med Assoc J. 2002;4:21–23.
- Basile C, Lucarelli K, Langialonga T. Spontaneous coronary artery dissection: One more extrarenal manifestation of autosomal dominant polycystic kidney disease? J Nephrol. 2009;22:414–416.
- Itty CT, Farshid A, Talaulikar G. Spontaneous coronary artery dissection in a woman with polycystic kidney disease. Am J Kidney Dis. 2009;53:518–521.
- Kucukdurmaz Z, Buyukhatipoglu H, Sezen Y, Kaya Z. Polycystic kidney disease with coronary aneurysm and acute coronary syndrome. Intern Med. 2009;48:1989–1991.
- Lee CC, Fang CY, Huang CC, Ng SH, Yip HK, Ko SF. Computed tomography angiographic demonstration of an unexpected left main coronary artery dissection in a patient with polycystic kidney disease. J Thorac Imaging. 2011;26:W4–W6.
- Pourafkari L, Ghaffari S, Zamani B, Tolui M. Coronary artery ectasia in a patient with polycystic kidney disease. J Cardiovasc Thoracic Res. 2011;3:101–102.
- Klingenberg-Salachova F, Limburg S, Boereboom F. Spontaneous coronary artery dissection in polycystic kidney disease. Clin Kidney J. 2012;5:44–46.
- Ohara K, Kimura T, Karasawa T, et al. A large coronary aneurysm and its probable precursor lesions in a patient with autosomal dominant polycystic kidney disease: An implication for the process of aneurysmogenesis. Pathol Int. 2012;62:758–762.
- Velásquez AS, Gama GT, Costa JR, Jr, Abizaid A, Feres FU. Aneurismas das artérias coronárias: uma rara manifestação da doença renal policística autossômica dominante. Rev Bras Cardiol Invasiva. 2010;18:476–478.
- Afari ME, Quddus A, Bhattarai M, John AR, Broderick RJ. Spontaneous coronary dissection in polycystic kidney disease. Rhode Island Med J (2013). 2013;96:44–45.
- Degrauwe S, Qanadli SD, Eeckhout E. Multi-level vascular aneurysms and polycystic kidney disease. Int J Cardiol. 2013;170:441–442.
- Kang YR, Ahn J-H, Kim KH, Choi YM, Choi J, Park JR. Multiple cardiovascular manifestations in a patient with autosomal dominant polycystic kidney disease. J Cardiovasc Ultrasound. 2014;22:144–147.
- Ruderman I, Menahem S. Generalized aneurysmal disease in association with autosomal dominant polycystic disease. Clin Kidney J. 2014;7:416–417.
- Rahman E, Niaz FA, Al-Suwaida A, et al. Analysis of causes of mortality in patients with autosomal dominant polycystic kidney disease: A single center study. Saudi J Kidney Dis Transplant. 2009;20:806–810.
- Fick GM, Johnson AM, Hammond WS, Gabow PA. Causes of death in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 1995;5:2048–2056.
- Rossetti S, Harris PC. The genetics of vascular complications in autosomal dominant polycystic kidney disease (ADPKD). Curr Hypertens Rev. 2013;9:37–43.
- Saw J. Spontaneous coronary artery dissection. Can J Cardiol. 2013;29:1027–1033.
- Biagini A, Maffei S, Baroni M, et al. Familiar clustering of aortic dissection in polycystic kidney disease. Am J Cardiol. 1993;72:741–742.
- Mathur M, Huda N, Cohen H, Parris T. Spontaneous right coronary artery dissection: A case of spontaneous resolution. JACC Cardiovasc Intervent. 2014;7:e9–e10.
- Cohen P, O'Gara PT. Coronary artery aneurysms: A review of the natural history, pathophysiology, and management. Cardiol Rev. 2008;16:301–304.
- Manginas A, Cokkinos DV. Coronary artery ectasias: imaging, functional assessment and clinical implications. Eur Heart J. 2006;27:1026–1031.
- Baman TS, Cole JH, Devireddy CM, Sperling LS. Risk factors and outcomes in patients with coronary artery aneurysms. Am J Cardiol. 2004;93:1549–1551.
- Wood FO, Trivax JE, Safian RD. Coronary artery aneurysms: Case report and review of transcatheter management strategies. Catheterization Cardiovasc Intervent. 2013;82:E469–E476.
- Ecder T, Schrier RW. Hypertension in autosomal-dominant polycystic kidney disease: Early occurrence and unique aspects. J Am Soc Nephrol. 2001;12:194–200.
- Kocaman O, Oflaz H, Yekeler E, et al. Endothelial dysfunction and increased carotid intima-media thickness in patients with autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2004;43:854–860.
- Grantham JJ, Torres VE, Chapman AB, et al. Volume progression in polycystic kidney disease. N Engl J Med. 2006;354:2122–2130.
- Torres VE, Chapman AB, Perrone RD, et al. Analysis of baseline parameters in the HALT polycystic kidney disease trials. Kidney Int. 2012;81:577–585.