Abstract
Objective: Cisplatin is a potent antineoplastic agent used and its major limiting side effect is nephrotoxicity. The aims of the study are early detection of acute kidney injury (AKI) with biomarkers and investigation of the potential nephron-protective effects of theophylline. Methods: Glomerular filtration rates (GFR), neutrophil gelatinase-associated lipocalin (NGAL), cystatin C were measured at 5th day of treatment in all of the patients. In addition, these parameters were measured repeatedly after the administration of cisplatin, at 2nd hour, 5th and 20th days. Patients: Sixty patients who are planned to receive cisplatin for the first time were included in the study. Patients were divided into two groups as Group 1 (n = 30) (standard treatment arm) and Group II (n = 30) (theophylline arm). Results: In both groups after the administration of cisplatin, GFR showed a significant decrease within time (p = 0.006). Urine NGAL levels were significantly high after 2 h of cisplatin administration (p < 0.001), no significant difference was observed between groups. However, when the time*group effects were considered together, higher NGAL levels were detected in the group not receiving theophylline (p = 0.025). After 5 days of cisplatin administration, urine protein levels were significantly higher in both groups (p < 0.001). Conclusion: Results showed that urine NGAL level is a superior biomarker compared to serum creatinine and serum cystatin C in the detection of early AKI. Theophylline was found not to bring a complete protection for the kidneys, but less nephrotoxicity was developed when compared to the group not receiving theophylline.
Introduction
Cisplatin is an antineoplastic agent used for the treatment of many solid organ cancers. It is an effective chemotherapeutic agent. However, nausea-vomiting, nephrotoxicity, neurotoxicity, ototoxicity and more rarely ocular toxicity can be observed.Citation1 The main dose limiting side effect of cisplatin is nephrotoxicity.Citation2 Cisplatin-related nephrotoxicity is dose-dependent and this is the most important limiting factor that restricts the dose increase and the efficiency of the medication, as well.Citation3 Cisplatin causes cell damage and cell death by activating many signal pathways in renal tubular cells. It forms a strong inflammatory response that further increases the tissue damage. Meanwhile, it leads to ischemic damage to the kidney by causing damage in the vascular structures of the kidney and contributes to the decrease in the glomerular filtration rate (GFR).Citation1
Acute kidney injury (AKI) is a well-known cause of high morbidity and mortality for all patient groups despite improved medical care.Citation4 The decrease in GFR begins earlier than the increase in serum creatinine and a decrease of roughly 50% occurs in the kidney functions when a rise is detected in the serum creatinine levels, which is the most commonly used marker in the diagnosis of renal failure.Citation5 In addition, creatinine production changes depending on the body muscle mass and dietary factors. All these factors could explain why serum creatinine is not a good biomarker to estimate the GFR correctly.Citation6 Therefore, the need for new biomarkers has increased in recent years.Citation7 In this sense, cystatin C and neutrophil gelatinase-associated lipocalin (NGAL) are two of early promising biomarkers.
Afferent arteriolar tonus and glomerular perfusion are adjusted with the negative feedback mechanism in order to limit the energy usage of the kidney (tubuloglomerular feedback) and determined by the fluid-solute inside the tubule.Citation8 It was shown that theophylline, which is a competitive antagonist of adenosine, improved kidney function at the development stage of cisplatin-dependent AKI.Citation9
In this study, we aimed to determine AKI at an early stage by assessing the serum cystatin C and urine NGAL levels in patients in whom cisplatin was administered for the first time and to research the probable effect of theophylline in protecting the kidney.
Materials and methods
Patients
Patients who applied to the Medical Oncology Department of Erciyes University Faculty of Medicine between 2011 and 2014 and for whom cisplatin-based chemotherapy was planned due to various malignancies were included in this prospective study. Approved by the Ethics Committee of Erciyes University, the study was conducted in compliance with ethic rules and with the consent of the patients. The ages, genders, malignancies, previous chemotherapy, cisplatin and theophylline usage histories of the patients were investigated. Their heights and weights were measured and body surface areas were calculated. People who were below the age of 18 years, had hypertension, fever > 38 °C, active infection, calculation of GFR < 60 mL/min before cisplatin administration, previous history of cisplatin-based chemotherapy application, history of pelvic radiotherapy and history of theophylline usage were not included in the study.
Chemotherapy protocol
For the patients, 21-day chemotherapy regimens consisting of 50 mg/m2 cisplatin were planned together with hydration, mannitol and diuretic treatment.
Study plan
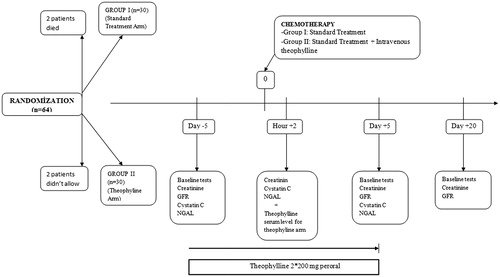
An aprepitant (Emend®, NJ, USA) oral capsule and dexamethasone (Dekort®, Istanbul, Turkey) 16 mg were given intravenously to the patients of both groups before taking cisplatin in order to prevent cisplatin-dependent nausea and vomiting (). Aprepitant treatment was continued as three doses in total for 48 h following cisplatin administration. Metoclopramide (Metpamid®, Istanbul, Turkey) tablet treatment was applied to the patients who had persisting complaint of nausea during the follow-ups. Volume loss based on vomiting was prevented and attention was paid to the steadiness of the hemodynamics. Before cisplatin administration, 20 mEq KCl and 2 g MgSO4 were given to the patients in group 1 together with 1000 mL 0.9% NaCl. After cisplatin, 150 mL 20% mannitol and 10 mEq furosemide were administered together with 1000 mL 0.9% NaCl. Similarly, before the cisplatin administration, 20 mEq KCl and 2 g MgSO4 were given to the patients in group II together with 1000 mL 0.9% NaCl. In addition, in group II, 100 mg intravenous infusion of theophylline was initiated 30 min before cisplatin administration which was given concurrently with theophylline. Similarly, after cisplatin administration, 150 mL 20% mannitol and 10 mEq furosemide were given together with 1000 mL 0.9% NaCl.
The cisplatin infusion period was kept stable as 2 h in both groups. Intravenous fluid infusions began 2 h before cisplatin administration and were given intravenously covering the period after the 2nd hour.
Blood and urine samples
The venous blood and urine samples of the patients in both groups were taken on the 5th day (−5th) before cisplatin administration, 2 h after cisplatin was given and on the +5th day and +20th day (before the second cure). Serum creatinine, Na, K, Mg and cystatin C, Anna, Mg, microprotein and creatinine in urine were measured. Biochemical analyzes were performed with the spectrophotometric method by using appropriate kits in Cobas 8000 701/702 (Roche®, Indianapolis, USA) autoanalyzers. The serum theophylline level was measured at the 2nd hour after cisplatin administration in group II. Theophylline level was researched with the enzymatic method by using appropriate kits in Indiko plus branded autoanalyzers.
Fractionated sodium excretion (FENa), fractionated magnesium excretion (FEMg) and proteinuria were calculated with the results obtained. Meanwhile, creatinine was measured in the 24-h urine, which was taken on the −5th, +5th and +20th days of cisplatin administration, and creatinine clearance and the GFR were calculated. NGAL was measured in the spot urine which was obtained from the patients of both groups on the −5th day, 2nd hour and +5th day of cisplatin administration. Urine NGAL was measured by using Lipocalin-2/NGAL ELISA kits with the catalog number 201-12-1720 (Sunredbio Products, Shanghai, China).
Statistical analyses
The data in this study were analyzed using IBM SPSS 22 software (Chicago, IL). The mean, SD, median and minimum–maximum values of the data were given as the descriptive statistics in the study. Shapiro–Wilks test statistics were used while examining the distribution of the variables in the data set. Significance level was considered as p < 0.05. Independent Sample t-test was used for comparing the test statistics of two independent groups during the comparisons of variables that complied with normal distribution. For the analysis of the data that were not distributed normally, the Mann–Whitney U test statistics were used. Pearson correlation analysis was conducted to statistically examine the relations of the variables with each other. The exact test method of the chi-squared test statistics was used for presenting the comparison results of the demographic data. The General Linear Mixed Effect models (GLM) were used during the interpretation of the intragroup and intergroup comparisons of the repeated data in the study. Data were interpreted by presenting the group effect, time effect and group*time effect. In case of a significant difference in intragroup and intergroup comparisons post hoc test statistics was used to observe which group had a change and when it occurred. The results were evaluated by implementing the Bonferonni correction method.
Results
Sixty-four patients were included in the study. During the study, two patients died and two patients left the study willingly. A total of 60 patients—18 female and 42 male—participated in the study the ages of which were between 30 and 78 years. There were no significant differences between the groups in terms of gender, age, weight and body surface area (BSA). Patient characteristics are shown in . Patients were randomized in two treatment arms as group I (n = 30) (standard treatment arm) and group II (n = 30) (theophylline arm).
Table 1. Comparison of demographical and laboratory features between the Group 1 and the Group 2.
Serum creatinine
In , the comparisons of the medication days of groups I and II are given according to the examined variables. Group effect, time effect and group*time effect were researched in the comparison. It was found that the average change in creatinine variable was not significantly different between the groups (p = 0.965). When the average change in creatinine is examined in respect of time, the change is found to be significant (p = 0.011). When the group*time effects are examined together, it is seen that the change in creatinine is not significant (p = 0.189). While the values on the +20th, +5th and −5th days are the same in both groups, a statistically significant decrease is observed between the −5th day and 2nd hour in terms of creatinine means.
Table 2. Comparison of the medication days in terms of GFR, NGAL and cystatin C variables between Group I and Group II.
Glomerular filtration rate
As it is shown in , the change in the GFR variable was not statistically different between the groups (p = 0.149). When the change in the GFR is examined in terms of time, it is seen that the average change is significant and there is a decrease in the GFR in both groups over time (p = 0.006). When the group*time effects are examined together, it is seen that the change in the GFR is not significant (p = 0.676). Whereas a significant decrease is observed in group I between the −5th and +5th days in respect of the GFR variable, it was discovered that the means of the +20th, −5th and +5th days were not different.
Neutrophil gelatinase-associated lipocalin
It is inferred from that no statistically significant difference exists between the groups according to the NGAL variable (p = 0.721). When examined in terms of time, the average change of the NGAL variable in both groups is found to be statistically significant and it increases in the NGAL (p < 0.001). It is seen that the NGAL average values of the NGAL variable’s −5th day, +5th day and 2nd hour values are different from each other in group I. While the average values of the −5th and +5th days present similarities in group II, the means of the 2nd hour, −5th day and +5th day show a difference. A significant increase is seen in the NGAL values at the 2nd hour in both groups. While this increase itself does not present statistical difference when assessed between groups, it is seen that the change is statistically significant according to the group*time effect (p = 0.025). Urinary NGAL levels were found to be increased significantly in both groups, and the rate of increase was higher in group I, when compared with the group II in the +2nd hour.
Cystatin C
No difference exists between the groups in terms of the cystatin C variable, as it is shown in (p = 0.077). The averaged change in the cystatin C variable is found to be significant (p < 0.001). It is seen that the change is not significant in respect of the group*time effect (p = 0.174). It is seen that the average values of the cystatin C variable are different from each other in group I on the −5th and +5th days and at the 2nd hour. While the average change seen on the −5th and +5th days presents similarities in group II, difference is observed in the means of the 2nd hour, −5th day and +5th day. Cystatin C presents a statistically significant and similar decrease in the 2nd hour in both groups.
Fractionated sodium excretion and fractionated magnesium excretion
Neither differences between the two groups nor significant changes within the two treatment arms regarding pre- and post-chemotherapy measurements in terms of serum FENa or FEMg values were observed.
Proteinuria
It is inferred from that difference exists between the groups in respect of the urinary microprotein/creatinine ratios (p = 0.019). Similarly, when examined in terms of time, the average change in the microprotein/creatinine ratios were found to be significant (p < 0.001). It is seen that the change is not significant in respect of the group*time effect (p = 0.153). While the average values of microprotein/creatinine are similar on the −5th and +20th days in group I, the average values on the +5th, +20th and −5th days are different from each other. Similarly, while the average change shows a similarity on the −5th and +20th days in group II, the means of the +5th, −5th and +20th days present different attributes from each other. A statistically significant increase was observed in the proteinuria amount in both groups on the +5th day. It is seen that proteinuria statistically increased more in group I compared to group II on the +5th day.
Table 3. Comparison of the medication days in terms of FENa, FEMg, proteinuria in Group I and Group II.
Serum theophylline level
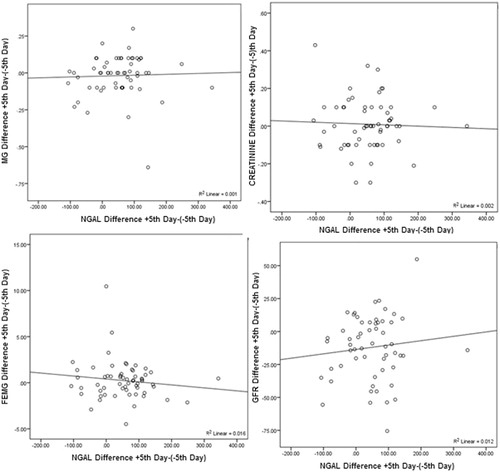
It was noticed that the serum theophylline levels of the patients in group II were within the therapeutic interval (5–15 mg/L) after 2 h following cisplatin administration. In and , the correlation comparison results of the delta variables are given in respect of the NGAL variables. While there is no statistically significant relationship between the creatinine ΔT3–T1 and the NGAL variable (p = 0.759), a negative-directional weak relationship is mentioned (r= −0.040). While there is no statistically significant relationship between the Mg ΔT3–T1 and the NGAL variable (p = 0.731), a positive-directional weak relationship is noted (r= −0.035). It was observed that the other variables do not have a significant relationship with the NGAL variables.
Table 4. Correlation comparison results of the delta variables according to NGAL levels.
Discussion
In our study, urine NGAL levels were found to be significantly increased in both groups within the +2nd hour of cisplatin administration. No statistically significant difference was observed between the groups. According to the group*time effect, the increase in urine NGAL levels were significantly higher in the group without theophylline intake when compared to the group with theophylline intake in the +2nd hour after cisplatin administration. However, the decrease in the GFR was similar in both groups.
It is well known that, serum cystatin C levels are not affected by gender, age, race, protein intake and muscle mass like serum creatinine.Citation10 Although the cellular mechanisms underlying cisplatin nephrotoxicity is still not exactly known, it is in vivo mechanism is quite complicated.Citation1 In recent years, emphasis has mostly been laid on the role of oxidative stress in its pathophysiology. Oxidative stress is characterized by an increase in reactive oxygen species formation and/or insufficiency of the antioxidant system.Citation11
AKI is a complex syndrome which ranges from a slight increase in serum creatinine level to anuria and need for renal replacement treatments and may manifest with various clinical manifestations.Citation7 The findings of AKI develop gradually and generally occur 3–5 days after cisplatin administration.Citation2 In this study, therefore, kidney functions were assessed 5 days after cisplatin administration and also after 20 days (before the subsequent treatment) in order to determine the long-term effect of the single-dose cisplatin.
It has been suggested that, proteinuria could be observed especially due to the effect of the cisplatin on the proximal tubule in cisplatin-administered mice.Citation12 In a study conducted on 30 patients, in whom three cures of high-dose cisplatin treatment were administered (40 mg/m2/day during 5 days), proteinuria, albuminuria and aminoaciduria were observed in each treatment cure.Citation13 Likewise, proteinuria was significantly observed in both groups on the +5th day after cisplatin administration in our study as well. More proteinuria was observed in the group without theophylline intake. This result could be interpreted as theophylline was not able to prevent proteinuria completely, however, less proteinuria developed depending on the development of less nephrotoxicity.
NGAL is a protein which is a member of the lipocalin superfamily. Its expression increases in the renal tubular cells during the regenerative process after renal damage. Urine NGAL is a biomarker which can reflect the damage in glomerules, proximal and distal tubules in various renal diseases.Citation14 NGAL response against AKI is quite fast. NGAL can be detected in urine within 2 h following the renal artery occlusion in studies conducted on mice.Citation15,Citation16 NGAL has been shown as an early biomarker of AKI initially in experimental studies and then in clinical studies.Citation5,Citation17,Citation18 In addition, Yang et al.Citation19 defined urine NGAL as an independent marker of in-hospital mortality and permanent loss of renal function in their study.
It has been shown in a study conducted in 196 children, to whom cardiopulmonary by-pass was performed, that urine NGAL level increased 15 times in the postoperative 2nd hour and 25 times in the 4th and 6th hours and that it had high sensitivity specify.Citation20 Meanwhile, it precisely estimated the renal replacement treatment need, hospitalization duration and mortality. It was reported in one study that once measured urine NGAL had 90% sensitivity and 99% specify in the diagnosis of AKI.Citation21 It was observed in another study that urine NGAL increased 2 days earlier than the ones with a 50% increase in the serum creatinine levels and >6 times, and urine NGAL levels were correlated with the severity of AKI.Citation22 Similar to these studies, urine NGAL presented a statistically significant increase within the +2nd hour of cisplatin administration in both groups in our study.
Several studies showed that cystatin C, which is another early biomarker in AKI was much more sensitive and specific than serum creatinine in GFR determination.Citation10,Citation23 However, cystatin C presented a statistically significant decrease in both groups within the +2nd hour of cisplatin administration in our study. While the increase in urine NGAL within the +2nd hour of cisplatin administration supports the decrease in GFR, the decrease in cystatin C and serum creatinine levels instead of a similar increase leads to the conclusion that they are not good biomarkers for the determination of AKI.
In clinical practice, protection is provided against cisplatin nephrotoxicity firstly by decreasing excessive cisplatin exposure through hydration/diuresis, monitoring creatinine clearance closely and decreasing the cisplatin dose when renal function starts to be disrupted.Citation24,Citation25 However, it was shown that traditional methods such as hydration and osmotic diuresis are insufficient to decrease nephrotoxicity substantially in patients whom single-cure cisplatin-based chemotherapy is applied.Citation26
The first method to prevent cisplatin nephrotoxicity is to use mannitol and diuresis. However, no full agreement has been reached about the efficiency of mannitol. It was presented in a study conducted on renal damage with saline, saline + furosemide and saline + mannitol intake that both saline and saline + furosemide administration had a protective effect against cisplatin nephrotoxicity. Moreover, it was also specified that mannitol could contribute to the cisplatin nephrotoxicity.Citation27 Similarly, it was also stated that high-dose furosemide administration might increase cisplatin nephrotoxicity.Citation28 It was observed that only hydration and osmotic diuresis were not adequate to prevent a decrease in GFR in patients who had single-cure cisplatin based chemotherapy.Citation26
In one study, the GFRs of patients, in whom intravenous theophylline was applied 45 min before giving the contrast agent, were calculated with inulin clearance and paraaminohippuric acid clearance. Thus, it was shown that adenosine played a major role in contrast agent nephropathy and theophylline prevented a decrease in renal function.Citation29 Afterward, the nephroprotective effect of theophylline in contrast agent nephropathy was also confirmed with several clinical studies.Citation30–32
Adenosine is an adenine nucleoside that is formed as a result of ATP hydrolysis. It leads to adenosine vasodilatation in the heart and many vascular beds. In the kidneys, adenosine leads to vasoconstriction in afferent arterioles and therefore to a decrease in GFR and renal blood flow.Citation33 It is a molecule related to the renal hemodynamic changeCitation34 caused by cisplatin, which plays a role in the tubule functions and hormone release in addition to the regulation of the hemodynamics in the kidney.Citation35 It was shown in many experimental studies that tissue adenosine concentrations increased after renal damage following ischemia or resulting from medication.Citation36 The protective effect of theophylline, which is an adenosine antagonist, on cisplatin nephrotoxicity was first presented in studies conducted on rats.Citation34 The study conducted by Benoehr et al.Citation26 was the first to show the kidney-protective effect of theophylline in humans who receive cisplatin-based chemotherapy.
In recent years, studies have been conducted which suggest that theophylline usage does not have any kidney-protective effect. It was presented in a prospectively randomized double-blind and placebo controlled study, which was conducted by Mousavi et al.Citation37 that aminophylline and theophylline did not have any protective effect against cisplatin nephrotoxicity in 76 patients. However, kidney functions were evaluated by considering only the creatinine levels 1 day before and 5 days after the cisplatin administration in that study.
In our study, GFR similarly decreased in both groups with the effect of cisplatin. Serum creatinine and cystatin C levels did not reflect this decrease in the GFR. Urine NGAL level increased in both groups 2 h after cisplatin administration and a higher increase was observed in the group without theophylline intake. Similarly, the protein level in the urine was higher in the group without theophylline intake 5 days after cisplatin administration. Although it was supposed that cisplatin had a less nephrotoxic effect in the group with theophylline intake, theophylline does not protect the kidneys completely.
Preventing cisplatin-dependent kidney injury is critically important. Thus, the morbidity and mortality related to AKI may decrease, hospitalization duration may be reduced and treatment costs may be decreased. Meanwhile, routine usage of an agent that protects the kidneys against cisplatin will allow for the use of cisplatin, which is an effective drug, in repeated cures without any decrease in doses and in higher doses.
Funding information
This study was funded by Erciyes University Scientific Research Council with the project number TTU-2014-5103.
Disclosure statement
On behalf of all authors, the corresponding author states that there is no conflict of interest. This article does not contain any studies with animals performed by any of the authors.
ORCID
Cevat Yazici http://orcid.org/0000-0003-0625-9542
References
- Pabla N, Dong Z. Cisplatin nephrotoxicity: Mechanisms and renoprotective strategies. Kidney Int. 2008;73:994–1007.
- Arany I, Safirstein RL. Cisplatin nephrotoxicity. Semin Nephrol. 2003;23:460–464.
- Hanigan MH, Devarajan P. Cisplatin nephrotoxicity: Molecular mechanisms. Cancer Ther. 2003;1:47–61.
- Lameire N, Van BW, Vanholder R. Acute renal failure. Lancet. 2005;365:417–430.
- Mishra J, Ma Q, Prada A, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534–2543.
- Kim KE, Onesti G, Ramirez O, Brest AN, Swartz C. Creatinine clearance in renal disease. A reappraisal. Br Med J. 1969;4:11–14.
- Malyszko J. Biomarkers of acute kidney injury in different clinical settings: A time to change the paradigm? Kidney Blood Press Res. 2010;33:368–382.
- Osswald H, Muhlbauer B, Vallon V. Adenosine and tubuloglomerular feedback. Blood Purif. 1997;15:243–257.
- Osswald H. Renal effects of adenosine and their inhibition by theophylline in dogs. Naunyn Schmiedebergs Arch Pharmacol. 1975;288:79–86.
- Newman DJ, Thakkar H, Edwards RG, et al. Serum cystatin C measured by automated immunoassay: A more sensitive marker of changes in GFR than serum creatinine. Kidney Int. 1995;47:312–318.
- Liochev SI, Fridovich I. The role of O2.—in the production of HO.: In vitro and in vivo. Free Radic Biol Med. 1994;16:29–33.
- Safirstein R, Winston J, Goldstein M, Moel D, Dikman S, Guttenplan J. Cisplatin nephrotoxicity. Am J Kidney Dis. 1986;8:356–357.
- Daugaard G, Abildgaard U, Holstein-Rathlou NH, Bruunshuus I, Bucher D, Leyssac PP. Renal tubular function in patients treated with high-dose cisplatin. Clin Pharmacol Ther. 1988;44:164–172.
- Kuwabara T, Mori K, Mukoyama M, et al. Urinary neutrophil gelatinase associated lipocalin levels reflect damage to glomeruli, proximal tubules and distal nephrons. Kidney Int. 2009;75:285–294.
- Chiao H, Kohda Y, McLeroy P, Craiq L, Housini I, Star RA. Alpha-melanocyte-stimulating hormone protects against renal injury after ischemia in mice and rats. J Clin Invest. 1997;99:1165–1172.
- Rabb H, Ramirez G, Saba SR, et al. Renal ischemic-reperfusion injury in L-selectin-deficient mice. Am J Physiol. 1996;271:408–413.
- Mishra J, Mori K, Ma Q, Kelly C, Barasch J, Devarajan P. Neutrophil gelatinase-associated lipocalin: A novel early urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol. 2004;24:307–315.
- Mishra J, Dent C, Tarabishi R, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury after cardiac surgery. Lancet. 2005;365:1231–1238.
- Yang HN, Boo CS, Kim MG, Jo SK, Cho WY, Kim HK. Urine neutrophil gelatinase-associated lipocalin: An independent predictor of adverse outcomes in acute kidney injury. Am J Nephrol. 2010;31:501–509.
- Bennett M, Dent CL, Ma Q, et al. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: A prospective study. Clin J Am Soc Nephrol. 2008;3:665–673.
- Nicholas TL, O’Rourke MJ, Yang J, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosis acute kidney injury. Ann Intern Med. 2008;148:810–819.
- Zappitelli M, Washburn K, Arikan AA, et al. Urine neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in critically ill children: A prospective cohort study. Crit Care. 2007;11:R84.
- Kyhse-Anderson J, Schmidt C, Nordin G, et al. Serum cystatin C, determined by a rapid, automated particle-enhanced turbidimetric method, is a better marker than serum creatinine for gomerular filtration rate. Clin Chem. 1994;40:1921–1926.
- Launay-Vacher V, Rey JB, Isnard-Bagnis C, Deray G, Daouphars M. Prevention of cisplatin nephrotoxicity: State of the art and recommendations from the European Society of Clinical Pharmacy Special Interest Group on Cancer Care. Cancer Chemother Pharmacol. 2008;61:903–909.
- Losonczy G, Mathe C, Muller V, Szondy K, Moldvay J. Incidence, risk factors and prevention of cisplatin-induced nephrotoxicity in patients with lung cancer. Magy Onkol. 2010;54:289–296.
- Benoehr P, Krueth P, Bokemeyer C, Grenz A, Osswald H, Hartmann JT. Nephroprotection by theophylline in patients with cisplatin chemotherapy: A randomized, single-blinded, placebo controlled trial. J Am Soc Nephrol. 2005;16:452–458.
- Santoso JT, Lucci JA, 3rd, Coleman R, Schafer I, Hannigan EV. Saline, mannitol and furosemide hydration in acute cisplatin nephrotoxicity. Cancer Chemother Pharmacol. 2003;52:13–18.
- Lehane D, Winston A, Gray R, Daskal Y. The effect of diuretic pre-treatment on clinical, morphological and ultrastructural cis-platinum induced nephrotoxicity. Int J Radiat Oncol Biol Phys. 1979;5:1393–1399.
- Erley CM, Duda SH, Schlepckow S, et al. Adenosine antagonist theophylline prevents the reduction of glomerular filtration rate after contrast media application. Kidney Int. 1994;45:1425–1431.
- Huber W, Schipek C, Ilgmann K, et al. Effectiveness of theophylline prophylaxis of renal impairment after coronary angiography in patients with chronic renal insufficiency. Am J Cardiol. 2003;91:1157–1162.
- Katholi R, Taylor GJ, McCann WP, et al. Nephrotoxicity from contrast media: Attenuation with theophylline. Radiology. 1995;195:17–22.
- Kolonko A, Wiecek A, Kokot F. The nonselective adenosine antagonist theophylline does prevent renal dysfunction induced by radiographic contrast agents. J Nephrol. 1998;11:151–156.
- Modlinger PS, Welch WJ. Adenosine A1 receptor antagonists and the kidney. Curr Opin Nephrol Hypertens. 2003;12:497–502.
- Heidemann HT, Müller S, Mertins L, Stepan G, Hoffmann K, Ohnhaus EE. Effect of aminophylline on cisplatin nephrotoxicity in the rat. Br J Pharmacol. 1989;97:313–318.
- Osswald H, Mühlbauer B, Schenk F. Adenosine mediates tubuloglomerular feedback response: An element of metabolic control of kidney function. Kidney Int. 1991;3932:128–131.
- Arend LJ, Thompson CL, Brandt MA, Spielman WS. Elevation of intrarenal adenosine by maleic acid decreases GFR and renin release. Kidney Int. 1986;30:656–661.
- Mousavi SSB, Zadeh MH, Shahbazian H, et al. The protective effect of theophyline in cisplatin nephrotoxicity. Saudi J Kidney Dis Transpl. 2014;25:333–337.