Abstract
Collapsing focal segmental glomerulosclerosis (cFSGS) is characterized by rapid progression to end-stage renal disease (ESRD). We evaluated the clinicopathological spectrum of cFSGS and compared its clinical behavior to steroid and tacrolimus (TAC)-resistant noncollapsing focal segmental glomerulosclerosis (FSGS). All patients (>14 years) diagnosed with cFSGS were enrolled in the study. Staining for differentiated podocyte markers such as WT 1, PAX and KI67 were performed in all patients. The outcome and histological features of cFSGS was compared with a prospectively followed cohort of steroid and TAC-resistant noncollapsing FSGS. The study included 22 cFSGS patients and 19 cases of steroid and TAC-resistant FSGS. Complete remission, partial remission, steroid resistance, progression to ESRD and death were observed in 13.6%, 4.5%, 27.3%, 36.4% and 18.2% patients, respectively. Patients with cFSGS had higher serum creatinine and more advanced tubulointerstitial changes compared to resistant FSGS. Twenty-six percent of therapy resistant noncollapsing FSGS progressed to ESRD after two years of stopping TAC. However, there was no difference in progression to ESRD between cFSGS and therapy-resistant noncollapsing FSGS at the end of two years. Glomerular collapse in the setting of FSGS is poorly responsive to treatment and has a high rate of progression to ESRD. The long-term prognosis of cFSGS and steroid and TAC-resistant FSGS are similar.
Introduction
Collapsing focal segmental glomerulosclerosis (cFSGS) is a pathologic entity characterized by segmental or global glomerular capillary collapse, podocyte swelling and hyperplasia, tubulocystic changes and tubulointerstitial inflammation.Citation1 Patients with cFSGS typically present with heavy proteinuria and exhibit rapid progression to end-stage renal disease (ESRD).
Response to steroid therapy is probably one of the best predictor of long-term prognosis in focal segmental glomerulosclerosis (FSGS).Citation2 Long-term prognosis of steroid and calcineurin inhibitor (CNIs)-resistant FSGS is not known. Cases of FSGS with no response to steroids and calcineurin inhibitors are at increased risk of progression of renal disease. Rydel et al. analyzed 81 cases of FSGS and reported 100% patient survival at five and 10 in cases with remission compared to 66% and 41% in cases without any response.Citation2 The other factor-determining prognosis is the variant of FSGS. Among various variants collapsing variant has got the worst prognosis. Thomas et al. reported renal survival of 74% and 33% at one and three year, respectively, in cases of cFSGS.Citation3
In our previous analysis of FSGS,Citation4 cFSGS was encountered in 2% cases, less than that described in multiethnic or American-African cohorts.Citation3 We undertook this observational study to document the clinicopathological spectrum of cFSGS and compare the clinical behavior of his group with other FSGS histological variants that exhibited therapeutically adverse behavior, that is, steroid and tacrolimus (TAC)-resistant disease.
Materials and methods
Study participants
The prospective observational study was carried out at the Postgraduate Institute of Medical Education and Research, Chandigarh, India. All patients (age ≥ 14 years) with a diagnosis of cFSGS based on light microscopy, immunofluorescence and electron microscopy were enrolled in the study. Patients who received prior immunosuppressive therapy, cases positive for hepatitis B/C (HBV/HCV), cytomegalovirus (CMV) or human immunodeficiency virus I/II (HIV-I/II) and history of diabetes mellitus or any other systemic illness such as systemic lupus erythematous, cryoglobinemia and small/medium vessel vasculitis were excluded from the study. The Department review committee approved the study.
Investigations included urinalysis, serum creatinine, liver function tests, antinuclear antibody, antineutrophil cytoplasmic antibody, CMV PCR, HBsAg, anti-HCV and ELISA for HIV-I/II. Clinical presentation was classified into nephrotic syndrome and progressive renal failure. Patients were followed with urine analysis, serum creatinine and serum albumin on a monthly basis for the first three months and then quarterly till three years or till ESRD/death. All patients received maximal tolerable dose of ARBs. Dedifferentiation of podocytes was confirmed by documenting loss of differentiated podocyte marker molecule (WT-1), gain of immature podocyte marker (PAX 2) and proliferation marker (Ki 67).
For the purpose of comparison, we included a cohort of prospectively followed steroid and tacrolimus (TAC)-resistant noncollapsing FSGS. We also followed them prospectively every six months till a period of two years of initiating TAC therapy.
Definitions
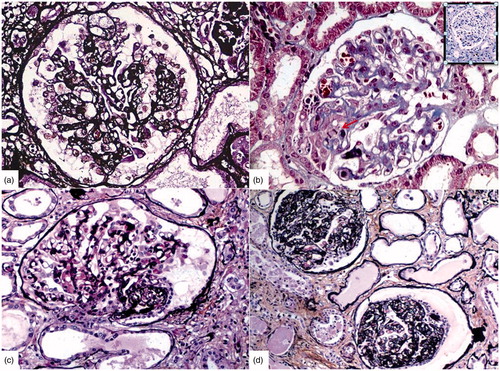
cFSGS: Segmental or global collapse of glomerular tuft with hypertrophy and hyperplasia of overlying podocytes (). Nephrotic syndrome: Proteinuria ≥3.5 g/d or ≥1.5 g/d along with serum albumin <2.5 g/dL, edema and hyperlipidemia.Citation5 Progressive renal failure: Deterioration of renal function over a period of weeks to <3 months. Relapse: reappearance of nephrotic range proteinuria after achieving remission. Steroid resistance: Persistence of nephrotic syndrome due to FSGS despite oral prednisolone (1 mg/kg/d) for 16 weeks. Complete remission (CR): reduction of proteinuria to <0.5 g/d and with creatinine clearance of >60 mL/min/1.73m2 and serum albumin >3.5 g/dL. Partial remission (PR): Reduction in proteinuria to 0.5–3.5 g/day and stable serum creatinine (change in serum creatinine <25%) or a decrease in proteinuria >50% from baseline and stable serum creatinine (change in serum creatinine <25%) with serum albumin >3.5 g/dL. TAC resistance: Inability to achieve CR/PR in spite of adequate dose (trough levels 5–10 ng/mL) and duration (24 weeks) of TAC therapy.
Figure 1. Photomicrographs of cFSGS show (a) global collapse of glomerular tuft wish hyperplasic and hypertrophied podocytes with overlying hypertrophied and hyperplastic podocytes (b) Hyperplastic podocytes (Ki 67 positive inset) over segmental collapsed tuft show mitosis, moderate cytoplasm with protein absorption droplets and prominent nucleoli (c) Segmental collapse with collagenized glomerular tuft having a crown of quiescent podocytes (d) Global collapse lined by row of cuboidal podocytes without mitosis and protein absorption droplets (PAS- Silver Methenamine stain a, c–d, Masson’s Trichrome-b, Immunohistochemistry Ki 67-insetd, a–c, X 40, d-X 20 original magnification).
Statistical analysis
Data are expressed as mean ± standard deviation and range for continuous variables and percentage for categorical variables. Student’s t-test and Mann–Whitney U-test was used to compare means for parametric and nonparametric data, respectively. Chi-square or Fisher's exact tests were used for the analysis of categorical variables. A two-tailed p values of < 0.05 was considered significant. Statistical analysis was performed using Graph Pad Prism -6.
Results
A total of 250 cases of FSGS were reported during the study period, including 22 (8.8%) with cFSGS () and 66 (26.4%) cases of steroid-resistant FSGS (44 received TAC and 19 non-cFSGS were resistant to therapy). There were 15 (68.1%) males and seven (31.9%) females with mean age of 26.9 ± 9.4 (range: 14–55) years. All the patients received oral prednisolone (1 mg/kg) for a period of 16 weeks before declaring resistance. Details of laboratory investigations and the clinical and pathological parameters are mentioned in .
Table 1. Comparison of clinical and pathological parameters of cFSGS and steroid and tacrolimus resistant FSGS.
cFSGS
The primary presentations were nephrotic syndrome and progressive renal failure in 11 (50%) each. CR, PR, SR nephrotic syndrome, ESRD and death were noted in 3 (13.6%), 1(4.5%), 6 (27.3%), 8 (36.4%) and 4 (18.2%), respectively. The clinical details are given in . Parvovirus B19 DNA was positive in eight (36.4%) cases. There was no difference in the clinical presentation (nephrotic syndrome or with renal dysfunction, p = 0.65), outcome (p = 0.60), the presence of TMA (p = 0.34) or Ki 67 staining (p = 1.00). Ki 67 () was positive in 68% of all the glomeruli with collapse. Loss of WT1 was restricted to collapse glomeruli. PAX2 was absent in normal glomeruli and was seen in only in the collapsed glomeruli. Among patients with cFSGS, there were no differences in the staining for WT1, Ki67 and PAX2 in cases with either nephrotic syndrome or progressive renal failure as the initial presentation.
Table 2. Brief summary of all the patients with cFSGS.
Nephrotic syndrome
Of the 11 study subjects, four (18.2%) patients had remission with steroids (3 CR and 1 PR). Of the three patients with CR; first case had infrequent relapses, all episodes were steroid responsive, second patient with CR became steroid dependent after initial response and was started on tacrolimus. The patient persists to remain in remission on low-dose prednisolone 0.1 mg/kg/day and tacrolimus and the third patient with CR had frequent relapses, which gradually progressed to steroid resistance. Initiation of tacrolimus for steroid-resistant state led to remission but had to be withdrawn following decline in GFR after four months. He continues to have nephrotic range proteinuria. One patient who achieved PR remains in remission after 30 months. Of the remaining seven (63.6%) patients, two (28.6%) expired within two months of starting therapy due to severe sepsis and five (71.4%) patients with steroid-resistant nephrotic syndrome; one (9.1%) responded to rituximab, three (27.3%) had progressive CKD and one developed ESRD (9.1%). Three patients showed progressive reduction in GFR, with one progressing to ESRD.
Progressive renal failure
Of the 11 patients with progressive renal failure, one (9.1%) showed improvement in serum creatinine with steroid therapy but continued to have nephrotic range proteinuria. Two (18.2%) developed sepsis and expired within two months of diagnosis. The remaining eight (72.7%) progressed to ESRD.
Patients of cFSGS with nephrotic syndrome had higher protein (p-0.37), serum creatinine (p < 0.0001) and lower serum albumin (p-0.04) compared to cases with cFSGS with progressive renal failure. Two (25%) underwent live related kidney transplantation and six (75%) are on dialysis. Of the two patients who underwent transplantation, one lost her graft after 12 months to plasma cell-rich rejection. She underwent a successful second deceased donor transplant and maintains normal graft function after 12 months. The second patient has normal graft function eight months after transplantation. Patients with renal failure showed tubulocystic dilation (p-0.08) and TMA (p-0.02) more frequently compared to cases with nephrotic syndrome. TMA was arteriolar and the onset was either subacute or chronic. Morphologically, TMA was evident in the form of subendothelial mucoid substance, hyperplastic arteriopathy and subendothelial mucoid substance with hyperplastic arteriopathy in 2, 4 and 1 case, respectively.
Comparison of cFSGS and treatment-resistant FSGS
Out of 19 cases, 13 (68.42%) had FSGS—not otherwise specified, five (26.31%) had cellular FSGS and one (5.26%) patient had tip variant of FSGS. Compared to patients with steroid and TAC resistant FSGS, patients with cFSGS had higher prevalence of hypertension and serum creatinine at presentation (). There were no differences in 24-h urine protein and serum albumin in patients of cFSGS and resistant FSGS. The details including clinical outcome are mentioned in . At the end of 24 months of stopping TAC therapy; four (21%) patients progressed to ESRD, one (5.2%) expired, five (26.3%) developed progressive chronic kidney disease and nine (47.3%) had persistent proteinuria with normal renal functions. Two patients with ESRD underwent renal transplantation with relapse of the disease.
Discussion
The present study is the first prospective study of cFSGS. In the present study, we observed a very high rate of cFSGS progressing to ESRD. In addition, we also observed that cFSGS had higher serum creatinine at presentation and similar risk of progression to ESRD/death as steroid and TAC-resistant noncollapsing FSGS.
In the present study, nephrotic syndrome and RPRF were the codominant forms of presentation. The prevalence of hypertension, renal dysfunction and steroid responsiveness was similar to that described in other studies. The two-year renal and patient survival was 45%. In earlier studies,Citation3,Citation5,Citation6 renal survival has varied between 33 and 42 months. However, the mean time to progress to ESRD was shorter in the present study compared to that in two earlier studies (13 and 19 months).Citation1,Citation7 Patients presenting with renal failure had higher incidence of TMA and tubulocystic inclusion compared to patients with nephrotic syndrome and was probably responsible for faster progression to ESRD.
In patients with FSGS, response to therapy is the strongest predictor of long-term outcome.Citation2 Patients with CR/PR have better outcome compared to those with no response.Citation2 In patients with SR-FSGS, CNIs viz; cyclosporine/TAC are the second line agents.Citation8,Citation9 A majority of cases respond to CNIs;Citation9 however, a small minority does not respond and progress to ESRD. The long-term prognosis of SR- and CNI-resistant FSGS is not clear. In our cohort, we found 26% of the SR and CNI resistant cases progressed to ESRD/death. At presentation, the results of the study demonstrate that cases with cFSGS have severe degree of renal dysfunction compared to steroid- and TAC-resistant FSGS; this could be explained by severe chronic tubulointerstitial changes and TMA in cases with cFSGS. However, at the end of two years, there were no significant differences in terms of progression to ESRD/death between the groups. The lack of significant difference may be explained by the poor therapeutic response in both the groups.
We noted significant positivity for Ki67, WT1 and PAX2 in cFSGS compared to patients of other FSGS variants. Podocyte dedifferentiation or dysregulation were common in idiopathic and viral associated cFSGS.Citation10 PAX2-positive cells covering the capillary tuft have been reported to be continuous with PAX-2/CK8-positive cells lining Bowman's capsule.Citation11 In the present study, Ki67 was strongly positive in patients with collapse, suggesting ongoing proliferation. PAX-2 was positive only in patients with quiescent collapse. Loss of WT-1 in collapsed glomeruli was universal, suggesting phenotypic dysregulation.
Parvovirus B19 DNA is reported in renal biopsies of 90% of patients with cFSGS and 80% patients with FSGS.Citation12 We found parvovirus B19 DNA in 36% and 15% biopsies of cFSGS and other variants of FSGS, respectively. The prevalence was similar in all groups, suggesting that parvovirus B19 does not significantly contribute to the development of cFSGS in our population. In an autopsy study, parvovirus B19 DNA in the kidney tissue of 10% cases.Citation13
Our study has limitations in terms of small sample size, short duration of follow-up and work-up for hypercoagulability in cases with TMA. To conclude, cases with cFSGS have a dismal outcome and the prognosis of therapy resistant non-collapsing FSGS and cFSGS are similar and lends support to the hypothesis of therapy response being one of the most important predictor of progression to ESRD.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Weiss MA, Daquioag E, Margolin EG, Pollak VE. Nephrotic syndrome, progressive irreversible renal failure, and glomerular “collapse”: A new clinicopathologic entity? Am J Kidney Dis. 1986;7:20–28.
- Rydel JJ, Korbet SM, Borok RZ, Schwartz MM. Focal segmental glomerular sclerosis in adults: Presentation, course, and response to treatment. Am J Kidney Dis. 1995;25:534–542.
- Thomas DB, Franceschini N, Hogan SL, Holder ST, Jennette CE, Falk RJ, et al. Clinical and pathologic characteristics of focal segmental glomerulosclerosis pathologic variants. Kidney Int. 2006;69:920–926.
- Nada R, Kharbanda JK, Bhatti A, Minz RW, Sakhuja V, Joshi K. Primary focal segmental glomerulosclerosis in adults: is the Indian cohort different? Nephrol Dial Transplant. 2009;24:3701–3707.
- Detwiler RK, Falk RJ, Hogan SL, Jennette JC. Collapsing glomerulopathy: A clinically and pathologically distinct variant of focal segmental glomerulosclerosis. Kidney Int. 1994;45:1416–1424.
- Stokes MB, Valeri AM, Markowitz GS, D'Agati VD. Cellular focal segmental glomerulosclerosis: Clinical and pathologic features. Kidney Int. 2006;70:1783–1792.
- Valeri A, Barisoni L, Appel GB, Seigle R, D'Agati V. Idiopathic collapsing focal segmental glomerulosclerosis: A clinicopathologic study. Kidney Int. 1996;50:1734–1746.
- Ramachandran R, Kumar V, Rathi M, et al. Tacrolimus therapy in adult-onset steroid-resistant nephrotic syndrome due to a focal segmental glomerulosclerosis single-center experience. Nephrol Dial Transplant. 2014;29:1918–1924.
- Cattran DC, Appel GB, Hebert LA, et al. A randomized trial of cyclosporine in patients with steroid-resistant focal segmental glomerulosclerosis. North America Nephrotic Syndrome Study Group. Kidney Int. 1999;56:2220–2226.
- Albaqumi M, Barisoni L. Current views on collapsing glomerulopathy. J Am Soc Nephrol. 2008;19:1276–1281.
- Dijkman HB, Weening JJ, Smeets B, et al. Proliferating cells in HIV and pamidronate-associated collapsing focal segmental glomerulosclerosis are parietal epithelial cells. Kidney Int. 2006;70:338–344.
- Tanawattanacharoen S, Falk RJ, Jennette JC, Kopp JB. Parvovirus B19 DNA in kidney tissue of patients with focal segmental glomerulosclerosis. Am J Kidney Dis. 2000;35:1166–1174.
- Aravindh R, Saikia UN, Mishra B, et al. Persistence of human parvovirus B19 in tissues from adult individuals: A comparison with serostatus and its clinical utility. Arch Virol. 2014;159:2371–2376.
