Abstract
Aim: The aim of this study was to compare peritonitis rates, peritoneal dialysis technique survival and patient survival between patients who started peritoneal dialysis earlier than 14 days (early starters) and 14 days or more (delayed starters) after insertion of a Tenckhoff catheter. Methods: Observational analysis was performed for all patients who underwent insertion of a Tenckhoff catheter at Far Eastern Memorial Hospital between 1 January 2006 and 31 December 2012. The patients were divided into two groups: early and delayed starters. The rate and outcomes of peritonitis were recorded. Peritoneal dialysis technique survival and patient survival were analyzed using the Kaplan–Meier method. Cox regression analysis was performed for peritoneal dialysis technique failure and patient mortality. Results: There were 80 early starters and 69 delayed starters. The peritonitis rate was 0.18 episodes per year in early starters and 0.13 episodes per year in delayed starters. There was no significant difference of peritonitis free survival (p = 0.146), peritoneal dialysis technique survival (p = 0.273) and patient survival (p = 0.739) at 1, 3, 5 years between early starters and delayed starters. After adjustment with age, albumin and diabetes, early starters did not have an increased risk of peritonitis, technique failure and mortality compared to delayed starters. Conclusion: Compared to the patients who started peritoneal dialysis 14 days or more after catheter implantation, the patients who started earlier did not have an increased risk of peritonitis, peritoneal dialysis technique failure and mortality.
Introduction
Peritoneal dialysis (PD) is a well-established technique of renal replacement therapy for patients with end-stage renal disease. The advantages of PD include better preservation of residual renal function and better survival in the first few years.Citation1–7 In addition, in Taiwan, the total lifetime cost paid by the National Health Insurance Bureau is significantly lower for PD than for hemodialysis (HD) patients.Citation8 In 2012, about 9% of patients with end-stage renal disease receive PD as long-term renal replacement therapy in Taiwan.Citation9
For a PD program to succeed, the adequate timing of PD catheter implantation and thus starting PD are extremely important. Starting PD early after PD catheter insertion is generally avoided due to the presumed increased risk of infection and dialysate leak.Citation10,Citation11 However, recent studies have reported a very-low incidence of leakage after a short break-in period.Citation12,Citation13 In addition, delaying the start of PD after catheter insertion may prolong patient discomfort from uremic symptoms, and also increase the possibility of HD during the waiting period and the risk of complications associated with HD.Citation14 Several guidelines suggest starting PD at least 14 days after implantation of a PD catheter.Citation15–19 However, there is no consensus in the literature on the optimal time interval between catheter placement and start of PD. The purpose of this study was to compare the outcomes between two groups of patients: those who started PD earlier than 14 days (early starters) and those who started PD 14 days or more (delayed starters) after PD catheter insertion.
Patients and methods
Far Eastern Memorial Hospital is a medical center located in New Taipei City, and approximately 110 PD patients are currently followed at our PD center. All patients who choose PD renal replacement therapy were admitted for insertion of a Tenckhoff catheter when they reach end-stage renal disease. PD training and education concerning PD care were usually started soon after admission. All of these patients received 1 g of intravenous cefazolin immediately before the operation. A low paramedian incision was made and the peritoneum was opened. The Tenckhoff catheter was then inserted into the peritoneal cavity using a guide wire. A subcutaneous tunnel beside the insertion site was created with a trocar, and the Tenckhoff catheter was pulled out to the skin of the left side abdominal wall through the tunnel. The peritoneum and wound were closed layer by layer after fixation of the catheter. Dialysate was infused into the peritoneal cavity to ensure the patency of the catheter and absence of leakage. If the patient had previously undergone abdominal surgery, the above procedure was performed with the assistance of laparoscopy. Occasionally, laparoscopic adhesiolysis was performed during the operation. The patients were discharged 2–5 days after the operation with continued PD training at the PD center. PD was usually started 10–20 days after Tenckhoff catheter implantation depending on the clinical situation of the patient.
Definition of peritonitis
The diagnosis of peritonitis was made based on the presence of at least two of the following signs: cloudy effluent or/and abdominal pain, leukocytes >100 cells per microliter with more than 50% polymorphonuclear neutrophils, and presence of bacteria in the dialysis effluent. Peritonitis which was caused by the same pathogen that caused the immediately preceding episode and occurred within 4 weeks of completion of the antibiotic course was considered relapse and not counted as another episode.
Data collection
A chart review was performed on all patients who started PD at our hospital between 1 January 2006 and 31 Dec 2012. Patients were excluded if they had a Tenckhoff catheter inserted at another hospital, or if they had previously undergone PD before 1 January 2006. If a patient received more than one Tenckhoff catheter insertion during this period, only the first episode was included for analysis. The patients were divided into two groups according to the timing of starting PD: those who started PD earlier than 14 days (early starters) and those who started PD 14 days or more (delayed starters) after PD catheter insertion. All of the patients’ records were collected and analyzed until the time of death, transplantation, transfer, PD failure or 31 Dec 2013, whichever came first.
Statistical analysis
All data was recorded as mean ± standard deviation. Categorical variables were compared using the chi-squared test. Continuous variables were compared using the unpaired Student’s t test. PD technique failure was defined as a transfer to HD for 30 or more than 30 days. The patients who remained on PD at the time of death, transfer or transplantation, were censored. Peritonitis-free survival, PD technique survival and patient survival were analyzed using the Kaplan–Meier method. Poisson regression model was performed for peritonitis rate, with factors and covariates of early or delayed starters, diabetes, age and albumin. Cox regression analysis was performed for PD technique failure and patient mortality, with covariates of early or delayed starters, diabetes, age and albumin. Statistical analysis was performed by PASW for Window software version 18.0 (SPSS, Chicago, IL).
Ethics statement
The Institutional Review Board of Far Eastern Memorial Hospital approved the retrospective cohort study. Written informed consent was not needed because the study retrospectively collected available medical records in the hospital. The Institutional Review Board specifically granted a waiver for the “no consent needed”.
Results
A total of 149 patients were included for analysis, with an average age of 55.6 ± 13.9 years (range 20.2–84.7 years). There were 66 (44.3%) males, and 64 (43%) of the patients had diabetes. The average period of follow-up was 30.5 ± 24.9 months. The overall average interval from implantation of a Tenckhoff catheter to the start of PD was 15.5 ± 9.0 (6–76) days. There were 80 early starters and 69 delayed starters. The interval between the implantation of a PD catheter to the start of PD was 11.0 ± 1.7 (6–13) days in early starters, and 20.7 ± 11.0 (14–76) days in delayed starters. The clinical characteristics of the two groups of patients are shown in . There were no significant differences in gender, age, ratio of diabetes, albumin, creatinine, the ratio of HD support before PD, ratio of PD started in 2010–2012 between the two groups.
Table 1. Clinical characteristics of the patients (n = 149).
Totally 79 patients (45 in early starters and 34 in delayed starters) dropped out of PD during this period. The drop out causes included death(27), transfer to HD(32) transfer to other hospital(9) and transplantation(11). The drop out causes of both groups are shown in .
Table 2. Drop out causes (n = 79).
Peritonitis
During this period of study, 47 patients presented with 60 episodes of peritonitis. Thirty patients of early starters and 17 of delayed starters had at least one episode of peritonitis during the study period. The overall peritonitis rate was 0.16 episodes per year at risk (one episode per 75.8 patient-month) with 0.18 episodes per year at risk (one episode per 65.3 patient-month) in early starters and 0.13 episodes per year at risk (one episode per 95.3 patient-month) in delayed starters. The early starters did not have an increased risk of peritonitis (p = 0.451, RR: 1.227(CI: 0.721–2.089) () compared to delayed starters. The possibilities of a first peritonitis event during the first three months were 11.2% in early starters and 7.4% in delayed starters (p = 0.385).
Table 3. Poisson regression model of peritonitis.
Kaplan–Meier estimation of survival
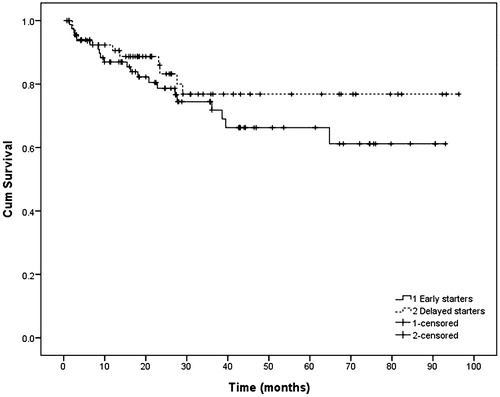
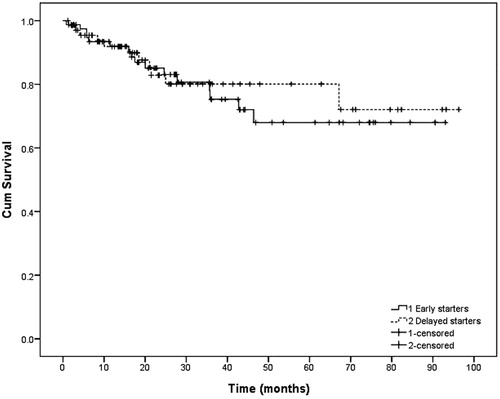
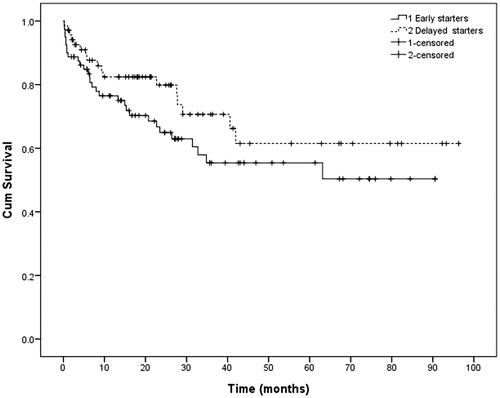
The peritonitis-free survival () at 1, 3, 5 years were 76.5, 55.4 and 55.4% in early starters and 82.4, 70.6 and 61.5% in delayed starters (p = 0.146).The death-censored PD technique survival () at 1, 3 and 5 years were 87.0, 74.5, and 66.3% in early starters, and 90.6, 76.8 and 76.8% in delayed starters (p = 0.273). The overall patient survival () at 1, 3 and 5 years were 91.9, 75.3 and 68.0% in early starters, and 91.9, 80.1 and 80.1% in delayed starters (p = 0.739).
Figure 1. Kaplan–Meier plot of peritonitis free survival according to the timing of starting peritoneal dialysis: early starters versus delayed starters.
Cox multiple regression analysis
After adjustment for age, diabetes, albumin, early starters did not have an increased risk of PD technique failure (p = 0.364, HR: 1.407(CI: 0.673–2.942) () and patient mortality (p = 0.759, HR 0.884 (CI: 0.402–1.943)) (), compared to delayed starters.
Table 4. Multivariate Cox regression model of PD technique failure.
Table 5. Multivariate Cox regression model of patient mortality.
Discussion
The results of this study indicate that the patients who started PD earlier than 14 days did not have a higher risk of peritonitis, PD technique failure and mortality compared to the patients who started PD 14 days or more after the implantation of a PD catheter.
Various clinical practice guidelines suggest that whenever possible, catheter insertion should be performed at least two weeks before starting PD.Citation15–19 Starting PD earlier than 14 days following catheter placement is generally avoided due to concerns that a shorter duration may not allow for adequate healing of the surgical wound, which in turn is presumed to increase the risk of dialysate leakage and therefore resulted in increased infections. There are a few studies assessing the timing of PD initiation after catheter implantation. Most of these studies compared immediate with delayed use of catheters and focused on only short term outcomes. The results were inconsistent. Cheng et al. compared a delayed start (hemodialysis support) with intermittent PD for 4 weeks after catheter insertion in adult patients before commencing continuous ambulatory PD. They found no difference in peritonitis between the two groups, despite the fact that there were more dialysate leaks, cuff erosions and delay in continuous ambulatory PD training in the immediate group.Citation12 A retrospective analysis study by Patel et al. of 33 pediatric patients reported that the delayed use of a catheter (average of 20 days) in 22 patients compared with immediate use in 11 patients resulted in a higher rate of peritonitis at 3 months in the delayed group, and also more exit site and tunnel infectionsCitation10 although dialysate leaks were more common in the immediate group. García Falcón et al. reported that early use of catheter, PD started less than 5 days after catheter implantation, was a risk factor of catheter related complications.Citation20 Leblanc et al. reported an association of early leaks with immediate PD initiation, compared with patients who started PD 10–14 days after catheter implantation.Citation21 However, there were also studies reported favorable outcomes of early catheter usage. Oktay Banli et al. studied 42 patients who started PD on 6th day of PD catheter insertion. They found a very-low rate early leaks (4.8%) as well as peritonitis (2.4%).Citation22 Young-Il et al. studied 51 patients who started PD immediately after catheter implantation and also reported a very low leaks rate, 1.9% at one month and none after one month. Infection rates were low, with a peritonitis rate of 3.9% and an exit site infection rate of 3.9%.Citation14 Sharma et al. showed, by adopting tighter PD catheter securing, the patients who started PD less than 7 days after catheter implantation did not have an increased complication rate, compared to patients who started PD more than 14 days postoperatively.Citation13
The results of above studies were inconclusive about the best timing of PD initiation after catheter implantation. Besides, few of them studied the association of timing of PD commencement with long-term outcomes. We did not have clinical data on dialysate leakage or wound conditions in both patient groups, and therefore we were unable to analyze their associations with the timing of starting PD and infections. However, we did not observe an increased rate of early peritonitis which was presumed to be associated with the condition of surgical wound, in early starters. The overall peritonitis rate and peritonitis free survival on the long term were also similar between these two groups of patients. The peritonitis rate of our study patients is comparable to previous literatureCitation23 and both patient groups achieved the peritonitis rate goal of 0.23–0.29 episodes per year, one episode every 41–52 months, recommended in International Society of Peritoneal Dialysis (ISPD) 2010 guidelines.Citation19 These findings suggested that the ISPD goal of peritonitis rate can be achieved if close attention is continuously paid to training and retraining program and protocols to prevent infection, no matter the timing of initiating PD.
We also compared other long-term outcomes, such as technique survival and overall survival, between these two groups of patients. We did not find an increased risk of technique failure and mortality in the early groups. These two long-term outcomes were rarely studied in previous literatures concerning the timing of PD after catheter implantation. Cheng et al. did not found an increased risk of catheter removal, as well as mortality at 6 months, in patients who started PD immediately, compared to patients with a delayed start (hemodialysis support).Citation12 In this study, the peritonitis rate, technique survival as well as traditional risk factors of death, including age, albumin and ratio of diabetes were similar between these two patient groups, it was not unexpected that these two groups of patients did not have a difference in risk of death.
In conclusion, early start of PD after catheter implantation did not carry an increased risk of peritonitis, PD technique failure and patient mortality. According to the result of this study, the waiting period between the catheter placement and the start of PD might be individualized. Under certain clinical circumstances, such as urgency or the patient’s unwillingness to undergo HD, PD might be started earlier then the recommended two weeks breaking period. The condition of the surgical wound should be assessed carefully to ensure adequate healing, and the patient should receive aggressive PD training before the start of PD. The potential of increased risk of complications, like dialysate leakage or/and infection, should always be kept in mind.
There are several limitations to this study. The sample size is small and it is from a single center. The observational design did not control for possible bias in the initial patient assignment for early or delayed start of PD. The main limitation for the comparisons could be related to selection bias since the assignment of the patients was not performed in a randomized fashion but on a physician, nurse, patient and family combined decision. The retrospective nature of this study also preclude us from obtaining complete and detailed information of several important clinical data, including the serial follow-up of residual renal function. These limitations could be addressed with a multicenter, prospective, randomized, controlled study. A randomized trial is currently being performed to determine the appropriate time to initiate PD after the insertion of catheter,Citation24 and this may help to elucidate the safest and shortest interval between the placement of a PD catheter and starting PD.
Acknowledgements
The authors wish to thank the nursing staff at the peritoneal dialysis center of Far Eastern Memorial Hospital for assisting in the collection of clinical records.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper
References
- Schaubel DE, Morrison HI, Fenton SS. Comparing mortality rates on CAPD/CCPD and hemodialysis. The Canadian experience: Fact or fiction? Perit Dial Int. 1998;18:478–484.
- Collins AJ, Hao W, Xia H, et al. Mortality risks of peritoneal dialysis and hemodialysis. Am J Kidney Dis. 1999;34:1065–1074.
- Termorshuizen F, Korevaar JC, Dekker FW, Van Manen JG, Boeschoten EW, Krediet RT. Hemodialysis and peritoneal dialysis: comparison of adjusted mortality rates according to the duration of dialysis: analysis of The Netherlands Cooperative Study on the Adequacy of Dialysis 2. J Am Soc Nephrol. 2003;14:2851–2860.
- Liem YS, Wong JB, Hunink MG, de Charro FT, Winkelmayer WC. Comparison of hemodialysis and peritoneal dialysis survival in The Netherlands. Kidney Int. 2007;71:153–158.
- McDonald SP, Marshall MR, Johnson DW, Polkinghorne KR. Relationship between dialysis modality and mortality. J. Am. Soc. Nephrol. 2009;20:155–163.
- Yeates K, Zhu N, Vonesh E, Trpeski L, Blake P, Fenton S. Hemodialysis and peritoneal dialysis are associated with similar outcomes for end-stage renal disease treatment in Canada. Nephrol Dial Transplant. 2012;27:3568–3575.
- Jansen MA, Hart AA, Korevaar JC, Dekker FW, Boeschoten EW, Krediet RT. Predictors of the rate of decline of residual renal function in incident dialysis patients. Kidney Int. 2002;62:1046–1053.
- Kao TW, Chang YY, Chen PC, et al. Lifetime costs for peritoneal dialysis and hemodialysis in patients in Taiwan. Perit Dial Int. 2013;33:671–678.
- Taiwan National Health Insurance Database, 2012 Annual Data Report. Available at: http://www.nhi.gov.tw/Resource/webdata. Accessed August 31, 2014.
- Patel UD, Mottes TA, Flynn JT. Delayed compared with immediate use of peritoneal catheter in pediatric peritoneal dialysis. Adv Perit Dial. 2001;17:253–259.
- Newman LN, Tessman M, Hanslik T, Schulak J, Mayes J, Friedlander M. A retrospective view of factors that affect catheter healing: four years of experience. Adv Perit Dial. 1993;9:217–222.
- Cheng YL, Chau KF, Choi KS, Wong FK, Cheng HM, Li CS. Peritoneal catheter-related complications: A comparison between hemodialysis and intermittent peritoneal dialysis in the break-in period. Adv Perit Dial. 1996;12:231–234.
- Sharma AP, Mandhani A, Daniel SP, Filler G. Shorter break-in period is a viable option with tighter PD catheter securing during the insertion. Nephrology (Carlton, Vic). 2008;13:672–676.
- Jo YI, Shin SK, Lee JH, Song JO, Park JH. Immediate initiation of CAPD following percutaneous catheter placement without break-in procedure. Perit Dial Int. 2007;27:179–183.
- Blake PG, Bargman JM, Brimble KS, et al. Clinical practice guidelines and recommendations on peritoneal dialysis adequacy 2011. Perit Dial Int. 2011;31:218–239.
- Dombros N, Dratwa M, Feriani M, et al. European best practice guidelines for peritoneal dialysis. Nephrol Dial Transplant. 2005;20:ix8–ix12.
- Yip T, Lui SL, Lo WK. The choice of peritoneal dialysis catheter implantation technique by nephrologists. Int J Nephrol. 2013;2013:940106. doi: 10.1155/2013/940106
- The CARI guidelines. Evidence for peritonitis treatment and prophylaxis: timing of commencement of dialysis after peritoneal dialysis catheter insertion. Nephrology (Carlton, Vic.). 2004;9:S76–S77.
- Figueiredo A, Goh BL, Jenkins S, et al. Clinical practice guidelines for peritoneal access. Perit Dial Int. 2010;30:424–429.
- García FT, Rodríguez-Carmona A, Pérez FM, et al. Complications of permanent catheter implantation for peritoneal dialysis: Incidence and risk factors. Adv Perit Dial. 1994;10:206–209.
- Leblanc M, Ouimet D, Pichette V. Dialysate leaks in peritoneal dialysis. Semin Dial. 2001;14:50–54.
- Banli O, Altun H, Oztemel A. Early start of CAPD with the Seldinger technique. Perit Dial Int. 2005;25:556–559.
- Piraino B, Bernardini J, Brown E, et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit Dia. Int. 2011;31:624–630.
- Ranganathan D, Baer R, Fassett RG, et al. Randomized controlled trial to determine the appropriate time to initiate peritoneal dialysis after insertion of catheter to minimize complications (Timely PD study). BMC Nephrol. 2010;11:11. doi: 10.1186/1471-2369-11-11.