Abstract
Purpose: To report a case of corneal endotheliitis following the mumps parotitis.
Methods: A 46-year-old man noticed ciliary infection and visual loss in the right eye after mumps parotitis. To determine the cause of the disease, reverse transcription–polymerase chain reaction (RT-PCR) was used to amplify mumps virus RNA in samples from the aqueous humor.
Results: RT-PCR revealed mumps virus RNA in an aqueous humor sample. Although full recovery of vision was achieved within 1 month of the onset, corneal endothelial cells were severely damaged.
Conclusions: The authors have detected mumps virus in the aqueous humor by RT-PCR for the first time.
Corneal endotheliitis can be caused by various virus infections, including herpes simplex virus (HSV), varicella zoster virus (VZV), cytomegalovirus (CMV), or other viruses, such as mumps virus.Citation1–3 We report an adult case of corneal endotheliitis accompanied by detection of mumps RNA in an aqueous humor sample during the resolution phase of mumps parotitis.
Case Description
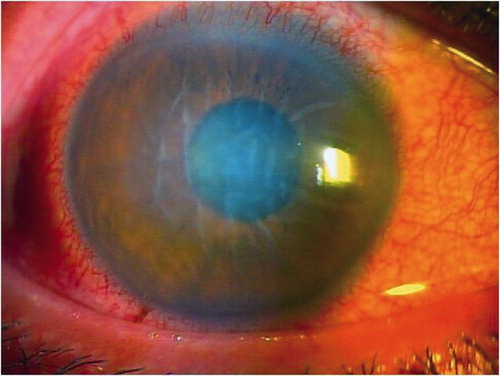
A 46-year-old man presented with redness and hazy vision in the right eye of 2 days’ duration. Seven days before admission he had developed a fever and characteristic swelling of the right parotid glands. IgM antibodies were detected in serum samples using an enzyme-linked immunosorbent assay (ELISA). His physician had diagnosed mumps virus infection. On examination, his vision was counting fingers in the right eye. Intraocular pressure (IOP) using applanation tonometry was 38 mmHg in the right eye. Biomicroscopy showed severe ciliary injection, diffuse corneal stromal edema, folds in Descemet’s membrane, and small pigmental keratic precipitates (KPs) (). The anterior chamber revealed 1+ cells in the right eye. Although the fundus could not be visualized in detail, there was no abnormal roughly. The other eye was completely normal. The anterior chamber was punctured on day 10 after the onset of ocular symptoms. Treatments included topical 0.1% dexamethasone sodium phosphate 6 times a day, 0.04% travoprost, 0.5% timolol maleate, tropicamide, and 5% phenylephrine hydrochloride. We used 0.5% moxifloxacin hydrochloride temporarily due to prevention of secondary infection.
Results
RT-PCR revealed mumps virus RNA in an aqueous humor sample. The total RNA was extracted from an aqueous humor sample using RNAiso Plus (Takarabio, Japan). The RNA was reverse transcribed in the presence of 200 units of reverse transcriptase and synthetic oligonucleotide primers, 5′-CTCATTGGCAATCCAGAGCA-3′ and 5′-ATGAACCTGTTGGTTGGATA-3′. The 223-base pair (bp) PCR products were amplified using RT-PCR as described previouslyCitation4,Citation5 and purified by polyacrylamide gel electrophoresis, which revealed the P gene among mumps virus.
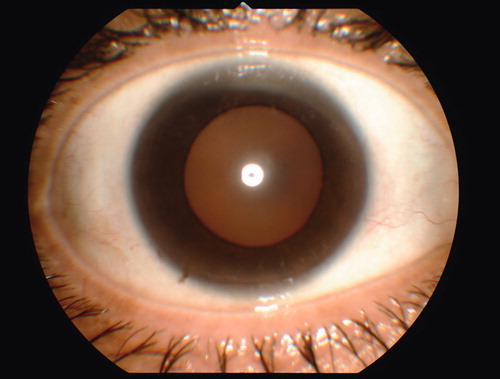
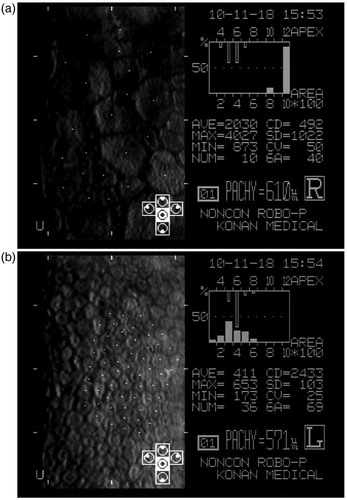
PCR was also performed on an aqueous humor sample to detect DNA of HSV, VZV, CMV, and Epstein-Barr virus (EBV). The results were negative for these viruses. Seven days after treatment, IOP had decreased to within normal limits, and corneal endotheliitis showed improvement. Fundus examination angiography was completely normal, and fluorescein angiography, performed for a more detailed examination, was also normal. One month after onset, vision in the right eye had improved dramatically to 20/20 and corneal endotheliitis showed complete resolution (). The first specular microscopy was performed 3 months after onset, and endothelial cell density was 392–612/mm2 in the affected eye and 2433/mm2 in the other eye (75–84% decrease) (). Endothelial cell density was unchanged in the follow-up after 9 months.
Figure 3. Scan images of the central cornea of both eyes were captured by microscopy 3 months after onset. Six-sided cells were lost and endothelial cell density was 392–612/mm2 in the affected eye (a) and 2433/mm2 in the contralateral eye (b) (75–84% decrease). Central corneal thickness of the affected eye was 610 µm and higher than that of the contralateral eye.
Discussion
Corneal endotheliitis is the rarest of all ocular manifestations of mumps. Typical unilateral symptoms include redness and lacrimation 2–11 days after parotitis, little or no pain, rapid clouding of the cornea, lack of corneal vascularization, and complete recovery of vision in 1–4 weeks.Citation1 To our knowledge, this is the first report to detect mumps RNA in the aqueous humor by RT-PCR in patients with corneal endotheliitis following mumps.
In conclusion, pathology of corneal endotheliitis with mumps has been unclear, and we have detected mumps virus in the aqueous humor by RT-PCR for the first time. Although timely treatment with topical steroids led to full recovery of vision with no residual signs or symptoms quickly, the virus in the aqueous humor severely damaged central corneal endothelial cells. Decreased endothelial cells were the greatest concern and have not changed 9 months after onset, and we will follow up the patient.
Declaration of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Fields J. Ocular manifestations of mumps: a case of mumps keratitis. Am J Ophthalmol. 1947;30:591–595
- Singh K, Sodhi PK. Mumps-induced corneal endotheliitis. Cornea. 2004;23:400–402
- Onal S, Toker E. A rare ocular complication of mumps: kerato-uveitis. Ocul Immunol Inflamm. 2005;13:395–397
- Yamada A, Takeuchi K, Tanabayashi K, et al. Sequence variation of the P gene among mumps virus strains. Virology. 1989;172:374–376
- Yamada A, Takeuchi K, Tanabayashi K. Differentiation of the mumps vaccine strains from the wild virus by the nucleotide sequences of the P gene. Vaccine. 1990;8:553–557