Dear Editor,
Serpiginous choroiditis (SC) is a rare form of uveitis that tends to affect both eyes in patients worldwide. The course is relapsing and progressive, starting at the papilla and spreading centrifugally with geographic chorio-retinal plaques. Yellow creamy edges go on expanding and leaving atrophic central scars. SC etiology is not clear, but an immune-mediated hypersensitivity reaction triggered by tuberculous antigens has been postulated.Citation1,Citation2 The disease often involves the macula, causing severe sight loss.Citation1 Serpiginous choroiditis tends to be refractory to immunosuppressants and steroids, thus different multiple aggressive immunosupressive combinations have been proposed.Citation3 We describe an unusual SC case in which adalimumab monotherapy rapidly induced and maintained remission for more than 1 year.
A 22-year-old Caucasian woman was referred to our center in May 2009 because of 10 months of posterior uveitis progression despite treatment with high-dose steroids. She was otherwise healthy but her mother had a history of necrotizing small-vessel ANCA-positive vasculitis that required kidney transplantation.
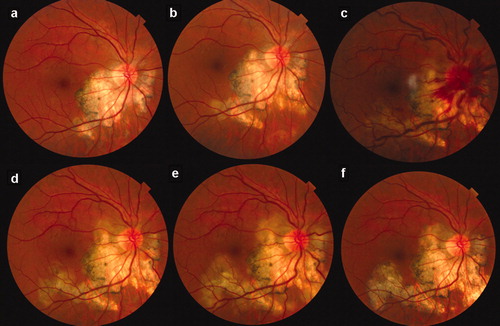
Ophthalmological exploration showed quiet anterior chamber and vitreous cavity in both eyes and a geographic chorio-retinal plaque starting at the papilla and spreading centrifugally with a yellowish creamy edge in the right eye (). Best-corrected visual acuity (BCVA) was 20/20 in both eyes but she complained of a paracentral scotoma in the right eye.
Figure 1. Fundus photographs of serpiginous choroiditis. Progression despite anti-tuberculous treatment (ATT) with oral prednisone (a–d). Papillo-phlebitis developed after 1 month ATT commencement (c). Exacerbation after mycophenolic acid was added (e). Remission after 1 month with adalimumab (f).
Serpiginous choroiditis was diagnosed after ancillary tests. Systemic workup included complete autoimmune analysis, serologic tests (toxoplasma, borrelia, bartonella, Treponema pallidum, and Rickettsia conorii), complete blood cell count, biochemical with ACE, and high-resolution pulmonary scan. All tests were negative or within normal limits, including tuberculin skin test (TST), which measured 15 mm on the fourth day (negative at 72 h). However, an ELISpot for tuberculosis (T-SPOT.TB, Oxford Immunotec, Abingdon, UK) was performed and results were positive. An additional skull base and neck scan was performed because of a concomitant otalgia and it showed an upper left cervical adenopathy of 14 mm with internal contrast enhancement, which was reported as infectious–inflammatory. We performed a fine-needle aspiration that resulted in a very small sample obtention. Culture and smear for mycobacteria were unfortunately negative.
Fluorescein angiography (FAG) showed early hypofluorescence and late hyperfluorescence of the active lesions with late leakage of the edges. Fundus autofluorescence (FAF) showed hyperautofluorescent edges with internal hypoautofluorescence of the chorio-retinal lesions ().
Figure 2. Fundus autofluorescence of serpiginous choroiditis. Progression despite anti-tuberculous treatment and oral prednisone (a–c). Exacerbation after mycophenolic acid was added (d). Remission after 1 month (e) and 1 year (f) with adalimumab monotherapy.
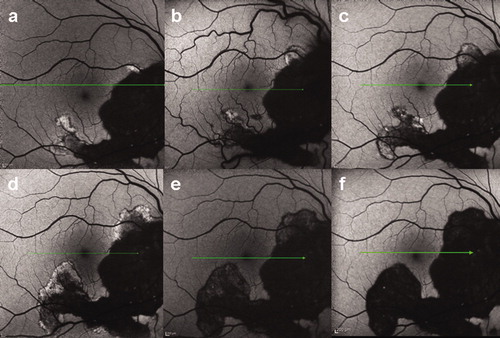
Four-drug anti-tuberculosis treatment (ATT) (isoniazid 5 mg/kg/d, rifampicin 10 mg/kg/d, ethambutol 15 mg/kg/d, and pyrazinamide 25 mg/kg/d) together with steroids 0.5 mg/kg/d were started. An immediate hypersensitivity reaction to isoniazid forced us to withdraw it and continue with only 3 drugs for 1 year. Progression was observed despite ATT treatment along with oral prednisone (0.5–0.1 mg/kg/d) ( and ).
One month after ATT initiation she experienced new visual disturbances in her right eye. Fundus examination showed venous enlargement and hemorrhages starting at the congestive optic disc (). BCVA was 20/20 in either eye with normal exploration in her left eye. A paradoxical ATT reaction with unexpected papillo-phlebitis was suspected and steroids were increased to 1 mg/kg/d. Papillo-phlebitis and chorio-retinitis responded well to a high dose of steroids. However, slow progression and relapses were observed in the following 6 months as steroids were tapered off ( and ). We tried to start cyclosporine 100 mg/12 h but an immediate intolerance reaction required us to withdraw the drug. We then decided to add mycophenolic acid 360 mg/12 h. Unfortunately, low-grade uveitis activity persisted and 2 months later a strong relapse was observed. Therefore, mycophenolic acid dose was increased to 360 mg/8 h and prednisone to 0.7 mg/kg/d. After 1 week new advancing edges of chorio-retinitis threatening the fovea were observed () and FAF showed high hyperautofluorescent edges progressing elsewhere (); thus, mycophenolic acid was withdrawn.
After 1 year of 3-drug ATT, cyclosporine intolerance, exacerbation with mycophenolic acid, and partial response to high-dose steroids, we decided to start anti-TNF-alpha blockade with adalimumab 40 mg/15 days in February 2011. ATT were stopped and low-dose prednisone was maintained.
One month after adalimumab treatment less active chorio-retinal lesions were observed and FAF demonstrated hypoautofluorescent edges of the lesions (). Steroids were tapered off and complete remission was maintained with adalimumab until the last visit in June 2012 ( and ).
Serpiginous choroiditis affects primarily the inner choroid and retinal pigment epithelium and secondarily the retina. Choroidal vascular occlusion, infectious agents, and degenerative processes have been postulated as etiologic theories. Interestingly, veno-occlusive phenomena have been previously described during ATT treatment.Citation4 In our case, papillo-phlebitis appeared just 1 month after 3-drug ATT was started. We interpreted papillo-phlebitis as paradoxical worsening of the condition after ATT because a relapse of chorio-retinitis was also present and responded well to the increased dose of steroids. Tuberculous infection has also been associated with SC in endemic and nonendemic countries since a significantly higher number of patients with SC were interferon-gamma release assay (IGRA) positive compared to healthy and other uveitis controls.Citation2 Furthermore, ATT along with steroids have been capable of inducing SC remission and healing. That was not our case since multiple relapses and continuous activity were present during ATT.
Therapeutic management of SC is unclear. High doses of steroids have been used in the past, leading to a reduction in activity but without achieving remission.Citation1,Citation5 Immunosupressants such as cyclosporine or azathioprine have been tried as steroid sparing and adjuvant treatments with controversial results.Citation3,Citation6 Because of the refractory nature of SC, alkylating agents and triple immunosupressive therapy have proven useful in some patients,Citation7-8 but unfortunately our patient presented intolerance to various drugs, including cyclosporine.
Experience with biologic therapy in SC is very limited. TNF-alpha inhibitors have proven to be efficacious in refractory uveitis. However, only one SC case has been reported to be treated with infliximab in which remission was achieved soon after infusion,Citation9 Latent tuberculosis reactivation with fatal outcome has also been reported in another SC case treated with infliximab,Citation10 thus latent tuberculous infection can be fatally misdiagnosed. In our case, maybe because of long steroid treatment, tuberculin skin test was negative at 72 h. We also performed an ELIspot test that resulted reactive. IGRAs and especially ELIspot are probably more sensitive than TST for tuberculosis detection in these steroid-treated patients. Nevertheless, we maintained 3-drug ATT for 1 year and despite no remission of the SC, it allowed us to safely start the treatment with adalimumab. A close monitoring of the patient is mandatory because a tuberculosis reactivation or reinfection can be possible while under anti-TNF treatment.
In conclusion, we would like to highlight adalimumab as an appropriate treatment alternative for refractory serpiginous choroiditis if tuberculosis has been correctly treated or ruled out.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Lim WK, Buggage RR, Nussenblatt RB. Serpiginous choroiditis. Surv Ophthalmol. 2005;50:231–244
- Mackensen F, Becker MD, Wiehler U, et al. QuantiFERON TB-Gold—a new test strengthening long-suspected tuberculous involvement in serpiginous-like choroiditis. Am J Ophthalmol. 2008;146:761–766
- Akpek EK, Baltatzis S, Yang J, et al. Longterm immunosuppressive treatment of serpiginous choroiditis. Ocul Immunol Inflamm. 2001;9:153–167
- Baglivo E, Boudjema S, Pieh C, et al. Vascular occlusion in serpiginous choroidopathy. Br J Ophthalmol. 2005;89:387–388
- Markomichelakis NN, Halkiadakis I, Papaeythymiou-Orchan S, et al. Intravenous pulse methylprednisolone therapy for acute treatment of serpiginous choroiditis. Ocul Immunol Inflamm. 2006;14:29–33
- Araujo AA, Wells AP, Dick AD, et al. Early treatment with cyclosporin in serpiginous choroidopathy maintains remission and good visual outcome. Br J Ophthalmol. 2000;84:979–982
- Akpek EK, Jabs DA, Tessler HH, et al. Successful treatment of serpiginous choroiditis with alkylating agents. Ophthalmology. 2002;109:1506–1513
- Hooper PL, Kaplan HJ. Triple agent immunosuppression in serpiginous choroiditis. Ophthalmology. 1991;98:944–951
- Seve P, Mennesson E, Grange JD, et al. Infliximab in serpiginous choroiditis. Acta Ophthalmol. 2010;88:342–243
- Cordero-Coma M, Benito MF, Hernández AM, et al. Serpiginous choroiditis. Ophthalmology. 2008;115:1633