Abstract
An inflammation or injury to optic nerve anywhere its pathway by extrinsic lesions causes the optic neuropathy. These lesions are more effective in confined spaces like optic canal, orbital apex. We present a 61 year old woman with optic neuropathy due to lesion in an Onodi cell. In this case patient presented with progressive loss of vision in her right eye within a few days. Computed tomography (CT) revealed mucosal thickening and inflammatory signs in right sphenoid sinus and presence of Onodi cell in that side. Magnetic Resonance Imaging confirmed compression to the optic nevre. Systemic antibioterapy and endoscopic sinus surgery was performed. Postoperatively, the visual acuity and control CT views were better than initial findings. Histopathologic evaluation revealed polyps in Onodi cell. Ophthalmologists should be aware of the Onodi cell pathologies that caused compressive optic neuropathy.
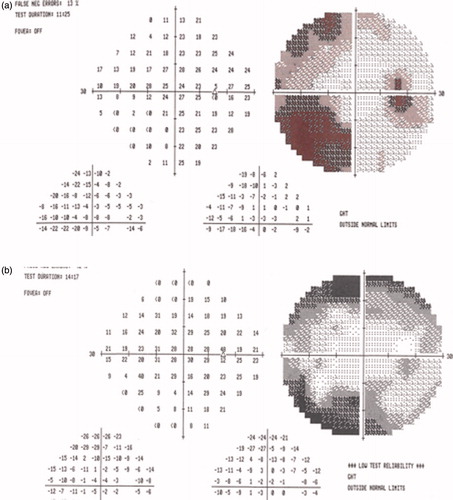
A 61-year-old woman with acute visual loss accompanied by pain in her right eye presented at the ophthalmology department of the Medicine Faculty at Ondokuz Mayis University in Samsun, Turkey. Her left eye had deteriorated 2 years earlier. Her visual acuity was 20/200 right and 20/100 left. The anterior eye segment and ocular pressure were normal in both eyes. The right optic disc was swollen and had blurred margins, and a macular star was observed. The left disc was pale. There was no relative afferent pupillary defect. Visual fields showed nerve fiber bundle defects (). The sedimentation rate was 44 mm/h and CRP 17 mg/L, but all other biochemical, hematologic, and immunological markers were normal.
Figure 1. (a) There was peripheral depression on the right visual field test. (b) The postoperative right visual field test was lighter than at first.
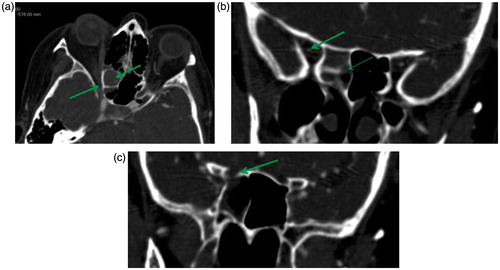
Orbital and cranial magnetic resonance imaging (MRI) revealed mucosal thickening in the right sphenoid and posterior ethmoid sinuses. Due to these MRI findings, we determined that advanced radiological imaging in the form of thin-slice paranasal computed tomography (CT) was necessary to demonstrate the Onodi cell. Polypoid soft tissue was evident around the right optic canal (). On the enhanced MRI scans, increased contrast uptake around the right optic nerve was considered to be venous congestion secondary to compression or an inflammatory retroorbital condition. Paranasal CT images supported our interpretations of the MRI findings and also revealed the presence of an Onodi cell ().
Figure 2. (a) MRI scan shows that inflamed tissue spread to the orbital apex and encircled the optic nerve. (b) Coronal MRI scans support the sagittal images.
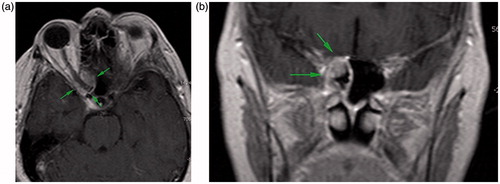
Figure 3. (a) A CT scan shows mucosal thickening on the right spheno-ethmoidal components and also the Onodi cell. Around the right optic canal, the thickening of the mucosa was more evident. This mass suggested a polypoid soft tissue. (b) The Onodi cell wall was intact. The thick arrow shows an optic nerve slice on the orbital apex. There is a gap (thin arrow) between the Onodi cell and the sphenoidal sinus. (c) The sphenoidal sinus wall was defective at the orbital apex.
Intravenous antibiotheraphy was administered and endoscopic sinus surgery (ESS) was performed. There were nasal polyposes in the ethmoidal cells and in front of the sphenoidal sinus ostium. Polypoid soft tissues were also present in the Onodi cell. The polypoid tissues in the Onodi cell and sphenoid sinus were removed and the optic nerve was defined by ESS. The histopathological result for the specimen was sinonasal polyp.
Ten days after surgery, visual acuities were 20/40 and 20/63 in the right and left eyes, respectively. We concluded that visual acuity of the left eye was not improved by treatment. Many measurements of visual acuity were made for both eyes. Especially in the left eye there was variation in acuity; a few measurements were 20/63 and a few others were 20/100, which may have resulted from poor patient cooperation. Visual field tests for her left eye gave stable results. We weren't able to determine the etiology of visual loss in the left eye but we suspected nonarteritic ischemic optic neuropathy because there was no contact between the Onodi cell and left optic nerve. Funduscopic examination yielded the same result.
DISCUSSION
The Onodi cell was first described by Adolf Onodi in 1904.Citation1,Citation2 It is an anatomical variant of the posterior ethmoidal cells that surround the optic nerve and is ventilated by the sphenoid sinuses.Citation2,Citation3 When the migration of the posterior ethmoidal cells is completed, the Onodi cell occurs around the optic nerve.Citation2
In the literature, the incidence of an Onodi cell is from 8 to 13% in radiological findings but the rate is 60% in cadaveric studies.Citation3 Many cases of spheno-ethmoidal mucoceles with visual disturbances have been reported. However, pathology of an Onodi cell is rareCitation1; case reports are more prevalent in the Far East than in Western countries. As a result of the close anatomic relationship between the Onodi cell and the optic nerve, Onodi cell pathologies may result in ophthalmologic complications.
We report a patient who presented with decreased visual acuity due to optic neuropathy because of polyps in an Onodi cell and sphenoidal sinus inflammation. Our case is instructive and demonstrates that etiologies of compressive and inflammatory optic neuropathy can be Onodi cell and sphenoidal sinus lesions. Being cognizant of the presence of an Onodi cell is important for the diagnosis of rhinogenic optic neuropathies and also for the avoidance of iatrogenic injuries of the optic nerve during ESS.
Optic neuropathy is caused by mechanical compression of the optic nerve, circulatory disturbance of the vasa nervorum due to the mechanic compression, or optic neuritis due to inflammation. Because of the presence of a macular star, we suspected that a retrobulbar region infection spread throughout the optic nerve to the right papilla and caused neuroretinitis. For that reason and due to the patient's positive response to therapy, we decided not to conduct an advanced search for the etiology of the neuroretinitis. In our case, the Onodi cell wall closest to the orbital apex was intact (). However, the consecutive slices of the coronal CT scans revealed that the spheniodal sinus wall was defective () and that there was a gap between the sphenoidal sinus and Onodi cell walls.
It is understood that air circulation in the Onodi cell is worse than that of the other sinuses. For that reason, the Onodi cell is predisposed to infections and it may be the starting point for sphenoidal infection. The MRI scans in our case revealed that the inflammation in the sphenoidal wall defect had spread to the orbital apex and encircled the optic nerve ().
Radiologic imaging is essential to preoperative diagnosisCitation2; specifically, CT scans are required to demonstrate anatomical variations. If the thickness of the slices is greater than the width of the Onodi cell, variations cannot be differentiated.Citation3 MRI scans are also required to determine the protein content of the Onodi cell material and to differentiate the nature of the lesion,Citation3 including mucocele, pyocele, and tumor.Citation1
Onodi cell infections frequently cause acute visual loss that can be reversed with early treatment.Citation4 In our case, visual acuity increased from 20/200 to 20/40 and the right visual field was lighter than before surgery (). Medical treatment can improve visual acuity but the fundamental treatment is surgery.Citation2 The best surgical approach is the subject of conjecture among surgeons. The transcranial approach may minimize the risk of optic nerve injury when a small Onodi cell mucocele is close to the optic nerve. However, brain parenchyma injury, leakage of cerebrospinal fluid, and possible contamination of the cerebrospinal fluid by mucocele contents are frequent and serious complications of this approach.Citation1 The endoscopic, transnasal approach lacks these complications and is a less invasive technique. In the present case, the endoscopic transnasal approach was performed and the pathology was completely removed without complications.
Onodi cell pathologies as a cause of optic neuropathy should always be kept in mind by the ophthalmologist. Axial and coronal CT and MRI images are essential for correct diagnosis. Visual loss can be improved with early treatment. Ophthalmologists and otorhinolaryngologists should evaluate these patients together so as not to overlook these types of pathologies.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Fukuda H, Fukumitsu R, Andoh M, et al. Small Onodi cell mucocele causing chronic optic neuropathy. Neurol Med Chir. 2010;50:953–955
- Toh ST, Lee JC. Onodi cell mucocele: rare cause of optic compressive neuropathy. Arch Otolaryngol Head Neck Surg. 2007;133:1153–1156
- Wu W, Sun MT, Cannon PS, et al. Recovery of visual function in a patient with an Onodi cell mucocele compressive optic neuropathy who had a 5-week interval between onset and surgical intervention: a case report. J Ophthalmol. 2010;2010:483056–483058
- Chee E, Looi A. Onodi sinusitis presenting with orbital apex syndrome. Orbit. 2009;28:422–424