Abstract
Acute leukemia commonly renders a child immunocompromised, making them susceptible to opportunistic microorganism infection.We report an interesting case that presented to us with multifocal choroiditis secondary to Candida albicans infection in a Leukemic child. Appropriate management was undertaken and the infection subsided.
Opportunistic microorganisms commonly cause infection in immunocompromised children. The same infection spreading to the eye tissues, especially the choroid, is not frequently encountered. The authors report a 13-year-old boy with acute myeloid leukemia presenting with multifocal choroiditis secondary to Candida albicans infection. A course of intravenous antifungals showed marked improvements to the choroidal lesions.
CASE REPORT
A 13-year-old Chinese boy, a known case of acute myeloid leukemia in remission awaiting hematopoietic stem cell transplantation (HSCT), was admitted to the pediatric ward with a 5-day history of fever. He was diagnosed as having neutropenic sepsis secondary to myelosuppresive chemotherapy for his leukemia. Past medical history revealed that the patient was diagnosed to have acute myeloid leukemia in September 2010. In July 2011, he relapsed with a lineage switch from myeloid to T lymphoid lineage. The patient was subsequently treated with chemotherapy. The plan was to induce durable complete remission followed by HSCT to afford a reasonable chance of cure for the patient. Prior to the diagnosis of his leukemia, the patient was well with a normal antenatal, intranatal, and postnatal history. He had completed his routine vaccinations. The patient is the second of four siblings and the other three siblings are all medically fit. There was no history of congenital immunodeficiency in the patient or the family members.
The patient achieved complete remission with induction treatment () and was subsequently given central nervous system (CNS) directed therapy (), after which the patient was deemed ready to undergo HSCT. However, the patient was found to have skin lesions around the central venous line (CVL) catheter site that grew Candida albicans, as determined from the skin scrapings. The CVL was removed. The blood fungal culture also grew Candida albicans.
TABLE 1. Patients chemotherapy regime following diagnosis of T-ALL on 27 July 2011 and prior to the systemic fungal infection.
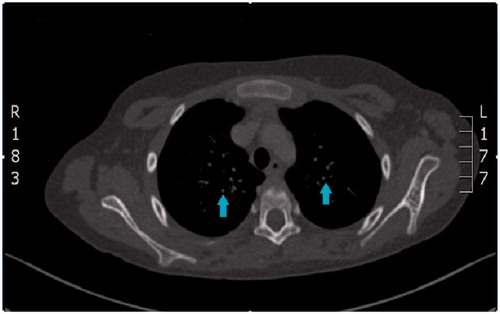
A computed tomography (CT) scan of the thorax and abdomen was done to look for metastatic fungal disease. Multiple small nodules of less than 0.5 cm were seen scattered throughout both lung fields and were associated with scattered focal fibrosis and pleural thickening suggestive of disseminated fungal disease (). Both kidneys appeared prominent with hypodense lesions, each measuring about 0.2 cm, suggestive of possible fungal lesions.
FIGURE 1. Multiple small nodules, less than 0.5 cm (arrows pointing to the lesions) are seen scattered throughout both lung fields associated with scattered focal fibrosis and pleural thickening.
The patient was referred for an ophthalmology consultation to look for fungal balls in the eye. Visual acuity was 20/20 in each eye and the patient denied any visual symptoms. Anterior segment findings and intraocular pressures were unremarkable. However, multifocal, well-circumscribed, whitish creamy lesions were seen scattered throughout the choroid of both eyes (). No vitritis, retinal hemorrhages, cotton wool spots, or vasculitic lesions were seen.
FIGURE 2. Multifocal creamy white, well circumscribed lesions seen in the choroid (arrow pointing to the lesions) during the first eye visit.

A lumbar puncture done during the present admission showed that the cerebrospinal fluid was negative for Candida. No organisms, erthryocyte or leucocyte, were detected in the cerebrospinal fluid. Protein levels were normal at 0.15 mg/dL and the glucose level was 3.6 mmol/L with corresponding serum glucose of 6.3 mmol/L. India ink staining was negative for encapsulated fungus. Cerebrospinal fluid culture and sensitivity were negative as well. Serum virology was negative for Rubella, Cytomegalovirus, and toxoplasmosis.
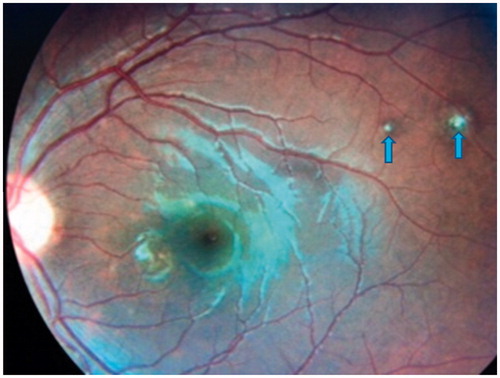
Due to the presence of disseminated fungal disease, the patient was treated with intravenous amphotericin B 33 mg over 6 h daily (1 mg/kg/dose) for 2 weeks and intravenous fluconazole 380 mg daily (12 mg/kg/dose) for 1 week followed by oral fluconazole 400 mg twice daily for 6 weeks. Close monitoring of liver and renal functions tests was done to look for potential drug toxicities. The patient responded well to the antifungals with resolution of his fever and scarring of the choroidal lesions ( and ). Repeat CT scan of the thorax and abdomen 1 month after treatment revealed resolving fungal infections. The blood culture prior to discharge was sterile.
FIGURE 3. Right eye fundus photo revealing scarred multifocal choroiditis (arrow pointing to the lesions), post intravenous antifungal completion.
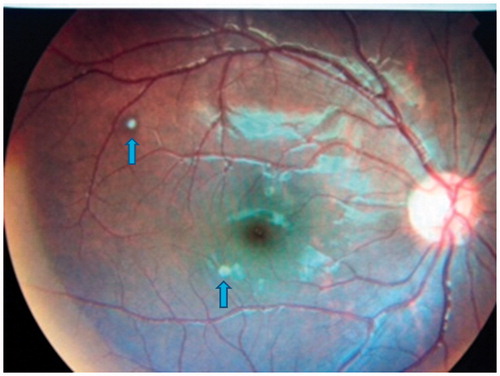
FIGURE 4. Left eye fundus photo revealing the multifocal choroiditis healing and scarring (arrows pointing to the lesions) post intravenous antifungal completion.
Two months later, during his next follow-up, it was noted that he had no recurrence of the fungal lesions in either eye nor any systemic fungal infections. Hence, preparation was made for HSCT, which had been postponed earlier. Unfortunately, his ALL relapsed again in June 2012. He underwent treatment with BFM (Berlin-Frankfurt-Munich) 2002 relapse protocol chemotherapy regime. The patient received a combination of chemotherapy regimes known as R1 block, R2 block, F1 block, and F2 block over a period of 27 weeks. The first combination of F1 block comprised prednisolone, vincristine, methotrexate, E. coli asparaginase, cytarabine, and dexamethasone. This was followed by the F2 regime, given 3 weeks later, comprising the same drugs but the cytarabine was given twice (once intravenously and once intrathecally). Next, 4 courses of R1 block and 4 courses of R2 block were given alternatively every 3 weeks, starting with R2. R1 consisted of dexamethasone, mercaptopurine, vincristine, cytarabine, E. coli asparaginase, methotrexate, and prednisolone. R2 consisted of dexamethasone, thioguanine, vindesine, methotrexate, ifosfamide, daunorubicine, E. coli asparaginase, cytarabine, and prednisolone. He is currently in his third remission and awaiting HSCT in December 2012.
DISCUSSION
Patients with leukemia are susceptible to develop rare and potentially life-threatening infections during periods of neutropenia. The infections could occur as a result of the underlying disease or chemotherapy. These patients are prone to all forms of microorganisms, from viral, bacterial, and protozoal to fungal in nature.Citation[1]
Fungus is a common cause of ocular infection in leukemia, as seen in this patient. The severity of this infection ranges from mild mucocutaneous infections to severe invasive disease that potentially involves any organ. Over the last few years, the incidence of invasive candidiasis, in particular candidemia, has increased significantly. Candida is a type of yeast, responsible for the majority of fungal infections in humans. Candida species is the fourth most common pathogen isolated in blood cultures in the United States.Citation[2] Immunocompromised patients, such as those affected by solid tumors or hematological malignancies, are at high risk for developing Candida infection.Citation[2] Broad-spectrum antibiotics, abdominal surgery, indwelling central venous lines, parenteral nutrition, and cytotoxic chemotherapy have also contributed to the high incidence of this particular type of fungal infection.Citation[3]
Fungemia secondary to Candida species commonly involves the eye as well. The most common features of candidal infections to the eye are uveitis and retinitis with characteristic cotton balls in the vitreous.Citation[3] Some of the rarely reported features include either focal or multifocal chorioretinitis or chorioretinitis with accompanying vitritis suggestive of an endophthalmitis.Citation[3] It is possible for Candida to spread hematogenously to the choroid and retina without extending into the vitreous. The main risk factor for chorioretinitis caused by Candida infections is fungemia with Candida albicans, as non-albicans species do not cause chorioretinitis.Citation[4] Other risk factors include multiple positive blood cultures for Candida albicans, visual symptoms, and compromised immunity.Citation[4]
The fundus lesions in this case appeared as multifocal, well-circumscribed, whitish, creamy choroid lesions with a histoplasmosis-like appearance. What is interesting about the lesions in this case is that they differ from the typical appearance of Candida fungus balls, vitritis, chorioretinitis, and endophthalmitis, which are more commonly encountered in candidal infections of the eye. Although no direct pathologic studies have been done on the eye lesions to support the diagnosis of candidemia, the positive skin scrapings, positive fungal blood cultures, and good response to anti-fungal treatment all indirectly support the diagnosis for Candida infection of the eye. This patient presented only with multifocal choroiditis without retinal involvement.
Prior to the advent of highly active antiretroviral therapy (HAART), infectious opportunistic multifocal choroiditis caused by Candida was much more frequently seen in patients suffering from acquired immune deficiency syndrome (AIDS).Citation[5] We believe this is the first reported case of candidal sepsis from CVL infection causing multifocal choroiditis in an immunosuppressed child with hematological malignancy. The atypical presentation of only multifocal choroiditis in this case should alert clinicians to be more wary of other possible clinical presentations of candidal infection to the eye besides the usual fungal balls and endophthalmitis, which are more commonly encountered.
The rate of developing chorioretinitis in patients with candidemia has reduced markedly since the 1990s due to the early identification of candidemia in blood cultures coupled with a trend of early empiric antifungal therapy.Citation[4] It was suggested that when systemic antifungal agents are given early in the course of Candida fungemia, chorioretinal lesions do not progress to endophthalmitis. Patients with a history of sepsis and endogenous chorioretinitis have a risk of developing choroidal neovascularization.Citation[6] This is a potential cause of late visual loss that should be monitored by the ophthalmologist in the long-term follow-up of these patients.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Sharma T, Grewal J, Gupta S, Murray PI. Ophthalmic manifestations of acute leukaemias: the ophthalmologist's role. Eye 2004;18:663–672
- Mikulska M, Bassetti M, Ratto S, Viscoli C. Invasive candidiasis in non-hematological patients. Mediterranean J Hematol Infectious Dis. 2011;3
- Mehta S, Jiandani P, Desai M. Ocular lesions in disseminated candidiasis. J Assoc Physicians India. 2007;55:483–485
- Mateo J, Ascaso FJ, Núñez E, et al. (2011). Ophthalmological Manifestations in Acute Lymphoblastic Leukemia, Novel Aspects in Acute Lymphoblastic Leukemia. In Faderl S (ed.), In Tech. ISBN: 978-953-307-753-6. Available from: http://www.intechopen.com/books/novel-aspects-in-acute-lymphoblastic-leukemia/ophthalmologicalmanifestations-in-acute-lymphoblastic-leukemia [last accessed March 2013]
- Morinelli EN, Dugel PU, Riffenburgh R, Rao NA. Infectious multifocal choroiditis in patients with acquired immune deficiency syndrome. Ophthalmology 1993;100:1014–1021
- Thomas PA. Current perspectives on ophthalmic mycoses. Am Soc Microbiol Clin Microbiol. 2003;16:730–797