A 7-year-old Yemeni male with no significant past medical or surgical history was referred for evaluation of bilateral corneal infiltrates two months after emigration to the United States. He complained of chronic itching, worse in the spring but persistent throughout the year, and moderate photophobia for 5 years. He was first seen by an ophthalmologist in Yemen 5 years prior who diagnosed allergic conjunctivitis. He had been treated unsuccessfully with a number of different oral and topical medications, most recently with topical steroid (Cortiphenol H) and topical antibacterial/antiprotozoal (Furazol).
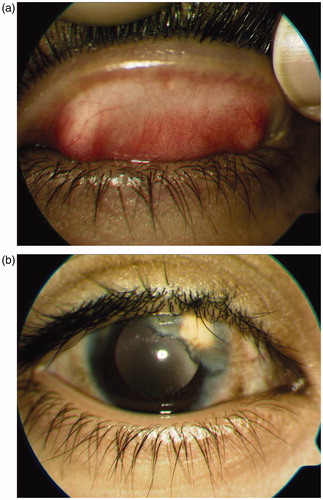
Best-corrected vision with spectacles on initial presentation was 20/100 OD and 20/80 OS. Slit-lamp examination revealed diffuse fine papillary reaction of the palpebral conjunctiva in both eyes, greater superiorly (). Corneal examination showed superior pannus and neovascularization with associated stromal lipid deposition OU (). Anterior chambers were quiet. Cycloplegic retinoscopy revealed marked scissoring consistent with irregular astigmatism. Dilated funduscopic examination showed healthy nerves and a normal retinal exam.
FIGURE 1. (a) Superior palpebral conjunctiva on presentation showing a diffuse, fine papillary reaction. (b) Slit-lamp photograph of the right eye showing corneal neovascularization and associated lipid deposition.
Our leading diagnosis was chronic allergic conjunctivitis. The patient was started on olopatadine 0.1% bid OU, loteprednol etabonate 0.5% qid OU, and oral cetirizine daily. Upon follow-up 1 month later, there was no significant improvement in vision or clinical exam. Given that trachoma is endemic in Yemen, a co-existent infectious etiology was also considered. A conjunctival scraping from the right palpebral conjunctiva was sent for culture and PCR. Cytological examination showed moderate PMNs on Gram stain. Giemsa revealed inflammatory cells. PCR for Chlamydia trachomatis was negative. Given the lack of response to anti-inflammatory therapy, and high index of clinical suspicion for trachoma, the patient was given empiric treatment for trachoma with oral azithryomycin 250 mg po daily for 2 weeks and topical erythromycin drops qid OU.
At next follow-up, he had improvement in subjective symptoms but clinical examination was unchanged. He underwent a biopsy from the bulbar conjunctiva in the superior limbal area of the right eye. Histopathologic examination of the Giemsa-stained specimen was notable for eosinophils and intracytoplasmic perinuclear inclusion bodies, consistent with a diagnosis of Chlamydia trachomatis (). The patient was treated with one oral dose of azithromycin 500 mg and 6 months of azithryomycin 1% eyedrops qid and remained on olopatadine 0.1% bid, loteprednol etabonate 0.5%, and oral cetirizine.
FIGURE 2. (a) Pathology slide showing intracytoplasmic inclusion bodies (arrow). (b) Slit-lamp photograph 6 months after treatment of trachoma showing a marked inprovement in pannus and lipid deposition.
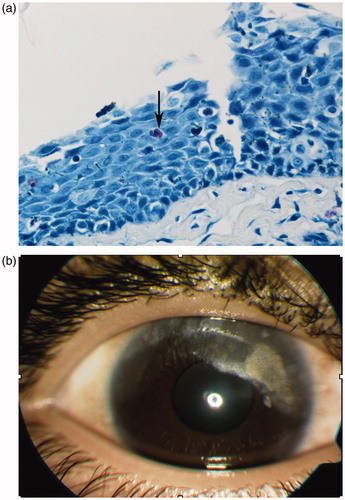
The patient's papillary reaction resolved, corneal neovascularization regressed with significant clearing of the associated lipid deposition over the next 6 months (). Visual acuity improved to 20/20 OU via overrefraction with hard contact lenses.
DISCUSSION
There is a high incidence of chronic allergic conjunctivitis in the general population and there can be numerous challenges in management, including when to undertake further testing for infectious etiology. There is a relatively high rate of co-existent infection, with Forte et al. reporting a 37% incidence of latent co-infections in patients diagnosed with chronic allergic conjunctivitis. Of note, Chlamydia trachomatis was common, diagnosed 30% of the time.Citation1 Our case highlights the importance of undertaking further testing when a condition such as ocular allergy is not responding to standard treatments given the possibility of an infectious and inflammatory condition co-existing, especially in patients from areas where trachoma is endemic.
Although trachoma is most often a clinical diagnosis, there are times where ocular signs are not classic, as shown by this case. Diagnosis can further be complicated by clinical symptoms that persist despite eradication of the organism,Citation2 and diagnostic tests are often suboptimal for diagnosis. Conjunctival scrapings with Giemsa stain offer a sensitivity of 30–60% and specificity of 50–70%, conjunctival cultures improve sensitivity to 50–70% and specificity to 100%.Citation3 PCR offers sensitivity of 60–80% and a specificity of 95–100%.Citation3 Thus, a negative PCR does not rule out presence of disease. In this case, conjunctival scrapings may not have offered the optimal specimen for diagnostic testing, which could explain the initial negative result.
This case highlights the importance of persistence in identifying the correct diagnosis and the clinical success that results with appropriate treatment measures.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Forte R, Cennamo G, Del Prete S, et al. Allergic conjunctivitis and latent infections. Cornea. 2009;28:839–842
- Keenan JD, Lakew T, Alemayehu W, et al. Clinical activity and polymerase chain reaction evidence of chlamydial infection after repeated mass antibiotic treatments for trachoma. Am J Trop Med Hygiene. 2010;82:482–477
- Solomon A, Peeling R, Foster A, Mabey D. Diagnosis and assessment of trachoma. Clin Microbiol Rev. Oct 2004;4:982–1011