Abstract
Purpose: To report a case of infectious keratitis due to Microsporidium after collagen crosslinking (CXL).
Methods: A 36-year-old man presented with a 3-day history of pain, redness and diminution of vision in his left eye. The patient had received CXL for keratoconus in the left eye 6 days prior to presentation. Best-corrected visual acuity (BCVA) was 20/25 OD and counting fingers OS. Slit lamp examination of the left eye showed a central epithelial defect measuring and multiple stromal infiltrates.
Results: Gram and Giemsa staining of corneal scrapings showed spores characteristic of Microsporidia. Hourly 0.5% moxifloxacin eye drops, 0.5% moxifloxcain eye ointment nocte and oral albendazole 400 mg twice daily were commenced. Corneal debridement was performed twice during the first week. At the end of 6 weeks BCVA was 20/60 in the left eye.
Conclusions: Microsporidial infection can be confirmed on microbiological examination. Our case responded well to medical treatment alone.
Postsurgical infectious keratitis is a rare complication that can cause serious ocular morbidity and even complete loss of vision. The surgical technique of collagen cross-linking involves the removal of epithelium intraoperatively. It has been associated with the occurrence of infectious keratitis in the postoperative period.Citation1–8 We present a case of microsporidial keratitis after collagen cross-linking.
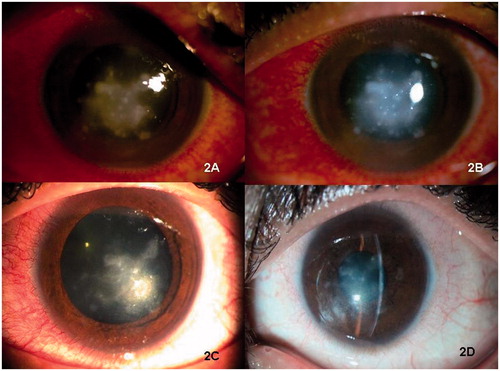
A 36-year-old man presented to outpatient department of our hospital with a 3-day history of pain, redness, and diminution of vision in his left eye. The patient had received corneal collagen cross-linking (CXL) treatment for keratoconus in the left eye 6 days prior to presentation at eye hospital. Postoperative treatment after CXL included 0.5% moxifloxacin hydrochloride eyedrops 4 times a day, 0.1% fluorometholone 4 times a day, and preservative-free eye artificial tear drops 6 times a day. A bandage contact lens was inserted at the end of the surgery. According to the patient, he was seen on the first postoperative day and was asked to continue the same treatment. On day 4 after the surgery, the patient presented to his surgeon with complaints of pain, redness, marked light sensitivity, and diminution of vision in the operated eye. The surgeon noticed multiple small corneal infiltrates. A presumptive diagnosis of infectious keratitis was made and empirical treatment was commenced in the form of hourly 0.5% moxifloxacin hydrochloride, hourly 1.3% tobramycin, hourly 5% natamycin, and 1% atropine 3 times a day in the left eye. However, clinical deterioration was noted over the next 48 h and the patient was referred to our center. At the time of presentation to our center, the best-corrected visual acuity (BCVA) was 20/25 OD and counting fingers OS. Slit-lamp examination of the left eye showed marked conjunctival injection. A central, large epithelial defect measuring 7.5 × 6.0 mm was noted on the corneal surface along with multiple coarse, pinhead-size anterior stromal infiltrates (). The intervening cornea was edematous and hazy. There was mild anterior chamber reaction. Details of the anterior segment could not be examined due to edema and haze of the intervening cornea. Ultrasound for posterior segment evaluation did not reveal any abnormality. The results of previous microbiological evaluation of corneal scrapings or bandage contact lens could not be traced. Repeat corneal scrapings were obtained and submitted for Gram stain, Giemsa stain, chocolate agar, Sabouraud dextrose agar, and thioglycollate broth. In addition, venous blood was sent for fasting blood sugar, complete hemogram, and ELISA for detection of HIV. Gram and Giemsa staining showed spores characteristic of microsporidia (). Laboratory blood examination was within normal limits. Hourly 0.5% moxifloxacin hydrochloride eyedrops, 2% homatropine eyedrops 4 times a day, 0.5% moxifloxcain eye ointment nocte, and oral albendazole 400 mg twice daily were commenced. Corneal debridement was performed twice during the first week of admission. A slow clinical response was observed over a period of the next 2 weeks and the patient became symptomatically better. Oral albendazole was continued for 6 weeks. The corneal infiltrates decreased in size and number and eventually disappeared at the end of 6 weeks, leaving a midstromal corneal scar. At the end of 6 weeks, the BCVA was 20/60 in the left eye. The patient is currently waiting for an anterior lamellar keratoplasty in his left eye ().
FIGURE 1. (A) Giemsa staining of smear showing microsporidial spores. (B) Clinical photograph showing multiple corneal infiltrates at the time of presentation in a case with post-collagen cross-linking keratitis.
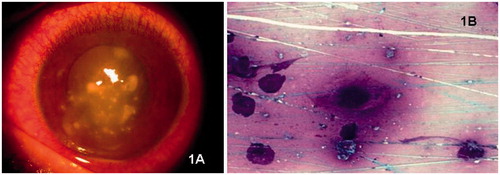
FIGURE 2. Clinical photographs showing gradual resolution of corneal infection after (A) 4 days, (B) 9 days, (C) 1 month, and (D) 3 months after treatment in a case with post-collagen cross-linking keratitis.
The published literature on post-CXL keratitis includes reports of infection with Staphylococcus epidermidis,Citation1 herpes simplex virus,Citation2 Acanthamoeba,Citation3 Pseudomonas aeruginosa,Citation4 Fusarium solani,Citation5 and, Escherichia coli.Citation6 Zamora et al.Citation7 have reported a case of polymicrobial keratitis caused by Streptococcus salivarius and coagulase negative Staphylococcus after CXL. To best of our knowledge, we report the first case of microsporidial keratitis after CXL. The clinical features in our case were typical of corneal microsporidial infections reported in the literature.Citation8 In addition, microbiological evaluation revealed spores on Gram and Giemsa staining. This is an important method to detect microsporidial infections since culturing these organisms from clinical specimens is difficult and diagnostic serologic tests are not available. Currently there are no defined guidelines for the treatment of ocular microsporidial infections. The described treatments include topical fumagillin, topical propamidine isethionate, topical hexamidine, systemic albendazole, and systemic itraconazole.Citation9 In our case, epithelial debridement, topical moxifloxacin, and oral albendazole led to a successful outcome as described previously.Citation9 The present case emphasizes the need to have a suspicion of microsporidial infection even in immunocompetent patients who presents with keratitis after CXL. A careful corneal smear examination confirms the diagnosis and guides further management in such cases.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Pérez-Santonja JJ, Artola A, Javaloy J, Alió JL. Microbial keratitis after corneal collagen crosslinking. J Cataract Refract Surg. 2009;35:1138–1114
- Kymionis GD, Portaliou DM, Bouzoukis DI, et al. Herpetic keratitis with iritis after corneal crosslinking with riboflavin and ultraviolet A for keratoconus. J Cataract Refract Surg. 2007;33:1982–1984
- Rama P, Di Matteo F, Matuska S, et al. Acanthamoeba keratitis with perforation after corneal crosslinking and bandage contact lens use. J Cataract Refract Surg. 2009;35:788–791
- Sharma N, Maharana P, Singh G, Titiyal JS. Pseudomonas keratitis after collagen crosslinking for keratoconus: case report and review of literature. J Cataract Refract Surg. 2010;36:517–520
- Salvador Garcia-Delpech S, Díaz-Llopis M, Udaondo P, Salom D. Fusarium keratitis 3 weeks after healed corneal cross-linking. J Refract Surg. 2010;26:994–995
- Pollhammer M, Cursiefen C. Bacterial keratitis early after corneal crosslinking with riboflavin and ultraviolet-A. J Cataract Refract Surg. 2009;35:588–589
- Zamora KV, Males JJ. Polymicrobial keratitis after a collagen cross-linking procedure with postoperative use of a contact lens: a case report. Cornea. 2009;28:474–476
- Joseph J, Sridhar MS, Murthy S, Sharma S. Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Ophthalmology. 2006;113:531–537. Epub 2006 Feb 17
- Loh RS, Chan CML, Ti S, et al. Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and management. Ophthalmology. 2009;116:2348–2353