Abstract
We report a 37-year-old woman with uveitic phase of Vogt Koyanagi Harada disease and tonic pupil, the tonic pupil persisted after other clinical features of this syndrome had disappeared; neurological evaluation shows absent knee and arm tendon reflexes and positive cholinergic supersensitivity test with Pilocarpine 0.125% confirming the diagnosis of Holmes Adie Syndrome.
A 37-year-old woman arrived with red eye on both sides, which she said started on the left side 15 days prior to her visit; 5 days later, the right eye also presented redness; 2 days after that, she suddenly lost visual acuity in the left eye, which became bilateral 2 days later, on day 9 of development. Upon interrogation, she informed us that she had tinnitus a few days before the eye redness started, but denied having headaches or nuchal rigidity. The patient refused lumbar puncture. The patient also denies any history of use of barbiturates or any other drugs that may cause absence of deep tendon reflexes, previous neurological symptoms, or trauma to the spinal region, as well as electrolytic problems; complete neurological and systemic evaluation was within normal findings.
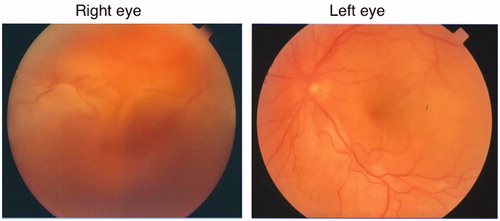
On admission, visual acuity was 20/80 RE and 20/200 LE. Bilateral intraocular pressure (IOP) was 10 mmHg. During anterior segment examination, both eyes revealed mild conjunctival hyperemia, transparent cornea, anterior chamber with cells 2+ and flare1+, and pharmacologically dilated iris. Examination of the posterior segment revealed vitreous opacity and cell 1+, swollen hyperemic optic disk, serous retinal detachment of the area between temporal vascular arcades, and inferior retina with peripapillary folds on both eyes (). Fluorescein angiography revealed areas of delayed choroidal nonperfusion in early frames, early pinpoint hyperfluorescence, disc hyperfluorescence and leakage, and late choroidal hyperfluorescence.
Figure 1. Fundus photographs of both eyes on admission, showing vitreous opacity and serous retinal detachment in right eye, and hyperemic optic disk and serous retinal detachment in left eye.
After a complete blood count (CBC), blood chemistry, and general urine examination came back normal and an HIV ELISA test and VDRL and FTA-Abs tests came back negative, we first decided a diagnosis of VKH was applicable. We initiated treatment with prednisolone acetate 1% q/2 h, tropicamide-phenylephrine TID, prednisone 75 mg po q/day, and a transseptal betamethasone acetate and then injected both eyes with phosphate. After systemic infections were ruled out and after we observed good response to steroids, we began treatment with azatioprine 150 mg/day.
After a month of treatment, visual acuity improved to 20/20 in both eyes, and ocular examination revealed anisocoria with an IOP of 13 mmHg in both eyes. During slit-lamp examination we saw no inflammatory cells in anterior chamber, the retina was attached, and we found a normally colored optic disk. Because of this improvement, topical steroid was gradually tapered off during a 6-week period and was then discontinued. Oral prednisone was also slowly tapered down while tropicamide-phenylephrine was discontinued.
On the fourth month, visual acuity was 20/20 in both eyes, uncorrected near visual acuity at 40 cm was Jaeger J1+ (20/20) RE and Jaeger J3 (20/40) LE, subjective refraction revealed emmetropia, and we didn't find any anterior chamber inflammation. Anisocoria persisted; the right pupil measured 2.8 mm and the left pupil measured 6.7 mm. Pupillary reflexes were preserved intact on RE while vermiform movements with luminous stimulus were present on LE, as well as a very slow response to accommodation and absence of the consensual reflex. Posterior segment examination showed a normal optic disk, sunset glow fundus, and nummular scars on mid-periphery. The general examination revealed alopecia and vitiligo on shoulders and arms.
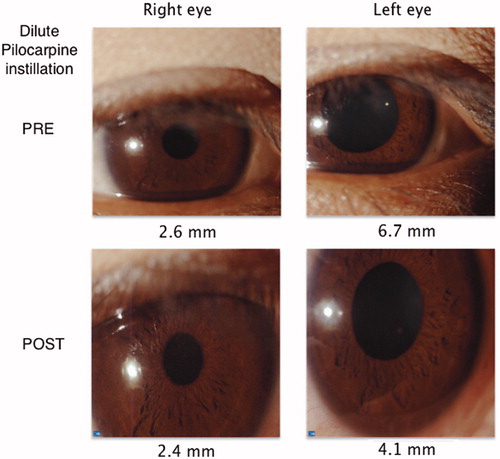
A cholinergic hypersensitivity test with pilocarpine 0.125% came back positive, with contraction of the LE pupil and absence of response on the RE (pre 2.8 RE y 6.7 LE, post 2.7 RE y 4.6 LE) (); also, bilateral lower extremity tendon reflexes were absent. With these findings, we were convinced a diagnosis of Holmes Adie-syndrome was warranted. With the criteria met,Citation1 the diagnosis of complete Vogt-Koyanagi-Harada syndrome was also supported.
Figure 2. Denervation supersensivity test, after thirty minutes of one drop 0.125% pilocarpine, showed left pupil constriction from 6.7 to 4.1 mm.
During her 24-month follow-up, the patient did not present any recurrence; in the posterior segment she presents pigmentary changes compatible with “sunset glow,” typical of VKH. Unilateral pupillary anisocoria persists with difficulty on accommodation and occasional headaches while reading. Alopecia showed improvement.
Vogt-Koyanagi-Harada disease (VKH) is a granulomatous panuveitis that involves the eyes, auditory system, meninges, and skin. This disease occurs more frequently among people with certain genetic predisposition, who also possess greater skin pigmentation as a distinguishing characteristic.Citation2 In 1978, the American Uveitis Society (AUS) revised the diagnostic criteria for VKH, trying to categorize patients according to their clinical manifestations; later, there was a revision resulting from a meeting of the First International Workshop on VKH disease in 1999. According to their proceedings, patients presenting ocular and extraocular manifestations were categorized as having complete or incomplete VKH disease depending on the number of systems involved.Citation1
Within the diagnostic criteria applied to Vogt-Koyanagi-Harada disease, central nervous system manifestations include meningismus and cerebrospinal fluid pleocytosis, which are present in the prodromic phase of the syndrome and may be absent in the uveitic phase due to its transitory nature. The neurological manifestations typically described include headache in 49% of the cases, photophobia 48%, tinnitus 36%, nuchal rigidity 33%, weakness 21%, flu-like symptoms 17%, and nausea in 13% of the cases.Citation3 Other neurologic manifestations have been reported in rare cases and include anterior ischemic optic neuropathy (in the uveitic phase),Citation3 acute myelitis, and tonic pupil.Citation4–6 The latter of these has been reported in 3 cases, 2 of them in females between the third and fourth decades of life (). According to the actualized VKH criteria,Citation1 Brouzas et al. did not report the absence of deep tendon reflexes in a patient with complete VKH syndrome.Citation4 Kim et al. reported a case of complete VKH with normal tendon reflexes,Citation5 while Narang et al. reported a case of probable VKH, where neither mentioned the absence of these reflexes.Citation6
Table 1. Ocular manifestations.
The physiopathological mechanism of the tonic pupil is related to a parasympathetic denervation of the sphincter muscle of the iris,Citation7 which results from damage to the ciliary ganglion; in most cases, the cause of this damage is unknown. After some weeks, post-ganglionic axons of the ciliary body regenerate and make synapsis on an inappropriate manner in the sphincter muscle. This denervation–reinervation is restricted to some segments of the iris, resulting in an asymmetric pupillary response to light and accommodation.Citation8
Clinical characteristics of the tonic pupil are poor reaction to light, near-light pupillary reflex dissociation, tonic miosis and redilatation, segmental sphincter paralysis, and cholinergic hypersensitivity. Diagnosis of tonic pupil is aided by using low-dose cholinergic agents (pilocarpine 0.1%), since denervation increases the number of cholinergic receptors and the affected eye will show an exaggerated miotic response compared to the contralateral healthy eye. This helps clinically to make a differentiation between pupil midriasis for other causes that would not respond to pilocarpine.Citation8
Ocular and orbital causes of tonic pupil include viral ganglionitis, vasospasm migraine, trauma, surgery, and, occasionally, ocular tumors. There have been descriptions of tonic pupil association with connective tissue diseases such as systemic Sjögren syndrome, temporal arteritis, and rheumatoid arthritis, and autoimmune diseases like celiac disease, autoimmune hepatitis, and endometriosis.Citation8 When involvement is bilateral, a generalized peripheral neuropathy or autonomic neuropathy, such as Riley-Day syndrome, diabetes, amyloidosis syndrome, or paraneoplastic syndrome, is suggested.Citation7
Association between VKH and Holmes-Adie syndrome is rare; only 3 cases were reported until March 2013Citation4–6 and all of them presented bilateral affection with normal deep tendon reflexes and, because of this, tonic (Adie’s) pupil diagnosis was reached ().
Table 2. Systemic manifestations.
In 1931, in two different publications, Holmes and Adie described what came to be known as Holmes-Adie syndrome. It is characterized by pupil mydriasis (which usually is unilateral and occasionally evolves to become bilateral), poor pupillary light reflex, accommodation paresis, strong pupillary response to near stimuli, and slow re-dilatation of the pupil after constriction due to near stimuli. This is accompanied by absence of deep tendon reflexes; when the reflexes are normal, it is only called Adie pupil. The possible explanation for the arreflexia in Holmes-Adie syndrome could be a deficit of large spinal somatosensorial afferent fibers and synaptic disorder of the spinal reflex pathways, both of which can be observed in electrophysiological studies.Citation9 Adie pupil is unilateral in 80% of the cases and becomes bilateral at an annual rate of 4%.Citation10 Holmes-Adie syndrome is also related to autonomic dysfunction in 28–40% of the patients presenting with orthostatic hypotension secondary to afferent baroreceptor failure and, rarely, with paroxysmal cough.Citation11 The presence of autoantibodies against sympathetic ganglia cells has also been described for other (non-VKH) autoimmune diseases, like type 1 diabetes mellitus. The initial damage to the nerve probably occurs due to metabolic or microvascular factors and this is what provokes an immune response.Citation12
The association between deep tendon reflexes and VKH has been reported anecdotally in a few cases; Najman et al.Citation13 described 3 patients with neurologic symptoms (mainly, absent deep tendon reflexes), who were diagnosed with Guillain-Barré syndrome and VKH syndrome simultaneously or within 2 weeks after the symptoms first showed up. This could be explained by the common origin in the neural crest of melanocytes and myelin-producing Schwann cells.
To date, there are few reports of association of tonic pupil syndrome in patients with Vogt-Koyanagi-Harada syndrome and there is no clear explanation for this relationship. A possible pathophysiological mechanism, suggested by Kim and coworkers, is that the pupillary tone in these patients may be caused by degeneration at the ciliary ganglion or involvement of short ciliary nerves owing to the diffuse ocular inflammation. This is, presumably, followed by aberrant reinnervation.Citation5 Another possible explanation is the lack of a common pathophysiological mechanism, but just chance of happening at the same time in the same patient since both diseases are more common in one population group (women between 3 and 5 decades of life). This is the first case in which an association of these syndromes (Holmes-Adie syndrome and Vogt-Koyanagi-Harada syndrome) exists.
In conclusion, pupillary reaction abnormalities, though uncommon, could be seen in association VKH syndrome.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Read RW, Holland GN, Rao NA, et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol. 2001;131:647–652
- Moorthy RS, Inomata H, Rao NA. Vogt-Koyanagi-Harada syndrome. Surv Ophthalmol. 1995;39:265–292
- Pan D, Hirose T. Vogt-Koyanagi-Harada syndrome: review of clinical features. Semin Ophthalmol. 2011;26:312–315
- Brouzas D, Chatzoulis D, Galina E, et al. Corneal anesthesia in a case with Vogt-Koyanagi-Harada syndrome. Acta Ophthalmol Scand. 1997;75:464–465
- Kim JS, Yun CH, Moon CS. Bilateral tonic (Adie's) pupils in Vogt-Koyanagi-Harada syndrome. J Neuro-ophthalmol. 2001;21:205–206
- Narang S, Sood S, Malik A. Probable Vogt-Koyanagi-Harada's syndrome associated with tonic pupils. Nepal J Ophthalmol. 2010;2:154–156
- Kawasaki A. Physiology, assessment, and disorders of the pupil. Curr Opin Ophthalmol. 1999;10:394–400
- Moeller JJ, Maxner CE. The dilated pupil: an update. Curr Neurol Neurosci Rep. 2007;7:417–422
- Mak W, Cheung RT. The Holmes-Adie plus syndrome. J Clin Neurosci. 2000;7:452
- Thompson HS. Adie's syndrome: some new observations. Trans Am Ophthalmol Soc. 1977;75:587–626
- Emond D, Lebel M. Orthostatic hypotension and Holmes-Adie syndrome: Usefulness of the Valsalva ratio in the evaluation of baroreceptor dysfunction. J Hum Hypertens. 2002;16:661–662
- Muhr-Becker D, Ziegler AG, Druschky A, et al. Evidence for specific autoimmunity against sympathetic and parasympathetic nervous tissues in type 1 diabetes mellitus and the relation to cardiac autonomic dysfunction. Diabet Med. Jun 1998;15:467–472
- Najman-Vainer J, Levinson RD, Graves MC, et al. An association between Vogt-Koyanagi-Harada disease and Guillain-Barre syndrome. Am J Ophthalmol. 2001;131:615–619
