Abstract
We report a case of an immunocompetent woman with atypical marginal keratitis. She presented with recurrent episodes of multiples microabscess distributed in a triangular pattern associated with stromal oedema and anterior chamber uveitis, affecting both eyes, but not simultaneously. The episodes responded to steroid drops, corneal inflammation was coincidental with a worsening of her blepharitis in the affected eye and S. aureus was isolated from the lids.
Recurrent multiple corneal lesions can be associated with immune-mediated ocular disorders, such as Epstein-Barr virus (EBV) multifocal keratitis,Citation1 archipelago keratitis due to herpes simplex virus (HSV),Citation2 or Thygeson keratitis.Citation3 The differential diagnosis of multiple corneal infiltrates also includes catarrhal staphylococcal marginal keratitis.Citation4 Catarrhal ulcers as well as phlyctenular keratoconjunctivitis are derived from an immune reaction in patients sensitized to staphylococcal antigens. Catarrhal ulcers can be multiple and are typically characterized by a circumferential progression of marginal infiltrates, while corneal phlyctenules typically are one nodule that appears first at the limbus and may latter migrate to clear cornea, with strands of superficial corneal blood vessels following the course of the phyctenule.Citation5 Both are usually a complication of longstanding staphylococcal blepharitis, but it has been suggested that other factors may be necessary for the initiation of the catarrhal ulcers in addition to the existence of S. aureus on the lid margin as an immune abnormality of the ocular surface of the affected eye, or the condition of contact between the cornea and the lid margin.Citation6
A healthy, nonatopic, 47-year-old woman complained of pain and blurred vision in her left eye. Her personal medical history was irrelevant, except for a previous episode of lumbar pain that had been studied by the internal medicine department years ago without etiology. Her right eye (OD) was amblyopic. Data concerning ophthalmological history revealed multiple acute episodes of both eyes over the past 18 years, which had been previously described as acute anterior uveitis, keratouveitis, subepithelial–intrastromal infiltrates, dendriform keratitis, and marginal keratitis. These episodes had been mostly clinically diagnosed and treated as herpetic. She also reported an episode of infectious keratitis in 2006, in which Staphylococcus aureus was isolated from the corneal scrap and a polymerase chain reaction (PCR) showed negative results for HSV, varicella zoster virus (VZV), and cytomegalovirus (CMV) and a left eye episode diagnosed and treated as archipelago keratitis in 2007 ().
Figure 1. (A) Left eye episode diagnosed and treated as archipelago keratitis in 2007, with multiple microabscesses in the supero temporal cornea. (B) December 2009, left eye showing ulcerative blepharitis with superior lid oedema, erythema and erythematous macular lesions on the superior nasal lid skin; conjunctival hyperemia; multiple anterior stromal microabscesses situated on the superior nasal cornea and one infiltrate positioned in the inferior corneal; stromal diffuse infiltration and oedema. (C) November 2012, right eye showed mild conjunctival hyperemia, and 3 anterior stromal infiltrates associated with mild anterior diffuse stromal infiltration. (D) November 2012, her left eye showed superior lid oedema and an erythematous superior nasal lid lesion, meibomitis, and conjunctival injection. The left cornea presented with multiple stromal infiltrates positioned in the supero nasal cornea moving away from the limbus with a convexity border. (E–F) June 2013, right and left eyes showing eyelid margin without inflammation and cornea without scarring or corneal neovascularization (barely perceptible paracentral scarring, on both eyes, detected in 2009, are not seen in the pictures).
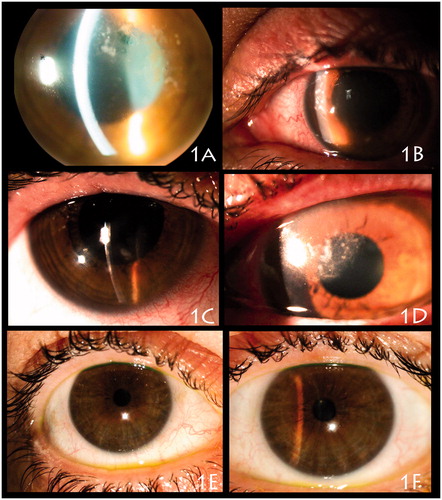
In December 2009, she complained of blurred vision, pain, and photophobia in her left eye. An ophthalmic examination disclosed a visual acuity of 20/60 in the right amblyopic eye and 20/160 in her left eye. The right eye was normal in appearance except for mild meibomitis and a paracentral corneal scar without blood vessels. The left eye showed blepharoconjunctivitis with erythematous popular lesions on the superior nasal skin; multiple anterior stromal microabscesses situated on the periphery of the superior nasal cornea; stromal diffuse infiltration and edema; a paracentral scar; and 2+ grade anterior chamber inflammation (). IOP was bilaterally within normal limits. We performed a multiple PCR from the aqueous humor, which was negative for HSV, VZV, CMV, EBV, and HHV 6. With the suspected diagnosis of herpetic archipelago keratitis, she received treatment with oral famciclovir and 1% prednisolone acetate, which was tapered, and lid hygiene for the blepharitis. The episode resolved after 4 months of treatment without vascular pannus or corneal scarring. The results of a serology test for the herpes simplex virus were negative for IgG and IgM and the results of an enzyme immunoassay (EIA) for syphilis was negative for IgG.
In February 2012, she again complained of pain and photophobia in her OS and an examination showed blepharitis and multiple corneal microabscesses affecting the supero nasal cornea. Culture and sensitivity from a left superior lid culture showed Staphylococcus aureus, sensitive to methicillin and ciprofloxacin. The corneal scrap was negative for bacteria, fungus, and Acanthamoeba, and the corneal multiple PCR was negative for the herpes family virus. We treated the episode with 1% prednisolone acetate for 1 month and 100 mg doxycycline for 5 months and we consulted with the dermatology department, which ruled out acne rosacea.
In November 2012, she presented with pain but this time in her right eye, which showed an acute meibomitis and 3 anterior stromal infiltrates in the inferior cornea (). Two weeks later she also complained of pain in her left eye, which presented with a new episode of multiple stromal infiltrates positioned in the supero nasal cornea and fitted with the eyelid inflammation location (), associated with stromal diffuse infiltration and edema, and also with keratic precipitates and a 2+ grade anterior chamber inflammation. The left corneal scrape was processed for bacterial, fungal, and Acanthamoeba cultures and for the herpes family virus PCR; the aqueous humor was processed for the herpes family virus PCR; all of the results were negative. We treated both eyes with fusidic acid ophthalmic gel for 3 weeks and 1% prednisolone eyedrops with resolution at 5 weeks without sequelae.
The last examination was performed in June 2013 and her visual acuity was 20/60 OD and 20/20 OS, with no new scars from the episodes described above (). The cultures of both superior lids were negative and the Demodex examination on the lashes was negative.
Staphylococcal marginal keratitis has been described as localized peripheral stromal infiltrates that spread paralleling the contour of the limbus. The infiltrates are separated from the limbus and the anterior chamber is typically quiet.Citation7 Often, there are signs of chronic staphylococcal blepharoconjunctivitis.
We believe that our case shares some characteristics with this entity: first, the corneal scrapes were negative and the episodes responded to steroid drops; second, corneal inflammation was coincidental with a worsening of her blepharitis in the affected eye and the location of the keratitis fitted with the location of the lid inflammation; and third, S. aureus was isolated from the lids. Because the keratitis of our patient consisted of multiple stromal inflammatory infiltrates and was associated with stromal edema and anterior chamber reaction, we can perhaps consider our case as an atypical and severe staphylococcal “marginal” keratitis.
Staphylococcal marginal keratitis and phlyctenular keratoconjunctivitis are noninfectious inflammatory processes of the ocular surface that share some similarities and both may be related to blepharitis, but we excluded phlyctenulosis as a possibility because our patient did not presented the typical features of this entity, as nodules, limbus affectation, or vascularizaded scars. On the contrary, archipelago keratitis may be an atypical presentation of herpetic keratitis, which is described as a multiple unilateral keratitis consisting of multiple foci of peripheral ulcers with intense underlying inflammatory infiltrates, positioned in a linear radial pattern, and extending centrally from a limbal lesion.Citation2 This was our first suspicion, but we observed that some of the keratitis episodes, usually the most severe, were coincidental with an acute blepharitis, and this association pointed to staphylococcal marginal keratitis as the cause.
Marginal keratitis affects immunocompetent humans and is the result of enhanced cell-mediated immunity at the limbus to cell wall antigens of the S. aureus located in the eyelids.Citation8 However, there is no clear information regarding which factors contribute to the development of corneal involvement associated with eyelid margin disease. Several studies have tried to identify whether the features of the S. aureus isolated in corneal or lid inflammation differs from the S. aureus isolated in the healthy eye. The staphylococcal enterotoxins, also known as superantigens (SAg), can activate T cells without processing by antigen presenting cells at picomolar concentrations, and have been associated with an increased severity of other immune disorders, such as atopic dermatitis, but SAg are unlikely to play a central role in the development of marginal keratitis.Citation9 S. aureus clonesCitation6 or toxins (alpha-, beta-, delta-lysine) produced by S. aureusCitation10 are also not necessarily important for the initiation of the catarrhal ulcer.
Probably we should focus our attention not only on the microbial antigens that stimulate this delayed-type hypersensitivity reaction, but also on the characteristics of the patient who suffers from the condition. In 2005, Tomo Suzuki found that HLA-A26, HLA-B35, and HLA-DRB1*08 were significantly increased in phlyctenular keratitis related to meibomitis, so some genetic predisposition may underly the different types of ocular surface inflammatory diseases associated with meibomian inflammation.Citation11 In that paper, the therapeutic management of the phlyctenular keratitis was also relevant because by focusing on the treatment of meibomitis with the specific antimicrobial agents for the bacteria isolated and using treatment intravenously in severe cases, the ocular surface inflammation was eradicated. Topical corticosteroids are the mainstay in the treatment of Staphylococcus marginal keratitis and may be use in combination with a broad-spectrum topical antibiotic in cases with epithelial breakdown, with lid hygiene and topical antibiotic for lids to decrease recurrences. Tetracycline causes a significant decrease in the production of lipase and inhibition of growth in S. aureus strains and can be effective in the long-term management of patients with meibomian keratoconjunctivitis.Citation12
This case describes the presentation and course of recurrent multiple stromal keratitis associated with S. aureus blepharitis, with some clinical particularities that have not previously been described.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Gregory R Nettune. Clinical findings in Epstein-Barr viral stromal keratitis: cornea, external diseases. Best poster (320) at the 2010 AAO
- Gabison EE, Alfonsi N, Doan S, et al. Archipelago keratitis: a clinical variant of recurrent herpetic keratitis? Ophthalmology. 2007;114:2000–2005
- Fintelmann RE, Vastine DW, Bloomer MM, et al. Thygeson superficial punctate keratitis and scarring. Cornea. 2012;31:1446–1448
- Thygeson P. Complications of staphylococcic blepharitis. Am J Ophthalmol. 1969;68:446–449
- Mondino BJ. Inflammatory diseases of the peripheral cornea. Ophthalmology. 1988;95:463–472
- Ueta M, Sotozono C, Takahashi J, et al. Examination of Staphylococcus aureus on the ocular surface of patients with catarrhal ulcers. Cornea. 2009;28:780–782
- Mozayeni RM, Lam S. Phlyctenular keratoconjunctivitis and marginal staphylococcal keratitis. In: Krachmer JH, Mannis MJ, Holland EJ, eds. Cornea, Fundamentals, Diagnosis and Management, 2nd ed. London: Elsevier Mosby; 2005:1235–1240
- Ficker L, Seal D, Wright P. Staphylococcal infection and the limbus: study of the cell-mediated immune response. Eye (Lond). 1989;3:190–193
- Jayamanne DG, Dayan M, Jenkins D, et al. The role of staphylococcal superantigens in the pathogenesis of marginal keratitis. Eye (Lond). 1997;11:618–621
- Seal D, Ficker L, Ramakrishnan M, et al. Role of staphylococcal toxin production in blepharitis. Ophthalmology. 1990;97:1684–1688
- Suzuki T, Mitsuishi Y, Sano Y, et al. Phlyctenular keratitis associated with meibomitis in young patients. Am J Ophthalmol. 2005;140:77–82
- Dougherty JM, McCulley JP, Silvany RE, Meyer DR. The role of tetracycline in chronic blepharitis: inhibition of lipase production in staphylococci. Invest Ophthalmol Vis Sci. 1991;32:2970–2975
