Bilateral diffuse uveal melanocytic proliferation (BDUMP) is a rare paraneoplastic disorder characterized by bilateral serous retinal detachment with degeneration of the retinal pigment epithelium (RPE).Citation1 The condition commonly occurs in females with gynecological carcinomaCitation2–7 or males with lung malignancy,Citation8–10 although several other cancer sites have been described.Citation1,Citation11,Citation12 Furthermore, the condition may occur as the first sign of yet undiscovered malignancy.Citation13
Our understanding of BDUMP has increased significantly in the last 5 years. Affected patients have recently been shown to possess cultured melanocyte elongation and proliferation (CMEP) factor in the IgG fraction of the serum,Citation5 explaining the efficacy of plasma exchange in the treatment of the condition.Citation4,Citation9 Furthermore, BDUMP-associated dermal and conjunctival melanocytic proliferations have been shown to have minimal malignant potential.Citation6
Although several authors have reported histological retinal findings in BDUMP,Citation7,Citation9,Citation14,Citation15 these may be complicated by preparation artifact. We present, for the first time to our knowledge, a mini case series of spectral domain optical coherence tomography (OCT) findings in BDUMP.
Case Reports
Case 1
This 48-year-old Caucasian female presented to our Medical Retina Clinic with a 3-month history of bilateral reduced vision. She had been diagnosed with clear cell adenocarcionoma of the ovary 12 months earlier and underwent hysterectomy, bilateral salpingo-oophorectomy, and chemotherapy with carboplatin and paclitaxel. She had been radiologically confirmed as disease-free 6 months earlier. On examination, best-corrected visual acuity (BCVA) was 20/200 right and 20/30 left. There was periorbital skin hyperpigmentation, as well as mild anterior chamber activity and vitritis bilaterally. Dilated fundus examination revealed bilateral inferior exudative retinal detachments (RD) with a shallow detachment at the right macula. Both fundi also demonstrated occasional irregular, pigmented lesions with widespread multifocal patches of well-circumscribed areas of RPE hypopigmentation. The latter lesions showed hyperfluoresecence on fundus fluorescein angiography (FFA) with corresponding hypoautofluorescence. Based on her history, examination and FFA findings, a diagnosis of BDUMP was made, and computed tomography (CT) imaging revealed an asymptomatic recurrence of intra-abdominal metastases.
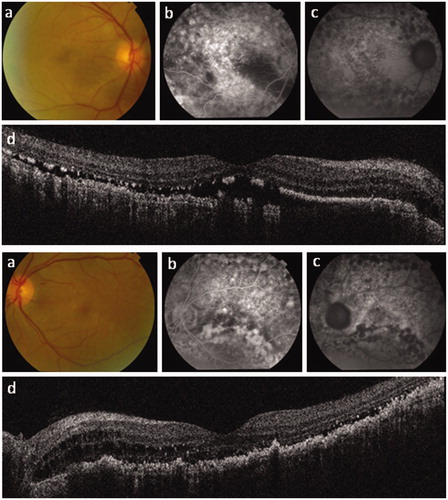
Chemotherapy was restarted with cyclophosphamide and pazopanib. The OCT () revealed widespread disruption of the highly reflective outer retinal bands. The right eye had diffuse shallow subretinal fluid elevating most of the macula. There was also a deposition of abnormal highly reflective material within the subretinal space, which appeared confluent under the papillo-macular bundle but with its resemblance to the “stalactites” seen with chronic separation temporally and loss of the ellipsoid zone explaining the reduction in acuity. Also, there was disruption of the RPE with corresponding hypoautofluorescence temporally and an unusually prominent and easily visualized Bruch's membrane. The presence of uniform autofluorescence signal in the nasal macula supports the OCT finding of relatively well-preserved retinal layers in this region. The left macula showed very shallow subretinal fluid, similar thickening of the RPE, and loss of the ellipsoid zone, but also cystoid degeneration under the papillo-macular bundle. As would be expected, regions of early hyperfluorescence on FFA corresponded to areas of RPE atrophy on OCT.
Figure 1. Right and left eye posterior segment imaging for case 1. (a) Color photography; (b) fundus fluorescein angiography (FFA); (c) autofluorescence imaging; and (d) spectral domain optical coherence tomography (OCT) imaging. Note the patchy retinal pigment epithelium loss on OCT with corresponding hyperfluorescence on FFA and hypoautofluorescence. The right OCT shows loss of the ellipsoid zone, which explains the marked reduction in visual acuity. OCT also reveals shallow serous macular detachments, particularly of the right eye.
Case 2
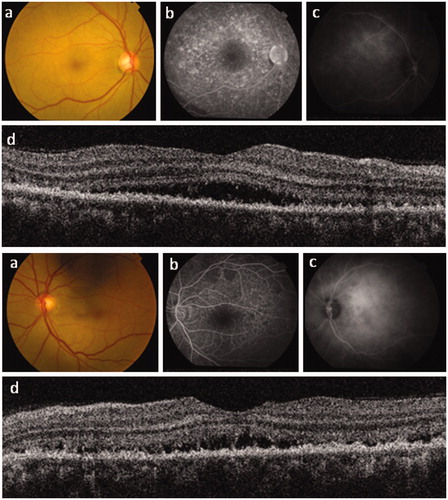
This 50-year-old female presented to our Eye Casualty department with reduced vision in both eyes. She had undergone total abdominal hysterectomy with right ovarian cyst aspirate for menorrhagia 18 months earlier, with subsequent histology revealing FIGO stage 3C1 serous adenocarcinoma of the endometrium with extensive vascular invasion and metastases to the right ovary. Subsequently, she underwent bilateral salpingo-oophorectomy with omentectomy and pelvis and para-aortic lymph node dissection and biopsy, revealing involvement in both regions. Chemotherapy with cisplatin and doxorubicin (cis/dox) was commenced, together with goserelin subsequently. On examination, BCVA was 20/20 right and 20/40 left with inferior exudative retinal detachments bilaterally. CT imaging by her oncologists revealed increasing size of the para-aortic lymph nodes, and she was given a further course of cis/dox chemotherapy. FFA revealed early patchy hyperfluorescence. A clinical diagnosis of BDUMP was made, and OCT examination () revealed bilateral shallow subretinal fluid with disruption of the highly reflective outer retinal bands. While the ELM appeared intact bilaterally, there was a loss of the ellipsoid zone with a more homogenous subretinal thickening replacing the photoreceptor outer segments, and the RPE also seemed to be irregularly thickened, more obviously so on the left side. In contrast to case 1, there is little evidence of RPE atrophy in either eye on OCT, and, as expected, areas of hyperfluorescence on FFA are small and located outside the fovea. Although some outer retinal cystic change was evident in the right retina, this was not seen in the left eye. Despite the absence of enhanced depth imaging on these scans, the choriocapillaris appeared normal. The inner retinal layers were conserved, with normal papillo-macular bundle thickness bilaterally.
Figure 2. Right and left eye posterior segment imaging for case 2. (a) Color photography; (b) fundus fluorescein angiography; (c) indocyanine green fundal angiography; and (d) spectral domain optical coherence tomography (OCT) imaging. OCT reveals diffuse thickening of the retinal pigment epithelium (RPE) with shallow serous macular detachments bilaterally. In contrast to case 1, this patient shows no full-thickness RPE defect, with correspondingly less hyperfluorescence seen on fluorescein angiography and relatively well-preserved visual acuity. The inner retinal layers, including the papillo-macular bundle, are well preserved bilaterally.
Discussion
Patients with BDUMP have been shown to possess anti-retinal antibodies,Citation4 and recently the serum of BDUMP patients has been found to possess an antibody that leads to melanocyte proliferation and elongation.Citation5 In a seminal paper describing 4 patients with BDUMP, Gass outlined 5 cardinal features of the condition: multiple round patches at the level of the RPE, corresponding hyperfluorescent patches on FFA, multiple slightly elevated uveal melanocytic tumours, exudative RD, and rapidly progressing cataracts.Citation15 In 2 of the 4 patients with ocular histology available, note was made of the striking pattern of “pigment epithelial destruction and clumping,” with “extensive destruction of the outer retina despite the relative sparing of the choriocapillaries.” We have confirmed these retinal findings on spectral domain OCT, and have documented varying severity of disease that may be related to the natural history of BDUMP. We have also shown that the inner retinal layers are relatively conserved. Furthermore, our findings add further evidence supporting the theory that BDUMP represents a paraneoplastic condition in which autoantibodies are directed against the RPE. Before making a diagnosis of BDUMP, other conditions causing bilateral serous retinal detachments should be considered, such as Vogt-Koyanagi-Harada disease, choroidal metastases, as well as intraocular lymphoma, among many others. It is hoped this OCT demonstration will help in the early diagnosis of affected patients, which may prove both sight- as well as life-saving.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Mora P, Gonzales S, Crafa P, et al. Peculiar findings in a case of bilateral uveal pigmented lesions. Ocul Immunol Inflamm. 2010;18:379–382
- Bruggemann A, von Bulow M, Finas D, et al. Bilateral diffuse uveal melanocytic proliferation associated with the recurrence of a Bartholin gland carcinoma. Br J Ophthalmol. 2011;95:888–889
- Duong HV, McLean IW, Beahm DE. Bilateral diffuse melanocytic proliferation associated with ovarian carcinoma and metastatic malignant amelanotic melanoma. Am J Ophthalmol. 2006;142:693–695
- Jaben EA, Pulido JS, Pittock S, et al. The potential role of plasma exchange as a treatment for bilateral diffuse uveal melanocytic proliferation: a report of two cases. J Clin Apher. 2011;26:356–361
- Miles SL, Niles RM, Pittock S, et al. A factor found in the IgG fraction of serum of patients with paraneoplastic bilateral diffuse uveal melanocytic proliferation causes proliferation of cultured human melanocytes. Retina. 2012;32:1959–1966
- Pulido JS, Flotte TJ, Raja H, et al. Dermal and conjunctival melanocytic proliferations in diffuse uveal melanocytic proliferation. Eye (Lond). 2013;27:1058--62
- Saito W, Kase S, Yoshida K, et al. Bilateral diffuse uveal melanocytic proliferation in a patient with cancer-associated retinopathy. Am J Ophthalmol. 2005;140:942–945
- Mandelcorn E, McGuire K, Dixon W, Mandelcorn M. Ocular paraneoplastic syndrome: a case of bilateral diffuse uveal melanocytic proliferation. Retina. 2009;29:1375–1376
- Mets RB, Golchet P, Adamus G, et al. Bilateral diffuse uveal melanocytic proliferation with a positive ophthalmoscopic and visual response to plasmapheresis. Arch Ophthalmol. 2011;129:1235–1238
- Sen J, Clewes AR, Quah SA, et al. Presymptomatic diagnosis of bronchogenic carcinoma associated with bilateral diffuse uveal melanocytic proliferation. Clin Exp Ophthalmol. 2006;34:156–158
- De Salvo G, Prakash P, Rennie CA, Lotery AJ. Long-term survival in a case of bilateral diffuse uveal melanocytic proliferation. Eye (Lond). 2011;25:1385–1386
- Ulrich JN, Garg S, Escaravage GK Jr, Meredith TM. Bilateral diffuse uveal melanocytic proliferation presenting as small choroidal melanoma. Case Rep Ophthalmol Med. 2011;2011:740640
- Rahimy E, Coffee RE, McCannel TA. Bilateral Diffuse Uveal Melanocytic Proliferation as a Precursor to Multiple Systemic Malignancies. Semin Ophthalmol. 2013 Oct 14. [Epub ahead of print]
- Barr CC, Zimmerman LE, Curtin VT, Font RL. Bilateral diffuse melanocytic uveal tumors associated with systemic malignant neoplasms: a recently recognized syndrome. Arch Ophthalmol. 1982;100:249–255
- Gass JD, Gieser RG, Wilkinson CP, et al. Bilateral diffuse uveal melanocytic proliferation in patients with occult carcinoma. Arch Ophthalmol. 1990;108:527–533
