To the editor,
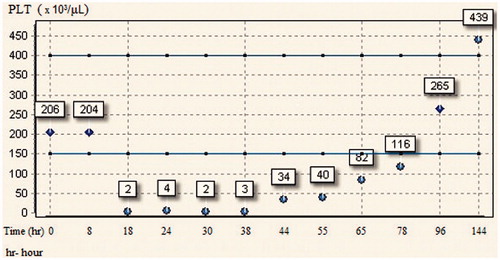
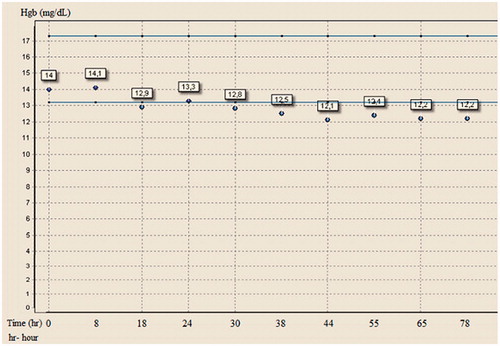
A 40-year-old man without previous medical history presented to the emergency department with chest pain and diagnosed with acute coronary syndrome (ST segment elevation myocardial infarction). After the loading dose of clopidogrel (600 mg) and acetylsalicylic acid (300 mg), he was taken to the catheterization laboratory for urgent coronary angiography. Angiography demonstrated a 95% thrombotic stenosis at proximal portion of the left anterior descending artery (LAD) and plaques in circumflex and right coronary arteries without significant stenosis. Therefore, we decided to primary intervention to LAD lesion and after the bolus dose (10 μg/kg) of intravenous tirofiban baloon angioplasty (Simpass 2 × 15 mm, 12 atm, AlviMedica, Istanbul, Turkey) with stenting (bare metal stent, Ephesus 3 × 18 mm, 12 atm, Medtronic, Minneapolis, MN) was successfully performed. The patient was transferred to the coronary care unit (CCU) and he received i.v. tirofiban infusion (0.1 μg/kg/min). Enoxaparin was also given during this period. During the CCU course, his platelet count fell rapidly from 204 × 103/μL to 2 × 103/μL 18 hours after receiving tirofiban infusion (). There was no significant drop for hemoglobin levels (). Patients peripheral blood smear showed no signs of platelet clumping, ruling out pseudothrombocytopenia. Heparin-induced thrombocytopenia was suspected in the differential diagnosis however enzyme linked immunosorbent assay (ELISA) test for antiheparin/PF4 antibodies was negative. Tirofiban infusion was stopped and the patient was transfused six units of crossmatch-compatible donor platelets with a rise in the platelet count from 2 × 103/μL to 34 × 103/μL during the next 26 hours. Intravenous immunoglobulin (IVIG) could not be given because the patient did not have any active bleeding. Seventy eight hours after the discontinuation of tirofiban infusion his platelet levels increased to 265 × 103/μL (). No bleeding, thrombotic or ischemic events occurred during the hospitalization and the patient was discharged from the hospital after 10 days.
The exact mechanism of thrombocytopenia associated with GP IIb/IIIa receptor inhibitors (abciximab, eptifibatide and tirofiban) is not well known but it is thought to be immune-mediated. Abciximab is associated with a higher incidence of thrombocytopenia than tirofiban and eptifibatide which are reported as 2.4%, 0.5% and 0.2%, respectively. Thrombocytopenia usually develops 24 hours after initial treatment, but may develop up to 10 days later, and the platelet count may return to normal within one to 6 days [Citation1]. The platelet count should be strictly monitored in patients receiving GP IIb/IIIa receptor inhibitors and the treatment should be discontinued when significant thrombocytopenia (<100 × 103/μL) occurs. In a case of thrombocytopenia with active clinical bleeding the patient should be treated with platelet-erythrocyte transfusions. However, for the patients with hematocrit values >25% or hemoglobin levels >7 g/dL blood transfusion should not be applied because it may have negative impact on patients outcome or it may increase the risk of stent thrombosis. But, for hemodynamically unstable patients or hemodynamically stable patients with hemoglobin levels <7 g/dL, there are no restrictions for blood transfusion [Citation2]. IVIG treatment (400 mg/kg/day for 5 days) also can be used in a case of tirofiban-induced thrombocytopenia with active bleeding. As a matter of fact there are tirofiban-induced thrombocytopenia cases that were successfully treated with IVIG therapy [Citation3–5]. It provides a quick recovery in the platelet count just after 20 hours of the treatment [Citation6]. On the other hand IVIG therapy is not indicated in case of abciximab- or ebtifibatide-induced thrombocytopenia because of the drug-dependent antibodies which are thought to be responsible for the platelet destruction at the reticuloendothelial system demonstrated only in patients after tirofiban treatment. Most important part of this issue is how the management procedures should be for the patients with severe thrombocytopenia without significant bleeding. Platelet transfusion should not be given to all thrombocytopenic patients without any significant bleeding because of the stent thrombosis or reinfarction risk. Especially for the patients without active bleeding, platelet transfusion with or without fresh frozen plasma or cryoprecipitate are indicated only for the patients with platelet count lower than 10 × 103/μL [Citation2].
In conclusion, GP IIb/IIIa inhibitor-induced thrombocytopenia should be managed carefully. Because even though the bleeding after thrombocytopenia increases mortality rates of the ACS patients, the treatment of the bleeding with hemostatic agents increases the risk for reinfarction or stent thrombosis.
Declaration of interest
The authors declare that they have no commercial associations or sources of support that might pose a conflict of interest.
References
- Merlini PA, Rossi M, Menozzi A, Buratti S, Brennan DM, Moliterno DJ, Topol EJ, Ardissino D. Thrombocytopenia caused by abciximab or tirofiban and its association with clinical outcome in patients undergoing coronary stenting. Circulation 2004;109:2203–2206
- Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, et al. ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2011;32:2999–3054
- Sanchez GC, Harizi H, Nurden A, Coste P, Jais C, Nurden P. A case of profound and prolonged tirofiban-induced thrombocytopenia and its correction by intravenous immunglobulin G. International society on thrombosis and haemostasis. J Thromb Haemost 2007;5:1068–1070
- Teke HU, Teke D. Profound thrombocytopenia related with tirofiban: Will it be enough to only stop medicine? Platelets 2013;24:335--337
- Bougie DW, Wilker PR, Wuitschick ED, Curtis BR, Malik M, Levine S, Lind RN, Pereira J, Aster RH. Acute thrombocytopenia after treatment with tirofiban or eptifibatide is associated with antibodies specific for ligand-occupied GpIIb/IIIa. Blood 2002;100:2071–2076
- Sakellariou D, Pastromas S, Koulouris S, Manolis A. First report of tirofiban-induced anemia. Tex Heart Inst J 2009;36:55–57