Abstract
Background: Marked ethnic variations in incidence, pathways to care and outcomes have been demonstrated in psychosis. Less research has focused specifically on first-episode psychosis (FEP), particularly adverse contacts such as compulsory detention and hospitalization. This is despite international initiatives to promote equity of care and active early intervention.
Aim: Systematically review current evidence for ethnic variations in rates of compulsory admission and hospitalization in FEP.
Methods: Relevant articles published before December 2012 were identified from PubMed, PSYCInfo, and CINAHL together with manual searching of reference lists. Studies providing quantitative data on compulsory detention rates and/or hospitalization, comparing ethnic groups in FEP, were included and quality rated by independent raters.
Results: All included studies (n = 7) provided data on compulsory detention while fewer (n = 3) focused on admission rates. Three studies reported increased detention in Black and minority ethnic groups, while one reported more hospitalization in White patients. Only two studies covered early intervention services (EIS).
Conclusions: There is a paucity of high quality, well powered studies addressing this important issue, especially in EIS settings. In order to best inform and evaluate fast-developing services, it will be essential to combine large methodologically robust studies with qualitative analysis of patient, carer, and staff experiences.
Introduction
Differences in the experiences of patients from Black or other ethnic minority groups (BME), as compared with native/majority populations, have been well documented in psychosis. Some studies have highlighted the increased incidence of schizophrenia in certain ethnic minorities and with migration (Fearon et al., Citation2006; Kirkbride et al., Citation2012; Leao et al., 2006) while others have identified differences in prognosis, symptomatology, neuroimaging findings, environmental adversity, genetics and substance misuse rates (Fisher et al., Citation2011; Morgan et al., Citation2010b; Velling et al., Citation2007). The complex interplay of these various factors with ethnicity is summarized in a recent review by Morgan et al. (Citation2010a).
Perhaps more controversially, differences in the rates of hospital admission and compulsory detention of BME patients versus the majority population have also been demonstrated, particularly in the United Kingdom (Morgan et al., Citation2005; Singh et al., Citation2007). Considering mental health service users as a whole (beyond first-episode psychosis (FEP)), a systematic review by Bhui et al. (Citation2003) identified differences in pathways to care between ethnic groups. Black patients were noted to have more complex pathways to specialist services, and admissions to hospital were more likely to require home visits compared with South Asian and White patients. The results for continuity of community care were varied, but African Caribbean patients were noted to have more “broken contact” with after-care services. Overall, Black patient groups (particularly African Caribbeans) appeared to show the highest rates of inpatient admission, though in one FEP study the highest rates were noted in White patients (Cole et al., Citation1995). Of those studies measuring compulsory detention, the majority showed Black patients had higher rates of detention than White patients, with less consistent findings for South Asians (Commander et al., 1999; Davies et al., 1996). The meta-analysis by Singh et al. (Citation2007) calculated the odds ratio for compulsory detention in Black patients to be 3.83 times higher than White British patients (and 2.06 times higher in South Asian patients). Findings such as these have implications for service users, providers and policy makers alike – especially when adverse routes to care are associated with poorer outcomes (Singh, Citation2001).
Recent years have seen much interest in early intervention in psychotic illness and, with it, more focus on the specific experiences of those presenting with a FEP. The finding that prolonged duration of untreated psychosis is associated with poorer outcomes (Marshall et al., Citation2005) alongside the concept of a “critical period” during which intervention is more likely to influence prognosis (Birchwood et al., Citation1998), has led to the widespread adoption of the early intervention model, promoting active identification and treatment of psychosis at the earliest stages (McGorry & Killackey, 2002; Singh & Fisher, Citation2007).
It is proposed that adverse contacts, including involuntary admission and possibly hospitalization, can contribute to later alienation from services, stigmatisation and social exclusion. Clinically, negative experiences of coercion and detention at these early stages may predispose the individual to resist intervention, delay future help-seeking and necessitate further coercion (Singh et al., Citation2007). Thus if the ethnic differences in compulsory admissions identified in general cohorts of people with severe mental illness are already present at the first episode, this is an important challenge to early intervention services (EIS).
There have been recent reviews on ethnic differences in “pathways to care” in early psychosis (Anderson et al., Citation2010; Merrit-Davis & Keshavan, Citation2006). The most recent (Anderson et al., Citation2010) did not find consistent results in relation to ethnicity across studies. However, a US study on the way patients are treated during their first hospitalization for psychosis concluded differences during the early stages of treatment between Black and White patients with psychotic disorders were likely to originate in the lead-up to, as opposed to during, their first hospitalization (Sohler et al., Citation2004). Black patients were less likely to have experienced outpatient treatment prior to hospitalization, and were more likely to be admitted for behavioural disturbances, compared with White patients primarily admitted for subjective suffering.
Despite the controversy surrounding use of the Mental Health Act in minority groups and enthusiasm for early intervention in psychosis, there is no existing systematic review of ethnic differences in rates of admission or rates of compulsory detention in patients with FEP. Therefore, we have conducted a systematic review of the international literature on differences in:
rates of hospitalization at first presentation in different ethnic minorities with FEP; and
rates of compulsory detention at first presentation in different ethnic minorities with FEP.
Methods
We undertook a literature search to identify published primary studies comparing ethnic groups for rates of compulsory detention and/or rates of hospitalization in FEP patients.
Definition of terms
By FEP, we referred to patients who present for the first time to mental health services with a psychotic disorder. By hospitalization, we referred to any admission to a residential unit for treatment – public or private facilities. By detention, we hoped to capture any form of compulsory detention, for example under the Mental Health Act in the UK (1983 onwards), and did not specify forensic or civil detentions in our initial search. The definition of ethnicity is of course riddled with complexity, and its use has been challenged as culturally inconsistent (McKenzie, Citation2008). However, we have followed the broad categorizations used by most research papers in the field. A relevant definition of ethnicity is given below: “a collectivity within a larger population having real or putative common ancestry, memories of a shared past, and a cultural focus upon one or more symbolic elements which define the group’s identity, such as kinship, religion, language, shared territory, nationality or physical appearance. Members of an ethnic group are conscious of belonging to an ethnic group”. (Bulmer, Citation1996, p 35).
Search strategy
We searched the following three electronic databases: Medline (1950–2012), PSYCInfo (1899–2012) and the Cumulative Index to Nursing and Allied Health Literature (CINAHL, 1937–2012) for papers published up to and including December 2012. The search terms were divided into four sets: compulsory admission terms (detain*, section*, compulsory, formal, involuntary), ethnic group terms, psychosis terms (psycho*, schizophreni*, bipolar, mania, manic) and admission terms (hospitaliz*, hospitalis*, admi*). Ethnic group terms were kept broad and extended beyond the more well-researched Black African/Caribbean groups to include “BME”, “Asian”, “Maori” and “Surinamese” plus terms such as “race” and “minority”. In addition to the electronic search, reference lists of relevant papers and key reviews were manually scrutinised for further studies. We also searched for grey literature/further research using Google Scholar and contacted experts in the field, as well as authors of the included papers to uncover further relevant studies. We did not restrict studies by year of publication, country of origin or language.
Inclusion criteria
We included observational studies with quantitative reporting of admission/detention rates in psychosis with inclusion of two or more ethnic groups. There were no age restrictions. Titles were initially screened for relevance and their abstracts reviewed. Selected papers were obtained in full text format and scrutinised in further detail. Reasons for rejecting papers were recorded using Reference Manager version 10 (New York, NY).
Studies were subdivided based on whether they gave information on admissions and/or detention. Where possible, statistical data in the form of odds ratios and chi-squared statistics were documented for each study. Where feasible, if odds ratios had not been given in a paper but could be calculated from the raw data presented, this was done. Data were extracted from the papers without formation of a priori hypotheses.
Quality ratings
We assessed quality of the selected studies using a reliable, validated tool for the assessment of epidemiological studies, the Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies Citation2009, available at: http://www.ephpp.ca/tools.html (Thomas et al., 2004). The tool has been evaluated for validity (Deeks et al., Citation2003) and shown good inter-rater reliability (Kappa 0.74). An accompanying dictionary was available to both raters to facilitate use of the tool, accessible online at: http://www.ephpp.ca/index.html.
Two independent raters (FM and HLF) studied each of the seven selected papers in detail and completed the EPHPP tool. The results were then reviewed and any differences discussed. Consensus was in fact reached for all the studies, so intervention from an available third independent rater was not necessary.
Data from all of the studies were extracted and presented in tabular form.
Results
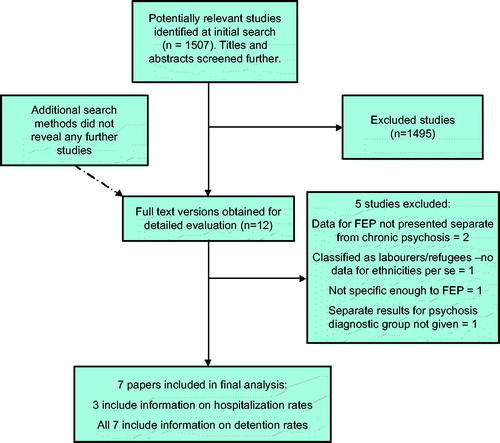
The initial electronic database search revealed 1507 titles (after electronic removal of duplicates between databases), of which only 12 were considered relevant/met the inclusion criteria after reviewing abstracts and summaries (). The other search methods did not reveal any additional studies. Hard copies of these studies were then analysed and five further studies excluded for the reasons presented in . The remaining seven papers were again read in detail and relevant data extracted. Of these, all seven looked at rates of compulsory detention in ethnic minorities versus native/majority populations while only three looked at differences in rates of hospitalization. All studies were in English and publication dates ranged from 1994 to 2010. Only two studies were of populations actively accessing EIS (New Zealand & Canada). With the exception of the Dutch study (based on a national register), all studies covered mainly urban areas with relatively dense ethnic minority populations. Of the UK studies, four were based on London patients, with one also covering a sample of patients from Nottingham (Morgan et al., Citation2005).
The remaining studies were based in New Zealand, Canada and the Netherlands. In keeping with the different ethnic makeup of each of these countries, the groups looked at varied with location of the study. UK studies explored differences between Black African, African Caribbean (collectively termed Black) and White British FEP patients as well as patients classified as “other”. This latter group comprised Southeast Asians and other ethnicities including Turkish people. The study based in New Zealand looked broadly at Maori versus non-Maori patients. The authors report Maori patients are a minority with a tendency to present later to mental health services, and draw parallels with the African Caribbean population of the UK in this regard. The Canadian study included White, Black (African and Caribbean), Asian (Southeast and Chinese) as well as “other” (of which Hispanics made up the largest proportion). In the Dutch national register study, the ethnicities studied were Surinamese, Moroccans, Turkish and Netherlands Antillean.
Quality of papers
summarises the relevant key characteristics of the seven selected papers. The results column reflects results with regard to ethnic differences in compulsory detention rates. Admission results (three papers) are discussed below. A summary of quality and relative strengths and weaknesses is given. The basis for these ratings can be located in the EPHPP tool’s accompanying dictionary. Sample sizes varied greatly between studies, with total numbers ranging from 81 to 462. The numbers of participants from each individual ethnic group fell as low as three (Asian & other group in Cole et al., Citation1995). The ages covered in the studies ranged from 15 to 64.
Table 1. Summary of quality ratings of selected papers and results for ethnic comparisons of compulsory detention.
The majority of studies scored weak to moderate on quality in all areas, with a few exceptions. The Netherlands study (Selten & Sijben, Citation1994) was the only one to score “strong” for selection bias as it was deemed highly representative of the sample population (using a complete national register covering the period of the study) and 100% of ethnicity/detention data was collected. All of the studies followed an observational design, generally not considered to be very strong methodologically using this tool but unavoidable given the subject matter.
None of the included studies conducting regression analysis demonstrate having taken steps to ensure there were enough observations per group, to match the number of potential confounding variables. A recommended “rule of thumb” is to have at least 10 times as many observations as predictor variables, in order to reduce the Type II error risk (discussed in Vittinghoff & McCulloch, Citation2007). One study took steps to blind researchers who were involved in diagnosing patients as psychotic. While it is true this is very difficult to achieve completely in such studies, patients in the study by Goater et al. (Citation1999) were interviewed by one qualified researcher, and the history then presented to another (who made the diagnosis) without revealing the patient’s ethnicity. The diagnosis of psychosis (and therefore decision to include in the study) was thus made with the diagnostician blind to the patient’s ethnicity.
Hospital admission
Only three studies (UK, New Zealand, Canada) assessed variations in hospital admission rates in FEP across ethnic groups. Archie et al.’s Canadian study showed no significant difference in rates of hospitalization in early psychosis in different ethnic minorities versus the White Canadian group (χ2 = 4.349, df = 3, p = 0.226). This was in keeping with Turner et al.’s New Zealand (EIS) study which showed no significant difference in rates of hospitalization in FEP presentations in Maori versus non-Maori service users. Interestingly, the English study by Goater et al. (Citation1999) showed native Whites were six times more likely to be hospitalized at first presentation in FEP, compared with Black people and “others”.
Compulsory detention
summarizes the results with regard to involuntary admission. Five of the seven (71%) studies found no significant difference in rates of compulsory detention. With the exception of Selten et al., all of the studies reported rates of detention as proportions detained from the respective total samples of people presenting with FEP. Two papers (Archie et al., Citation2010; Turner et al., Citation2006) looked at samples of patients presenting to specialist EIS. Selten & Sijben (Citation1994) presented proportions of people admitted from the national population of people with schizophrenia (Dutch National Register) and reported rates of compulsory admission as the number of people detained out of the total number of schizophrenia admissions from each ethnic group.
Selten & Sijben (Citation1994) showed a significantly increased rate of compulsory detention among Surinamese women aged 15 to 34 but not in other groups nor between male patients from different ethnic backgrounds. However, the actual numbers of patients in each ethnic category is again very modest and no correction was made for repeated testing.
The other two studies reporting a significant difference between FEP patients from ethnic groups, compared with White natives, were Morgan et al. (Citation2005) and Archie et al. (2010). Morgan et al.’s UK study was in fact the largest with regard to total sample numbers (smallest ethnic group was “other White” with 33 patients, largest group White British at 237 people) and the strongest with regard to considering confounders. It is reported that African Caribbean men had over 3.5 times the odds of being detained than their White British FEP counterparts, and for Black African patients the odds were over four times. Archie et al.’s smaller Canadian study (n = 200) goes as far as suggesting a significant difference in proportions of ethnic minority FEP patients being detained but does not conduct regression analysis to account for confounders. The highly heterogeneous “Asian” category of patients experienced significantly fewer compulsory detentions compared with all other groups.
Discussion
Our systematic review on comparisons of hospital admission and compulsory detention rates in different ethnic groups of FEP patients has shown there are few studies investigating this relationship, and those that exist are generally not of high quality. This is in keeping with a recent systematic review on pathways to care in FEP (Anderson et al., Citation2010), which called for additional research into the service response to health-seeking behaviours in FEP.
Considering variation in risk of hospitalization at first presentation by ethnicity, only three papers addressed this. It is difficult to draw combined conclusions when the few relevant individual studies showed such marked clinical, statistical and contextual heterogeneity. It is worth noting both studies which showed no significant difference in rates of admission were relatively recent (2006, 2010) whereas the UK paper which reported a difference was (Goater et al., Citation1999) before the Early Intervention model was as widely in place as it is today. Differences in service provision in the different countries, as well as the variation in ethnic mix of the local populations would need to be better understood to put these findings in context. As for Goater et al.’s finding that White patients were six times more likely to be hospitalized, they hypothesized patients from ethnic minorities may be less willing to be admitted to hospital or GPs may miss psychotic symptoms in ethnic minority patients and subsequently delay referral for admission.
There were more data available comparing rates of involuntary admission across ethnic groups. All seven selected studies addressed this question, though again there was marked heterogeneity. None of the studies were rated “strong” in more than one domain. The overall trend is therefore in agreement with the larger, higher quality study by Morgan et al., also the most recent. Although a tentative finding, it sits in contrast to previous theories that ethnic disparities in service experiences develop only after a number of years (Burnett et al., Citation1999; Cole et al., Citation1995). Pooling these studies suggests a disparity exists at the very early stages of contact with services and this will be an important consideration as EIS expand and develop over the coming years. It may be that over the years of illness, the gap between detention rates in BME groups and White patients may widen further (Takei et al., Citation1998) – but the fact it exists at the outset is a source of concern. Excess rates of detention among BME patients has driven service users and politicians to call for change (Merrit-Davis & Keshavan, Citation2006; Singh et al., Citation2007) and a reduction in disproportionate adverse contacts.
Hypotheses on why Black and especially African Caribbean patients in the UK are detained more frequently ranged from differences in symptomatology (Morgan et al., 2010a) with increased paranoia and aggressive behaviour in Blacks through to institutional racism in UK psychiatry. It has also been demonstrated perceived racism in African Caribbeans with psychosis can reduce adherence to medication, as well as increased hospital bed days. Interestingly, a sense of powerlessness to be able to challenge such perceived racism contributed to fewer hospital days and greater adherence, possibly a result of feeling “resigned” to the system (Chakraborty et al., Citation2011). Other potential contributory factors include different attitudes towards services as well as beliefs about mental illness and thus help-seeking. The reality is likely to be multifactorial and complex. A recent UK study focusing on ethnic variations in pathways to acute care and compulsory detention for women in a mental health crisis, suggested the significant ethnic disparities may be partly accounted for by differences between groups in acute help-seeking behaviour (Lawlor et al., Citation2012).
By extending our search beyond the UK, we have been able to identify a small number of papers from abroad addressing these same questions in their respective populations. The Canadian study did not address confounding factors but suggested a reduced detention rate in Asians. Interestingly, this was alongside the finding that Asians were more likely to present to emergency (ER) services. Cultural and attitudinal differences are proposed to account for this but it must be noted the “Asian” group consisted of patients from backgrounds as ethnically diverse as Chinese and Bangladeshi. The Dutch study by Selten & Sijben (Citation1994) was the only one to single out females as being at increased risk of detention (young Surinamese). The authors point out the similarities between The Netherlands Antilleans and African Caribbeans in the UK but do not note a significant difference in detention rates for these patients. This may be to do with the later migration of such patients to the Netherlands – so that many second generation Antilleans had not yet reached the typical age for presentation of psychosis.
Future research
Future studies addressing ethnic disparities in detention/admission will benefit from being larger. Of note, the grouping together of all ethnic minority groups may not be justified. EIS will be well placed to conduct such studies prospectively (Fisher et al., Citation2008) with consideration of a wide range of potential confounders. Additional variables could include duration of untreated psychosis, substance misuse, command of native language and severity of illness. Also an issue is that of the denominator used in compulsory detention studies. The vast majority of papers addressing this question only report differences in the proportion of people sectioned out of those already deemed appropriate for admission; it would be more useful to account for whether there are differences in the FEP population at an earlier stage – such as a difference in the risk of being admitted to hospital in the first instance, and looking at national figures of prevalence in different groups if possible (e.g. Selten & Sijben, Citation1994).
Alongside quantitative observational studies, qualitative work seeking to better understand the narrative of patients and their carers in the early stages of illness, with particular emphasis on experiences of hospitalization and detention should also be conducted.
Limitations
It must be noted there is considerable complexity inherent in any ethnic group-based research. One issue is that of definitions. Cultural, racial, ethnic and migrant groups, for example, are closely related but distinct concepts, though precise definitions may be unclear in studies. Ethnicity should be distinguished from race, the latter of which is based purely on phenotypic differences. Ethnicity is fluid and changeable, and those who perceive themselves as belonging to the same ethnic categories may differ significantly in terms of cultural identity (Morgan et al., Citation2008). Additionally, our search strategy was thorough and broad, but could have been enhanced further through use of a forward citation strategy to potentially identify further relevant papers.
Conclusion
We conclude that despite much debate and interest in the issue, current reports on ethnic variations in admission rates and detention in FEP are conflicting and of moderate to poor quality. Findings from the largest UK study however challenge the hypothesis that disparities in compulsory admission by ethnic group develop only later in the illness, and highlights a need to further investigate the underlying mechanisms driving this difference at the initial contact stages.
Declaration of interest
The authors declare no conflicts of interests. The authors alone are responsible for the content and writing of this article.
References
- Anderson KK, Fuhrer R, Malla A. (2010). The pathways to mental health care of first-episode psychosis patients: A systematic review. Psychol Med, 40, 1585–97
- Archie S, Akhtar-Dinesh N, Norman R, et al. (2010). Ethnic diversity and pathways to care for a first episode of psychosis in Ontario. Schizophrenia Bull, 36, 688–701
- Bhui K, Stansfeld S, Hull S, et al. (2003). Ethnic variations in pathways to and use of specialist mental health services in the UK. Systematic review. Br J Psychiatr, 182, 105–16
- Birchwood M, Todd P, Jackson C. (1998). Early intervention in psychosis: The critical-period hypothesis. Int Clin Psychopharmacol, 13, s31–40
- Bulmer M. (1996). The ethnic group question in the 1991 census of population. In: Ethnicity in the 1991 Census. Office of Population Censuses and Surveys, The Stationery Office, London, Vol. 1: Demographic Characteristics of the Ethnic Minority Populations. UK: Office for National Statistics, 33–62
- Burnett R, Mallet D, Bhugra D, et al. (1999). The first contact of patients with schizophrenia with psychiatric services: Social factors and pathways to care in a multi-ethnic population. Psychol Med, 29, 473–84
- Chakraborty A, King M, Leavey G, McKenzie K. (2011). Perceived racism, medication adherence, and hospital admission in African-Caribbean patients with psychosis in the United Kingdom. Soc Psychiatr Psychiatr Epidemiol, 46, 915–23
- Cole E, Leavey G, King M, Johnson-Sabine E. (1995). Pathways to care for patients with a first episode of psychosis: A comparison of ethnic groups. Br J Psychiatr, 167, 770–6
- Commander M, Cochrane R, Sashidharan S, et al. (1999). Mental healthcare for Asian, White and Black patients with non-affective psychoses: Pathways to psychiatric hospital, in-patient and after-care. Soc Psychiatr Psychiatr Epidemiol, 34, 484–91
- Davies S, Thornicroft G, Leese M, et al. (1996). Ethnic differences in the risk of compulsory psychiatric admissions among representative cases of psychosis in London. Br Med J, 312, 533–7
- Deeks JJ, Dinnes J, D’Amico R, et al. (2003). Evaluating non-randomised intervention studies. Health Technol Assess, 7, 1–187
- Effective Public Health Practice Project (EPHPP) Quality Assessment Tool for Quantitative Studies. (2009). Available from: http://www.ephpp.ca/tools [last accessed December 2011]
- Fearon P, Kirkbride J, Morgan C. (2006). Incidence of schizophrenia and other psychoses in ethnic minority groups: Results from the MRC AESOP study. Psychol Med, 36, 1541–50
- Fisher H, Morgan C, Hutchinson G, et al. (2011). Childhood abuse and psychosis in different ethnic groups: A case-control study. Adv Psychol Res, 85, 173–81
- Fisher H, Theodore K, Power P, et al. (2008). Routine evaluation in first episode of psychosis services: Feasibility and results from the MiData project. Soc Psychiatr Psychiatr Epidemiol, 43, 960–7
- Goater N, King M, Cole E, et al. (1999). Ethnicity and outcome of psychosis. Br J Psychiatr, 175, 34–42
- Kirkbride JB, Errazuriz A, Croudace TJ, et al. (2012). Incidence of schizophrenia and other psychoses in England, 1950–2009: A systematic review and meta-analysis. PLoS One, 7, e31660
- Lawlor C, Johnson S, Cole L, Howard L. (2012). Ethnic variations in pathways to care and compulsory detention for women experiencing a mental health crisis. Int J Soc Psychiatr, 58, 3–15
- Leao T, Sundquist J, Frank L, et al. (2006). Incidence of schizophrenia or other psychoses in first and second-generation immigrants: A national cohort study. J Nerv Mental Dis, 194, 27–33
- Marshall M, Lewis S, Lockwood A, et al. (2005). Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: A systematic review. Arch Gen Psychiatr, 62, 975–83
- McGorry PD, Killackey EJ. (2002). Early intervention in psychosis: A new evidence based paradigm. Epidemiol Psichiatr Soc, 11, 237–47
- McKenzie K. (2008). Improving mental heathcare for ethnic minorities. Adv Psychiatr Treat, 14, 285–91
- Merrit-Davis O, Keshavan M. (2006). Pathways to care for African Americans with early psychosis. Psychiatr Serv, 57, 1043–4
- Morgan C, Charalambides M, Hutchinson G, Murray R. (2010a). Migration, ethnicity, and psychosis: Toward a sociodevelopmental model. Schizophrenia Bull, 36, 655–64
- Morgan C, Mallett R, Hutchinson G, et al. (2005). Pathways to care and ethnicity 1: Sample characteristics and compulsory admissions. Report from the AESOP study. Br J Psychiatr, 186, 281–9
- Morgan C, McKenzie K, Fearon P. (2008). Society and psychosis. Cambridge: Cambridge University Press
- Morgan KD, Dazzan P, Morgan C, et al. (2010b). Differing patterns of brain structural abnormalities between black and white patients with their first episode of psychosis. Psychol Med, 40, 1137–47
- Selten J, Sijben N. (1994). First admission rates for schizophrenia in immigrants to The Netherlands. The Dutch national register. Soc Psychiatr Psychiatr Epidemiol, 29, 71–7
- Singh S. (2001). African-Caribbeans and schizophrenia: A commentary. Adv Psychiatr Treat, 7, 291–3
- Singh SP, Fisher HL. (2007). Early intervention services. Psychiatr, 6, 333–8
- Singh S, Greenwood N, White S, Churchill R. (2007). Ethnicity and the Mental Health Act 1983: Systematic review. Br J Psychiatr, 191, 99–105
- Sohler N, Bromet E, Lavelle J, et al. (2004). Are there racial differences in the way patients with psychotic disorders are treated at their first hospitalization? Psychol Med, 34, 705–18
- Takei N, Persaud R, Woodruff P, Brockington I. (1998). First episode psychosis in Afro-Caribbean and White people. An 18-year follow-up population-based study. Br J Psychiatr, 172, 147–53
- Thomas BH, Ciliska D, Dobbins M, Micucci S. (2004). A process for systematically reviewing the literature: Providing the research evidence for public health nursing interventions. Worldviews Evid Based Nurs, 1, 176–84
- Turner M, Smith-Hamel C, Mulder R. (2006). Pathways to care in a New Zealand first episode psychosis cohort. Austra New Zealand J Psychiatr, 40, 421–8
- Velling W, Selten J, Mackenbach J, Hoek H. (2007). Symptoms at first contact for psychotic disorder: Comparison between native Dutch and ethnic minorities. Schizophrenia Res, 95, 30–8
- Vittinghoff E, McCulloch C. (2007). Relaxing the rule of ten events per variable. Am J Epidemiol, 166, 710–18